Presentation
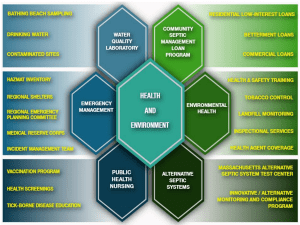
advertisement

Ideal MAP for resuscitation A moving target Prof. Jean-Louis TEBOUL Medical ICU Bicetre hospital University Paris-South France Questions 1- Why do we use vasopressors in septic shock? 2- Which first-line agent? 3- When to start? 4- Which therapeutic target? Questions 1- Why do we use vasopressors in septic shock? 2- Which first-line agent? 3- When to start? 4- Which therapeutic target? Why do we use vasopressors in septic shock? Septic shock is characterized by a decreased vascular tone (inducible NO synthase activation, etc) Hypotension Hypoperfusion worsening Autoregulation of organ blood flow organ blood flow mean arterial pressure Why do we use vasopressors in septic shock? 1- Septic shock is characterized by a decreased vascular tone (inducible NO synthase activation, etc) 2- Profound hypotension worsens organ hypoperfusion …… and represents an independent risk of death 48 hrs 65 mmHg Why do we use vasopressors in septic shock? 1- Septic shock is characterized by a decreased vascular tone (inducible NO synthase activation, etc) 2- Profound hypotension worsens organ hypoperfusion …… and represents an independent risk of death 3- Correction of hypotension with a vasopressor allows improving organ perfusion Probable “arterial pressure” effect Urine flow (ml/h) Creatinine clearance 60 * * * (meq/l) * * 30 baseline 4 hrs 54 73 72 mmHg mmHg mmHg Blood lactate 8 hrs 0-2 hrs 54 mmHg 4-6 hrs 72 mmHg while cardiac output did not change baseline 4 hrs 8 hrs 54 73 72 mmHg mmHg mmHg Autoregulation of renal blood flow renal blood flow 54 72 mean arterial pressure Why do we use vasopressors in septic shock? 1- Septic shock is characterized by a decreased vascular tone (inducible NO synthase activation, etc) 2- Profound hypotension worsens organ hypoperfusion …… and represents an independent risk of death 3- Correction of hypotension with a vasopressor allows improving organ perfusion and microcirculation % StO2 95 90 85 80 StO2: 75 ± 9% 75 p < 0.05 70 65 healthy volunteers 60 82 ± 4 * 55 before NE with NE NIRS technology Vascular Occlusion Test StO2 (%) Inflation of the pneumatic cuff Deflation of the pneumatic cuff AUC 90 Start point : 80 70 60 End point : 0.85 x baseline StO2 0.98 x baseline StO2 Recovery slope Desaturation slope Index of recruitment of microvessels 50 Start point : 1.05 x minimal StO2 40 Occlusion time Time (%/s) 3.5 3.0 StO2 recovery slope Restoration of a “good” MAP with early introduction of NE 2.5 2.0 resulted in recruitment 0.05 1.5 of microvessels and better tissuep <oxygenation 1.0 0.5 0.0 before NE with NE Questions 1- Why do we use vasopressors in septic shock? 2- Which first-line agent? 3- When to start? 4- Which therapeutic target? Questions 1- Why do we use vasopressors in septic shock? 2- Which first-line agent? 3- When to start? 4- Which therapeutic target? 140 140 SAP 120 100 80 100 MAP DAP 20 80 60 60 40 120 reflects the vascular tone vasodilatation 40 20 low DAP Consider vasopressors When to start vasopressors? • when MAP is < 65 mmHg despite “adequate” fluid resuscitation • or when MAP is < 65 mmHg and DAP is low even if the patient has not been yet fully fluid resuscitated Questions 1- Why do we use vasopressors in septic shock? 2- Which first-line agent? 3- When to start? 4- Which therapeutic target? Autoregulation of organ blood flow organ blood flow ? 65 mmHg? mean arterial pressure MAP: 65 mmHg MAP: 75 mmHg MAP: 85 mmHg % 150 100 13 50 urine output capillary flow red cell velocity tonometry PCO2 gap Autoregulation of organ blood flow organ blood flow 65 75 85 Mean Arterial Pressure (mmHg) Crit Care Med 2000; 28:2729-2732 Crit Care Med 2005; 33:780 –786 increasing MAP above 65 mmHg results in little benefit 48 hrs 65 mmHg Crit Care Med 2000; 28:2729-2732 Crit Care Med 2005; 33:780 –786 MAP target value: 65 mmHg Probably higher target value if: • History of chronic hypertension 10 patients none with history of severe hypertension MAP: 65 mmHg MAP: 75 mmHg MAP: 85 mmHg % 150 100 13 50 urine output capillary flow red cell velocity tonometry PCO2 gap Organ Blood flow no prior hypertension with prior hypertension 65 Mean arterial pressure mmHg pts with chronic hypertension pts with no chronic hypertension Probably higher target value if: • History of chronic hypertension • High CVP Probably higher target value if: • History of chronic hypertension • High CVP • Increased abdominal pressure Is it dangerous to target a MAP value up to “normal values” (around 85 mmHg) in septic shock? 13 pts with septic shock * Recovery slope %/min * 65 75 MAP 85 mmHg 65 6 pts with septic shock Perfused Vessel Density No worsening but improvement of microcirculation for MAP target up to 85 mmHg with NE Microvascular Flow Index 20 pts with septic shock Highly variable response among patients 20 pts with septic shock Perfused capillary density improved in pts with an altered sublingual perfusion at baseline, and decreased in patients with preserved basal microvascular perfusion. Conclusion 1- Why do we use vasopressors in septic shock? 2- Which first-line agent? 3- When to start? 4- Which therapeutic target? at least 65 mmHg probably higher value if: • History of chronic hypertension • High CVP • Increased abdominal pressure 65-85 mmHg seems to be a safe range Thank you