Chirurgiczne leczenie achalazji przełyku
advertisement

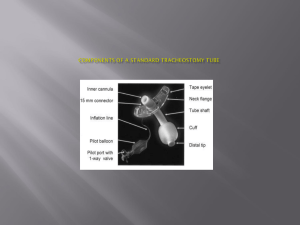
PATHOLOGIES OF THE TRACHEA Department of Thoracic, General and Oncological Surgery Medical University of Lodz Head of the Department: Prof. Marian Brocki Author of the lecture: Edyta Santorek-Strumiłło, MD ETIOLOGY OF TRACHEAL STRICTURES prolonged endotracheal intubation, tracheostomy, 92 % of strictures direct and indirect tracheal injuries, aspiration of a foreign body into the tracheal lumen, tracheal burns, tracheal wall infections, other (sarcoidosis, tuberculosis, histoplasmosis), primary benign and malignant tracheal tumors, malignant infiltration of the trachea. Introduction: • An increasing number of patients treated due to respiratory failure by prolonged endotracheal intubation, mechanical ventilation and tracheostomy causes the increase of a number of airway obturations. • According to different authors the rate of complications of tracheostomy ranges from 2 % to 21%. • There is only a low percentage of tracheal stenoses that are symptomatic and demand surgical treatment. ENDOTRACHEAL INTUBATION Endotracheal intubation is a minimally-invasive procedure. A plastic tube is introduced through the month or nostrils into the tracheal lumen usually under a laryngoscope control and is fixed within the trachea by the inflation of a special balloon. It is a routine medical procedure used, among others, during general anesthesia or resuscitation. COMPLICATIONS OF ENDOTRACHEAL INTUBATION injuries of the lips, teeth, tongue, tonsils, throat, larynx, injury of the vocal cords, injury of the trachea laryngeal edema or spasm after intubation tube removal, acute pulmonary distention or tension pneumothorax infection of the airway, errosions of the tracheal wall caused by an endotracheal tube cuff pressure and chronic ischemia A Fome-Cuf endotracheal tube TRACHEOSTOMY Tracheostomy is one of the most frequent procedure performed in intensive care units, laryngologic and surgical departments as it preserves the patency of the airway and enables effective mechanical ventilation in patients with respiratory failure. INDICATIONS FOR TRACHEOSTOMY : obstruction of the airway control of the secretions mechanical ventilatory support in respiratory failure decrease of dead respiratory space and the treatment for sleep apnea TRACHEOSTOMY in patients that require mechanical ventilation for longer than 14 days tracheostomy should be performed as soon as possible when their general state is stable enough. duration of endotracheal intubation shouldn’t be longer than 7 days and if extubation is not possible within next 5-7 days due to patient’s general state tracheostomy must be done. Relative anatomy TYPES OF TRACHEOSTOMY TUBES CUFLESS TUBES CUFFED TUBES TECHNIQUE A. 3-cm long horizontal skin incision is made 2 cm over the sternal notch . Subhyoid muscles are separated vertically and the pretracheal fascia is exposed. The thyroid isthmus can be divided if it hinders tracheal exposure. TECHNIQUE B. Tracheostomy is usually done below the second tracheal ring. The third ring is elevated with a sharp hook and a disk is excised using a surgical blade No 11. TECHNIQUE C. Any secretion is removed from the airway and a tracheostomy tube is introduced with its low-pressure cuff collapsed. When the tracheostomy tube is already inserted its guiding mandril is removed, surgical wound is sutured and the tube is fastened with tapes around the neck. TECHNIQUE D. In the case of initracheostomy or if tracheostomy is performed due to emergency conditions it is done through the cricothyroid membrane. A small skin incision is made over the membrane and it punctured with a mandril of smaller diameter. The procedure is carried out under local anesthesia. TRACHEOSTOMY COMPLICATIONS OF TRACHEOSTOMY –6% EARLY COMPLICATIONS : LATE COMPLICATIONS : hemorrhage tracheoarterial fistula abscess in tissues tracheoesophageal fistula sourrounding a stomy subcutaneous emphysema postintubation tracheal stricture mediastinal emphysema tracheomalacia dislocation of a tracheostomy persistent tracheocutaneous tube tracheostomy tube obstruction fistula MAIN FACTORS RESPONSIBLE FOR POSTINTUBATION AND POST-TRACHEOSTOMY TRACHEAL STENOSES : compression of an endotracheal tube to tracheal mucosa movements of an endotracheal tube along the tracheal wall bad surgical technique and improper care of tracheostomy prolonged intubation pressure within a cuff over 30 mmHg infections patient’s general state (hypotension, hypoxia). Tracheal stenosis after long-term endotracheal intubation or tracheostomy Incidence: ~31% Site: Cuff level or stoma level Degree of stenosis: 11~25% in 18% patients, 26~50% in 22% patients, >50% in 3.7% patients only 3~20% were symptomatic (stenosis>30%) Symptoms: shortness of breath, inspiratory stridor, expiratory wheeze Tracheal stenosis after long-term endotracheal intubation or tracheostomy diagnosis - chest an neck roentgenograms rigid/flexible bronchoscopy computed tomography spiral computed tomography magnetic resonance imaging spirometry laryngoscopy, fluoroscopy, virtual bronchoscopy on the basis of computed picture analysis EBUS – endobronchial ultrasound. CLASSIFICATION OF TRACHEAL STENOSES : Classical classification : glottic stenosis subglottic stenosis stenosis of the cervical part of the trachea stenosis of the mediastinal part of the trachea McCaffrey’s classification I – subglottic stenosis shorter than 1 cm II – isolated subglottic stenosis longer than 1 cm III – subglottic stenosis without glottis inclusion IV – stenosis including the glottis Cotton’s classification - based on the grade of the tracheal lumen stenosis I - stenosis < 70% II - 70% < stenosis< 90% III - stenosis > 90% IV - complete obstruction of the trachea Tracheal stenosis Web-like subglottic stricture Circumferential subglottic stenosis TREATMENT OF TRACHEAL STENOSES endoscopic dilation of a stricture (mechanical dilators, balloon dilation) completed by laser therapy or argon plasma coagulation. mechanical ablation of granulation through a rigid bronchscope ( forceps, electroresection) endoscopic laser patency restoration (evaporation : CO2 -laser, Nd:YAG laser), T-tube implantation, silicone stents expandable metallic stents tracheal resection with end-to-end anastomosis. Indications for treatment : Endocopic dilation : method of temporary tracheal lumen restoration before final treatment. Used often due to emergency indications. Drawbacks : risk of tracheal perforation, hemorrhage, short-term therapeutic effect. Laser therapy : effective ablation of granulation, membranous strictures and central stenoses shorter than 4 cm with preserved partial lumen patency. Enables dilation of the stricture and airway splinting. The method is ineffective in a case of complete tracheal obstruction. Drawbacks : risk of tracheal perforation, intensification of stenosis, arrythmia, air embolism, risk of ignition of a fiberoptic bronchoscope and an intubation tube. Indications for treatment : Argon plasma coagulation : enables relatively safe repeatable ablation of granulation during endoscopy (the depth of coagulation is 0.5-3 mm) In some cases it gives permanent restoration of the tracheal lumen in other cases it makes it possible to prepare a patient to a radical treatment (resection, stent implantation) Drawbacks : method ineffective in complete tracheal obstruction and strictures longer than 1 cm. Indications for treatment : Stent implantation : high efficient, simple technique offering instant improvement of respiratory function. It is usually used in patients in whom surgery is contraindicated or a temporary protection of the tracheal lumen patency is necessary before surgical treatment. Drawbacks: granulation formation, retention of secretion, hemorrhage, stent migration to the lower part of the trachea, stent rupture, intolerance of stent, stent erosion into adjacent organs. Tracheal resection INDICATIONS : Tracheal resection is presumed to be the most effective method for the treatment of tracheal stenoses as it enables the elimination of the stricture and restoration of a physiologic airway state. The method gives good results in patients with benign isolated tracheal stenoses not longer than 4 cm- maximally 6 cm and low surgical risk. CONTRAINDICATIONS : stenosis > 50% of the tracheal length multilevel stenosis high stenosis (glottic or subglottic) recurrence of stenosis after tracheal resection bad patient’s general state TRACHEAL RESECTION Complications : Early : laryngeal and tracheal mucosa edema pneumothorax mediastinitis disturbances of phonation, dysphagia, hemorrhage, surgical wound infection Late : formation of granuloma in the line of anastomosis, recurrence of stenosis, retension of secretion in the bronchial tree, tracheoesophageal fistula, tracheoarterial fistula. NEOPLASTIC STENOSES OF THE TRACHEA Etiology of neoplastic tracheal stenosis : adenomas, carcinomas (primary tracheal carcinomas are extremely rare) papillomas, polyps, lipomas, chondromas, malignant tumors of adjacent tissues infiltrating the trachea (esophageal tumors, thyroid tumors, mediastinal tumors ) NEOPLASTIC STENOSES OF THE TRACHEA Symptoms and signs of neoplastic tracheal stenoses are similar to those observed in postintubation strictures. A basic sign is an increasing dyspnea. Hemoptysis and retrosternal pains are observed more frequently in neoplastic than in postintubation stenoses. DIAGNOSIS OF TRACHEAL TUMORS: laryngoscopy tracheal endoscopy and endoscopic biopsy x-ray examination computed tomography magnetic resonance imaging NEOPLASTIC STENOSES OF THE TRACHEA TREATMENT: endoscopic resection of benign tumors endoscopic resection of a benign tumor + ablation of residual tumor tissues with argon plasma coagulation partial tracheal resection for benign and selected malignant tumors (subglottic tumors, tumors invading adjacent tissues and tumors involving more than 4 cm of the tracheal length are unsuitable for resection as oncological margins can’t be achieved) palliative methods for the restoration of the tracheal lumen in inoperable tumors (laser, argon plasma coagulation, expandable stents, T-tube) resection of larger than 6 cm of the trachea with the implantation of a prosthesis RECAPITULATION : The resection of the cervical part of the trachea for postintubation stenosis is a safe procedure if a patient is qualified properly for this method of treatment. It means that his or her general state, the localization and length of the stenosis meet the conditions for resection. To perform the procedure successfully, apart from its technical aspects, an experienced anesthesiologist having necessary equipment to provide effective patient ventilation during the operation and good postoperative care is an indispensable condition.