ANATOMY AND PHYSIOLOGY OF THE EYE
advertisement

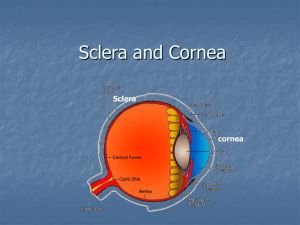
ANATOMY AND PHYSIOLOGY OF THE EYE Kay Ford, C.O.T., C.O.E. VISTAR EYE CENTER Roanoke, VA OUTLINE OF PRESENTATION • • • • • • • • OCULAR ADNEXA LACRIMAL SYSTEM BONY ORBIT ANTERIOR SEGMENT POSTERIOR SEGMENT EXTRAOCULAR MUSCLES VISUAL PATHWAY CONCLUSION AND RESOURCES OCULAR ADNEXA • Eyelids, eyebrows, eyelashes, accessory glands and lacrimal (tear) apparatus. EYELIDS • Primary function is to protect the eye from bright light and foreign objects. • They protect the cornea from drying by blinking to spread the tears over the eye surface, aids flow of tears out of the lacrimal gland, and facilitates the drainage of tears into the nasolacrimal system. • Landmarks are the medial canthus, lateral canthus, the plica semilunaris (third eyelid) and the caruncle. • Eyelids have three layers: 1. Outer layer of skin 2. Middle layer of fibrous tissue and muscle. Within the middle layer of the upper and lower eyelids is a dense, plate-like framework, the tarsus or tarsal plate. Also located in the middle layer is the orbicularis oculi, a circular muscle that closes the eye when it contracts (winking). A second muscle, the levator palpebral superioris, is attached to the upper tarsal plate. 3. Inner layer of tissue called conjunctiva, a thin, translucent mucous membrane that lines the outer front surface of the eyeball, except for the cornea. CONJUNCTIVA • The conjunctiva is an epithelial membrane which covers the anterior sclera and continues to the back surfaces of the lids to form a conjunctival sac. There are three portions of the conjunctiva: 1. Bulbar: covers the white sclera 2. Palpebral: covers the backside of the eyelid 3. Fornix: where bulbar and palpebral meet (loose pocket called the fornix or cul-de-sac). LACRIMAL APPARATUS • The orbital structures that produce tears and the ducts that drain the excess fluid from the front of the eyes into the nose. The lacrimal tears are produced by the lacrimal gland, located under the frontal bone at the upper-outer angle of the orbit. These tears then flow through the six to twelve lacrimal canals or ducts into the conjunctival sac. The tears drain from the sac into the upper and lower punctum (the small holes in the eyelid margins) into the upper and lower canaliculus. The canuliculi take the tears into the lacrimal sac and then into the nasolacrimal duct, then on into the nose. This explains why you need to blow your nose when you cry. EYEBROWS • Each eyebrow is a thickened ridge of skin with short hairs which diverts perspiration from running into the eye. EYELASHES • The eyelashes also protect the eyes. Sebaceous glands at the base of each lash are called glands of Zeis. These glands produce a lubricating fluid. An inflamed gland causes a stye or hordeolum. • Chronic condition called blepharitis is inflammation of the lids. ACCESSORY GLANDS • The accessory glands are the meibomian glands, ciliary glands, and glands of Krause and Wolfring. • Meibomian glands are sebaceous glands which secrete an oily substance onto the lid margins that help prevent the lids from sticking. A blocked meibomian gland results in a chalazion. • The ciliary glands are sweat glands while the glands of Krause and Wolfring are accessory lacrimal glands. BONY ORBIT • The bony orbit provides protection, support and attachment for muscles and the eyeball. • Frontal, ethmoid (the weakest), sphenoid, zygomatic (the strongest), maxilla, lacrimal and palatine (the smallest) • Protect the eyeball from injury. • Many openings to transmit arteries and/or veins and nerves to and from the orbit. • Types of openings are fissures (crevices) and cracks and foramina (holes). • The major openings are the optic foramen, which contains the second (II) cranial nerve (optic nerve , and the supraorbital fissure, which contains the fourth (IV) cranial nerve known as the Trochlear nerve. THREE LAYERS OF THE EYEBALL 1. FIBROUS LAYER This is the outer layer of the eyeball. It has two layers: • CORNEA • SCLERA CORNEA The cornea is a transparent organ without any blood vessels. Its primary function is refraction of light rays. The cornea has a refractive power of about +45.00 diopters. It is composed of 5 layers. **More about the cornea later in this presentation. SCLERA • The sclera is white in color. Its primary function is protection of the eyeball. It connects to the cornea at the area called the limbus and is pierced posteriorly by the optic nerve. It acts as the insertion points for the six extraocular muscles. 2. VASCULAR LAYER • Also known as the uveal tract. This layer functions to supply nutrition to other layers of the eye. It is the middle layer of the eye and is situated between the sclera and retina. It is composed mostly of blood vessels and capillary nets. • The uveal tract has 3 parts: Choroid Ciliary Body Iris CHOROID • The choroid is located posterior to the ciliary body and iris. It is attached firmly at the optic disc and ora serrata. It is the most vascular portion of the vascular layer and is drained by the vortex veins. CILIARY BODY • The ciliary body is located near the base of the iris and posterior to it. It is composes of blood vessels and the ciliary muscle fibers. Its primary function is to alter the shape of the crystalline lens by suspensory ligaments called the zonules of Zinn. It also produces aqueous humor (more on this later). IRIS • The iris is the most anterior portion of the vascular layer. It gives the eye its color (i.e. blue, brown or hazel). • It consists of blood vessels, pigment and muscle tissue. • The hole in the center is called the pupil. • The pupil regulates the amount of light that enters the eye. It is small in bright light (constricted) and large in dim light (dilated). • As we get older, the pupil gets smaller, resulting in the need for more light when reading. 3. NERVE LAYER • The nerve layer is the retina. It is the innermost layer of the eye and is a direct extension of the brain and is normally transparent. The attachments are most firm at the ora serrata and around the optic nerve head (optic disc). When injured, it cannot repair itself. An injured retina, such as a retinal detachment, is best viewed by a dilated fundus exam (DFE). • The retina has 9 layers. RECEPTORS • • The retina is composed of two visual receptors, rods and cones. Cones produce color vision and give improved acuity. Cones are used in day vision under normal and high levels of illumination. Day vision is known as photoptic vision. Rods produce black and white vision. Rods function in dim light or low levels of illumination such as during nighttime. Night vision is known as scotopic vision. LANDMARKS • There are four major landmarks in the retina: 1. 2. 3. 4. Macula Fovea Optic nerve head Ora serrata MACULA • The macula is the optical center of the retina. It appears redder in color when compared to the orange appearance of a the other area of the retina. FOVEA • The fovea is a depression located in the center of the macula. It only has cones and is the area of best vision. OPTIC NERVE HEAD • The optic nerve head is the point of exit of the optic nerve and appears yellow when compared to the orange appearance of the rest of the retina. ORA SERRATA • The ora serrata is the most anterior portion of the retina and is nearly all rods. OCULAR MEDIA • • • • Cornea Aqueous Humor Crystalline Lens Vitreous Humor ANTERIOR CHAMBER • Bordered anteriorly by the cornea and posteriorly by the iris. CORNEA The cornea is a transparent organ without any blood vessels. Its primary function is refraction of light rays. The cornea has a refractive power of about +45.00 diopters. It is composed of 5 layers. CORNEA • The cornea is a transparent organ without any blood vessels. Its primary function is refraction of light rays. The cornea has a refractive power of about +45.00 diopters. It is composed of 5 layers: • • • • • Epithelium Bowman’s Membrane Stroma Descemet’s Membrane Endothelium CORNEAL LAYERS • EPITHELIUM – Outermost layer, about 5 cell layers thick. This layer heals very quickly when injured and does not scar. • BOWMAN’S MEMBRANE – Second layer. Will scar when injured. • STROMA – Middle layer that comprises about 90% of the cornea. • DESCEMET’S MEMBRANE – Serves as barrier for fluids. • ENDOTHELIUM – Innermost layer – one cell layer thick. Cells do not regenerate if injured. POSTERIOR CHAMBER • Bordered anteriorly by the iris and posteriorly by the front face of the vitreous. AQUEOUS CHAMBER It is the space in the eye located between the cornea and the crystalline lens. It is divided into the anterior chamber and the posterior chamber. AQUEOUS HUMOR • The aqueous chambers are fills with aqueous humor, which is manufactured by the ciliary body. The product is clear, colorless and has a watery consistency (99% water). • Aqueous humor’s functions are refraction of light, control of intraocular pressure (IOP), and nourishment of the posterior surface of the cornea and the crystalline lens. It flows from the posterior chamber through the pupil into the anterior chamber. It drains through the angle formed by the cornea and iris to the trabecular meshwork. • The trabecular meshwork is a grate-like structure that leads into the Canal of Schlemm, which is circular and lies under the limbus. Pressure in the eye (IOP) is related to the production and outflow of aqueous humor. • Elevated pressure in the eye (IOP) can cause diseases called glaucoma. There are more than 20 different types of glaucoma. • Glaucoma is associated with elevated pressure, changes in the optic disc, and defects in the visual field and can be blinding. • IOP increases if the angle is blocked, if the flow of aqueous humor is blocked, or if the aqueous input is greater than the output. • Treatment consists of improving outflow or by decreasing the production of aqueous humor by medication and/or surgery. CRYSTALLINE LENS • The crystalline lens is transparent and biconvex. It is composed of a capsule, cortex, and nucleus. • It is about 10 mm in diameter and 5 mm thick. It is suspended from the ciliary body by the zonules of Zinn. It is approximately +12.00 Diopters in power. • Lens primary functions are refraction of light and accommodation (adjusts for near and far vision). • Presbyopia is the loss of accommodation is the loss in flexibility of the lens which happens around age 40 and causes poor close vision. • The lens contains a large amount of protein. Changes in the protein causes the lens to lose transparency. This is called a CATARACT. • The cataract can form in any part of the lens or in multiple locations (nuclear, cortical, anterior or posterior subcapsular or a combination). • Cataract surgery is done to remove the cloudy contents of the lens and is almost always replaced by a man-made intraocular lens, contact lens or aphakic glasses. Aphakia is the absence of a lens. VITREOUS CHAMBER • The vitreous chamber (large cavity of the eye) is filled with gel-like substance located behind the crystalline lens. It is encased by the vitreous membrane and cannot be reproduced. It refracts the light and is the internal support of the eye. • Floaters are spots in your vision usually caused by cellular debris in the vitreous. • Surgery is sometimes required to repair rupture, hemorrhage of leakage of the vitreous. EXTRAOCULAR MUSCLES • The extraocular muscles (EOMs) are organized into an umbrella-like bundle among the orbital fat, orbital blood vessels, and nerves. • Six muscles associated with eye movement: 1. 2. 3. 4. 5. 6. Superior Rectus (SR) Inferior Rectus (IR) Medial Rectus (MR) Lateral Rectus (LR) Superior Oblique (SO) Inferior Oblique (IO) • The muscles are coordinated so that double vision does not occur. • Each eye can rotate on three different axes due to the six muscles. Ocular Motility Alignment • Heterotropia – both eyes do not point in the same direction when both eyes are open. One eye suppresses to eliminate possibility of double vision )diplopia). The eye that is deviated most of the time usually has poorer vision (amblyopia). Terms also used for heterotropia are strabismus, squint, crossed-eye, evil-eye, and wall-eye. If unable to be corrected with noninvasive treatment, surgery is required to realign the muscles involved (recession and/or resection). • Heterophoria – condition where both eyes do not point in the same direction, but only when one eye is covered. Eyes are parallel when both are open. Usually no invasive treatment is required. • Orthophoria – Both eyes point in the same direction when the eyes are open or covered. (This is the normal.) VISUAL PATHWAY • The visual pathway is the path taken by nerve impulses between the eye and the brain when retina is stimulated by light. • The visual pathway has seven structures: the retina, optic nerve, optic chiasm, optic tract, lateral geniculate body, optic radiations, and the visual cortex. • When pathway is intact, the brain interprets what is seen on the retina. • Office procedure of visual field testing will map the normal blind spot, and help to identify, locate and quantify any defect along the visual pathway. Can be used in diagnostic manner to differentiate between eye pathology and source of defect. Reference • Ophthalmic Coding Coach • By the American Academy of Ophthalmic Executives • Available through the American Academy of Ophthalmology and the American Medical Association • ISBN 978-1-61525-274-9 THANK YOU