pulmoed
advertisement
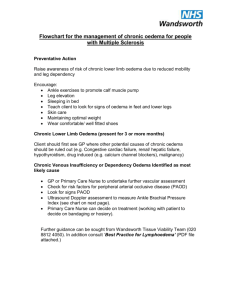
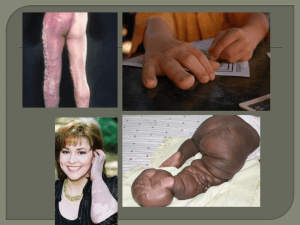
Pulmonary Oedema What is Pulmonary Oedema? • Abnormal accumulation of fluid within the lung tissue – The excess fluid may collect in different parts of the lung according to the severity of the condition and the cause Upper lobe pulmonary venous blood diversion • This can be an early sign of pulmonary oedema • Normally, the upper lobe pulmonary veins are smaller than the lower lobe veins • In elevated left heart pressures, these upper lobe veins become engorged with blood Normal Upper lobe diversion Note how the upper lobe pulmonary veins are so small, they are hardly seen The upper lobe pulmonary veins are dilated (upper lobe diversion) Sequence of Pulmonary Oedema 1 • The first part of the lung to become involved is the interstitial space. – Fluid first builds up in the lymphatic spaces and in the bronchial walls – These structures are normally not large enough to be visible on a CXR, but in pulmonary oedema, the fluid accumulation is so great that they can be seen. At this stage, the normal sharp margin of the central vascular structures is lost, and thickened bronchial walls can be seen Abnormal thickened bronchi – look like polo mints (“peribronchial cuffing”) Vascular contours not as clearly defined as normal, due to fluid in lymphatic tissue (“perihilar haze”) Sequence of Pulmonary Oedema 2 • As the fluid build-up continues, the septae between small units of lung tissue (pulmonary lobules) also become engorged with fluid. • This is particularly noticeable in the lower lateral parts of the lung and small lines parallel to the chest wall become visible – Kerley B lines. Kerley B lines in a patient with interstitial pulmonary oedema. Fluid may also collect in the fissures (not shown). Sequence of Pulmonary Oedema 3 • Once the interstitial space becomes saturated, the fluid then accumulates in the pleural space (pleural effusions). • Eventually, fluid gathers within the alveolar space – alveolar oedema. This can be in a perihilar (“bat wing”) distribution or throughout the lungs. This is “Bat wing” pulmonary oedema. There is perihilar consolidation with relative sparing of the extreme apex and base What causes Pulmonary Oedema? • There are many causes! • Three important causes include: – Left heart failure – Valvular Heart Disease – Hypoalbuminaemia Pitfalls in Diagnosing Pulmonary Oedema on CXR • Severe alveolar pulmonary oedema can look identical to adult respiratory distress syndrome, pulmonary haemorrhage and extensive pneumonia. • Interstitial pulmonary oedema can also look similar to other conditions. • Upper lobe pulmonary venous blood diversion alone is not pulmonary oedema – it just reflects increased left heart pressures. Always treat the patient – not the chest X-Ray Take Home Points • The CXR is a useful tool in confirming suspected pulmonary oedema • The pattern of CXR abnormality depends on the anatomical location of the oedema • The CXR is not a substitute for clinical examination and should be used with other information (e.g. ECG)