PLACENTA PERCRETA. PRESENTACION DE CASO
advertisement
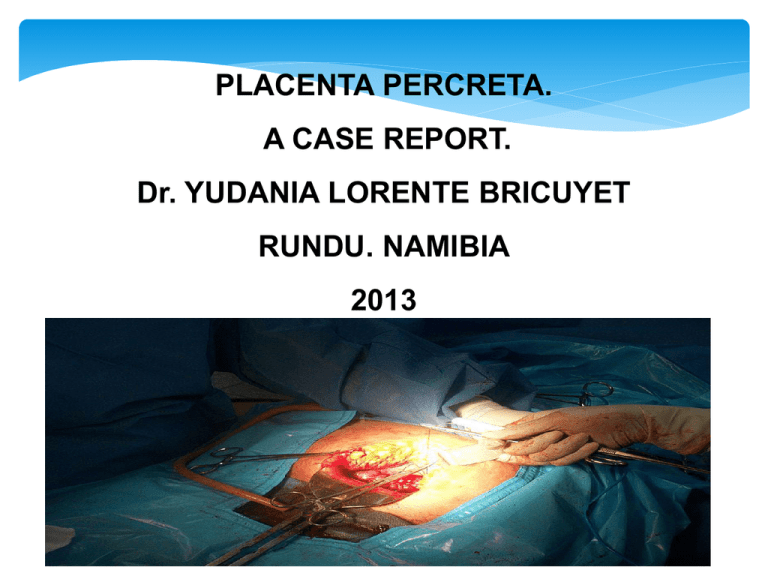
PLACENTA PERCRETA. A CASE REPORT. Dr. YUDANIA LORENTE BRICUYET RUNDU. NAMIBIA 2013 The Placenta: is an organ that develops in the uterus during pregnancy. It is a unique characteristic of the higher mammals. In humans it is a thick mass, about 18 cm in diameter, liberally supplied with blood vessels. It usually weighs about 1 to 2 pounds (about 1/6 of the weight of the baby). The placenta is attached to the uterus, and the fetus is connected to the placenta by the umbilical cord. The placenta draws nourishment and oxygen, which it supplies to the fetus, from the maternal circulation. In turn, the placenta receives the wastes of fetal metabolism and discharges them into the maternal circulation for disposal. It also acts as an endocrine gland, producing estrogen, progesterone, and gonadotropin. Shortly after delivery of the fetus the placenta is forced out by contractions of the uterus. Severe haemorrhage may occur if the placenta does not emerge in its entirety or if the uterus fails to contract properly. A case report. Name: Murunga Angelina 28 years old. Previous obstetric history: G 5 P3 (nvd) A1. LMP: 31/1/2012 EDD:7/11/2012 Risk factors: RVI on HAART and Preeclampsia. This patient came to Rundu Hospital on 26/10/2012 complaint LAP. On examination was found: BP 179/109 mm/Hg. Abd. Cephalic, FHR present and normal, no contractions noticed. Pedal oedema. And in VE. Os was closed, no bleeding per vagina. Was admitted with follow diagnosis: 1) Gestation of 38.3 weeks. 2) Severe preeclampsia. (treated with methyldopa) 3) RVI on HAART. On 27/10/2012 during round, the Dr on call, decided to order labs test ( FBC, U+E, LFT, and Urine analysis) and also to start induction with Misoprostol, BP was normal and general condition of the patient was stable. The patient received 3 doses of Cytotec to tried to induce labour. The BP was controlled. On 28/10/2012 the labs results was received: Hb 10.94 g/dl WCC 5.94x10 l. Platelet 134x10 l. And Creatinine 74 mmol/l. Then the Dr was informed and decided to do Caesarean section due to Severe Preeclampsia with maternal affectation and failed Induction, and informed immediately to specialist for assistance. During surgery ,the anterior wall of the uterus was normal, then the baby was extracted with good Apgar score by classical segment incision, but the placenta was on posterior wall and penetrated through the uterus and some part was attached on the bowels and retroperitoneal tissue. Obstetric Hysterectomy was done and also removed some placenta tissue from de bowels with assistance of de general surgeon. Placenta accreta is a rare but potentially life-threatening complication of pregnancy that is today an increasingly frequent cause of maternal morbidity and mortality. The term refers to any placental implantation that results in its abnormal adherence to the uterine wall. CLASIFICATION The placenta forms an abnormally firm attachment to the uterine wall. There is absence of the decidua basalis and incomplete development of the Nitabuch's layer. There are three forms of placenta accreta, distinguishable by the depth of penetration. 1.Placenta accreta. 2.Placenta increta. 3.Placenta percreta. Pathogenesis Type Description Percent Placenta accreta An invasion of the myometrium which does not penetrate the entire thickness of the muscle. 75-78% Placenta increta Occurs when the placenta further extends into the myometrium, penetrating the muscle. 17% Placenta percreta The worst form of the condition is when the placenta penetrates the entire myometrium to the uterine serosa. This variant can lead to the placenta attaching to other organs such as the rectum or bladder.[9] 5-7% Risk factors 1) Presence of scar tissue: •Asherman’s Syndrome. (D and C) •Myomectomy. •Caesarean section. 2) Trophoblastic invasion. 3) Low lying placenta. 4) Congenital and acquired uterine defects: • Uterine septa. • Leiomyoma. • Cornual pregnancy. 5) Some study suggest that the rate of incidence is higher when the fetus is female. Diagnosis Placenta accreta is very rarely recognised before birth, and is very difficult to diagnose. A Doppler ultrasound can lead to the diagnosis of a suspected accreta and an MRI will give more detail leading to further suspicion of such an abnormal placenta. However, both the ultrasound and the MRI rarely confirm an accreta with certainty. While it can lead to some vaginal bleeding during the third trimester, this is more commonly associated with the factors leading to the condition. In some cases the second trimester can see elevated maternal serum alpha-fetoprotein levels, though this is also an indicator of many other conditions. A three dimensional power color doppler ultrasound scan has been used. Usually in this case, manual blunt dissection or placenta traction is attempted but can cause haemorrhage in accreta. Treatment •HYSTERECTOMY: The safest and most common treatment is a planned caesarean section and abdominal hysterectomy if placenta accreta is diagnosed before birth. In cases where there is invasion of bladder, it is treated in similar manner to abdominal pregnancy and manual placental removal is avoided. However, this may eventually need hysterectomy and/or partial cystectomy. CONSERVATIVE: Pitocin and antibiotics are used for post-surgical management. When there is partially separated placenta with focal accreta, best option is removal of placenta and oversewing the uterine defect. If it is important to save the woman's uterus (for future pregnancies) then resection around the placenta may be successful. Conservative treatment can also be uterus sparing but may not be as successful and has a higher risk of complications. Techniques include: •Leaving the placenta in the uterus and curettage of uterus. Methotrexate has been used in this case. •Intrauterine balloon catheterisation to compress blood vessels. •Embolisation of pelvic vessels. •Internal iliac artery ligation. •Bilateral uterine artery ligation. Complications. 1.Haemorrhage (3000mls-5000mls) 2.Disseminating Intravascular Coagulations (DIC) 3.Transfusion reactions. 4.Other complications accompanying blood transfusion (HIV and Hepatitis) 5.Surgical complications (emergency hysterectomy, bowel injury, urological injuries etc.) 6.Pulmonary embolism. 7.Adult Respiratory Distress Syndrome (ARDS) CONCLUSION Placenta Accreta is a nasty little secret in the world of Obstetrics and Gynaecology. It is fast on the rise, due to the primarily dramatic increase in Caesarean Sections, the majority of which are unnecessary. Any type of uterine surgery increases your risk of developing placenta accreta with subsequent pregnancy, no more than caesarean section. The more caesareans you have, the greater your likelihood of developing placenta accreta. Thank You