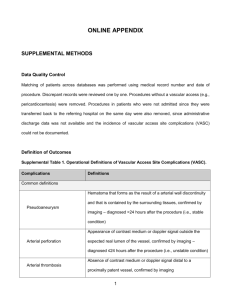
Do we have the answer Semin Vasc Surg 2012:25:108-114
advertisement

For the motion: Endovascular Therapy is a better option for limb salvage in diabetic ulcer treatment Dr. Prasad Jetty Division of Vascular and Endovascular Surgery The Ottawa Hospital University of Ottawa Endo vs open surgery for diabetic ulcers PTA 25% 75% Stenosis Total Occlusion p = 0.053 Stent 37% Stenosis 63% Total Occlusion # 1. Patency • Patency of angioplasty is worse than bypass in diabetic ulcer patients Angioplasty patency is worse! • YES # 1. Patency • BUT ARE BYPASSES THAT GREAT??? • 30-40% of bypasses develop stenoses with in 1 yr (Seminars of Vascular Surgery 2012 25:108-114) • 20-80% of successful patent bypasses have recurrent or persistent ulcers or wounds at 1 yr (Seminars of Vascular Surgery 2012 25:108-114) • Too late or bypass flow is not enough • Non-ischemic ulcer • Occluded bypass does not necessarily mean amputation or recurrent ulcer # 1. Patency • With good surveillance post angioplasty one can identify restenoses early and can easily and safely repeat the endovascular intervention and thus rival the patency rates of bypass procedures # 1. Patency • Are vasculopaths really looking for high 5 and 10 years patencies? • 1 year mortality of patients with CLI is ~25% (American College of Cardiology, Canadian Cardiovascular Society 2005, 2009 updated guidelines) # 1. Patency • Therefore angioplasty may only need to be patent long enough until the patient dies from another cause or at least long enough to allow for ulcer healing, and can easily be repeated if it recurs #2. Periprocedural mortality and morbidity #2. Periprocedural mortality and morbidity • Large prospective NSQIP analysis of >2500 patients revealed bypass has ~20% periprocedural complication rate, and 49% readmission rate at 6 mos (65% are bypass related) • • (LaMuraglia et al. Significant periooperative morbidity accompanies contemporary bypass surgery. Eu J Vasc Endo vasc Surg 2012; 43(5):549-55) Conte et al. Diabetic Revascularization – Do we have the answer Semin Vasc Surg 2012:25:108-114 #2. Periprocedural mortality and morbidity • 10-20% of bypass develop incisional wound complications • metaanalysis 12% decline in ambulation and 15% loss of independent living post bypass surgery • • (LaMuraglia et al. Significant periooperative morbidity accompanies contemporary bypass surgery. Eu J Vasc Endo vasc Surg 2012; 43(5):549-55) Conte et al. Diabetic Revascularization – Do we have the answer Semin Vasc Surg 2012:25:108-114 #2. Periprocedural mortality and morbidity • Complications post angioplasty is ~2% (groin hematomas, pseudoaneurysms) and the patient is discharged the same day) • • (LaMuraglia et al. Significant periooperative morbidity accompanies contemporary bypass surgery. Eu J Vasc Endo vasc Surg 2012; 43(5):549-55) Conte et al. Diabetic Revascularization – Do we have the answer Semin Vasc Surg 2012:25:108-114 #3. Multiple run-off vessels and distal pedal circulation #4. Burning bridges? You will be burning bridges! #4. Burning bridges? • BASIL trial • Concluded that survival is worse in pts who had endo-first failures followed by rescue bypass vs bypass-first pts #4. Burning bridges? • Flawed logic- Selection Bias • Pts who failed angioplasty have selected themselves out as higher risk • Problems with BASIL • Extremely highly selective- only 1/10 patients randomized actually got the procedure they were suppose to get (does not represent the usual vascular population) • Interventional radiologists did the endo procedures vs vascular surgeons • Procedures done 12-14 years ago - OUTDATED!! • There are some good things about BASIL.... #4. Burning bridges? • BASIL is very good in thai food #5. Do all diabetic ulcers with vascular stenoses or occlusions need revascularization? NO Loss of sensation- prone to injury Demyelination and atrophy of intrinsic muscles Disruption of normal bony architecture Resultant abnormal pressure points Impaired immunity and delay in healing Micro vascular ischemia Macro vascular ischemia #5. Not all diabetic ulcers with vascular stenoses or occlusions need revascularization • some will heal with conservative therapy • It is difficult to know exactly who will benefit • Tendancy for vascular specialist to revascularize in the setting of concomittant vascular disease and therefore some patients maybe receiving revascularization when it may not be necessary. #5. Not all diabetic ulcers with vascular stenoses or occlusions need revasculariztion • An unnecessary bypass may be worse than an unnecessary angioplasty Ask Uncle Google… Thank you Division of Vascular and Endovascular surgery The Ottawa Hospital and University of Ottawa Round 1 Rebuttal TASC 2 Classification • Type A: endovascular procedures are recommended • Type B: endovascular procedures are recommended unless an open revascularization procedure (surgery) is required for other lesions in the same anatomic area • Type C: open revascularization procedures are recommended. Endovascular procedures are only recommended in patients who have a low healing potential following surgical revascularization • Type D: endovascular procedures are not recommended as first-line treatment TASC guidelines are lesion-centric and do not emphasize the importance of weighing comorbid factors and life expectancy #6. If you don’t embrace endovascular therapy someone else will • It is crucial that the vascular surgeon embraces endo and leads innovation in the field otherwise we are going towards extinction Evolution