232.
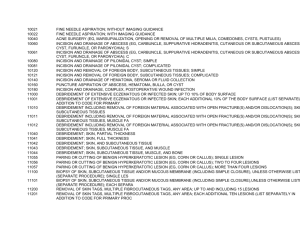
advertisement
Common Office Procedures Baby Health Service Lexington, KY Spalding University Louisville, KY Delwin B. Jacoby, DNP, APRN Delwin B. Jacoby, MSN, APRN has no financial interest or affiliations with any entities regarding this content – April 17, 2013 Objectives for Common Office Procedures Review AHA recommendations for antibiotic prophylaxis for common office procedures. Demonstrate removal procedures for veruccae and acrochordons. Discuss management of subungual hematomas. Develop a plan for the management of ingrown toenails. Demonstrate correct procedure for a digital nerve block in both hands and feet. Perform incision and drainage of an uncomplicated abscess and paronychia. Demonstrate procedures to biopsy suspicious lesions– shave biopsy, punch biopsy, and elliptical excision. Overview of Simple Office Procedures Can be performed in most any office Requires the following: good light source exam table mayo stand/table basic instruments and equipment protective gear anesthesia suture material Basic Instruments & Equipment Scalpels, scissors, punches Forceps Undermining scissors Hemostats Needle holders Syringes and needles Cotton swabs Liquid nitrogen/cryo Gauze pads Suture material English Nail Anvil * Universal Precautions & Sterile Technique Antibiotic Prophylaxis April 2007 - New AHA guidelines for antibiotic prophylaxis – Prosthetic cardiac valve – Previous infective endocarditis – Congenital heart disease only in the following categories: Unrepaired cyanotic congenital heart disease, including those with palliative shunts and conduits Completely repaired congenital heart disease with prosthetic material or device, whether placed by surgery or catheter intervention, during the first six months after the procedure* Repaired congenital heart disease with residual defects at the site or adjacent to the site of a prosthetic patch or prosthetic device (which inhibit endothelialization) – Cardiac transplantation recipients with cardiac valvular disease Acrochordons (Skin Tags) • Commonly found on neck, axilla, bra-line, groin • Topical Anesthesia +/• EMLA • Cetacaine spray • Grasp tag with forceps and snip base with sharp scissors • Apply pressure for hemostasis and dress • Review S & S of infection • No follow-up needed • Few complications Acrochordons (Skin Tags) CPT - 11200 - Removal any method of up to 15 tags any area CPT – 11201 – Removal of each additional 10 lesions. Warts Common, generally benign condition of viral etiology Challenging!!!! Commonly spread by auto-inoculation Cosmetically unappealing Often resolve spontaneously Tend to be recurrent no matter the treatment option Occur most commonly in children Types of Warts (Verrucae) Verruca vulgaris – common warts Periungual warts – occur around nails Verruca planus – flat warts Verruca plantaris – plantar warts Condylomata acuminata Warts Epidermal overgrowths caused by HPV. Spread by direct contact. HPV type 1,2,4 – Assoc with Plantar Warts (verruca plantaris) HPV type 3 &10 – assoc with Flat Warts (verruca planus) HPV type 16,18,31 assoc with genital warts – assoc with genital cancers (condylomata accuminata). HPV 2,4,7,27,29 – Assoc with common warts (verruca vulgaris) Verrucae Common Treatments for Warts Chemical Destruction – Salicylic Acid – Podophyllin/Podophylloxin – Trichloracetic acid – Bichloracetic acid – Others Immune system modulator – Imiquimod (Aldara) Cryotherapy – Liquid nitrogen Duct Tape?!?! Cryotherapy Application of extreme cold to destroy lesions Easy to use Quick Generally good results with little scarring No local anesthesia needed/pain tolerable Multiple lesions can be treated Cryotherapy - Disadvantages Initial cost and set-up Postoperative pain Lesion recurrence Hypopigmentation may occur Repeat visits common Occasional scarring Cryotherapy - Precautions Previous Rx to cryotherapy Do not use on suspected cancerous lesions Caution around nails and nailbed Do not use on eyelids, elbow, digits - relative contraindication Nose, ears, lips, ant. tibial area - caution Dark skin Vascular compromise Immunocompromised patients Cryosurgical Systems Liquid nitrogen - 196 degrees C Verruca-Freeze (chemical refrigerant) - 70 degrees C Histofreezer (chemical refrigerant) - 55 degrees C Cryosurgery Cryosurgical Products Cryosurgery Techniques CPT - 17000 – Destruction benign or premalignant lesion by any method, first lesion. CPT – 17003 - Destruction benign or premalignant lesion by any method, 2nd – 14th lesion. Cryotherapy - Veruccae Nail Anatomy Subungual Hematoma Painful accumulation of blood under the nail secondary to trauma Evacuation relieves pain > 50% of nail bed involvement suggests sig. laceration and possible fracture. Assess neurovascular function prior to procedure Patient education and expectations are very important Subungual Hematoma Evacuation CPT – 11740 –Evacuation of subungual hematoma Ingrown Toenail (Onychocryptosis) Common Leads to pain/ disability Etiology - ill-fitting shoes, improper toenail cutting, trauma. Ingrown toenail spicule leads to inflammatory response Stages of Ingrown Toenails Stage 1 - erythema, pain, swelling Stage II – erythema, pain, swelling, suppuration Stage III – granulation tissue, hypertrophy along with stage II characteristics Ingrown Toenail (Onychocryptosis) Ingrown Toenail Management Stage 1 – Conservative management Stage 2 – Partial toenail removal Stage 3 – Partial toenail removal; Consider referral to Podiatrist Partial Nail Removal Soak in warm H20 prior to procedure Digital nerve block bilaterally with plain 2% xylocaine or bupivacaine (marcaine) 0.25% Prep area with betadine Elevate the nail edge with hemostats or nail elevator Partial nail removal 2-3 mm with nail splitter or sharp scissors Partial Nail Removal (Cont.) Remove the wedged section by rotating the separated portion toward the healthy nail Apply phenol solution (88%) to the nail matrix Apply topical antibiotic and dressing Dispense wound care instructions Recheck as needed, observe for signs of infection Prevention instructions Ingrown Toenail - Partial Nail Removal English Nail Anvil Ingrown Toenail - Partial Nail Removal CPT – 11730 – Avulsion of nail plate, partial or complete, simple; single Digital Nerve Block Digital Nerve Block ***No CPT exists for digital nerve block; Service included in procedure performed. Abscess Incision and Drainage of Abscess Abscess – local collection of purulent materiel in a cavity surrounded by inflamed tissue. – produces pain, pressure and tissue damage. Furuncle (boil) – Starts in hair follicle or sweat gland Carbuncle – furuncle extends to subcutaneous tissue Acute paronychia – abscess around nail Bacteria involved – Mostly S. aureus and other gram+ organisms, MRSA common !! Skin Tension Lines Indications for I & D of Abscess An abscess must be drained in order to heal Systemic antibiotics cannot penetrate the abscess Check to see if the lesion is “fluctuant” All skin abscesses, furuncle/carbuncle, inflamed epithelial cysts, paronychia with abscess must have I & D for resolution Contraindications/Caution Facial abscess - CN VII Caution in area around vital structures such as the eye and neck Caution in areas overlying nerves and blood vessels Instruments Needed Surgical Blades I & D Procedure Determine skin tension lines to minimize scarring Prep skin with antibacterial agent Inject local anesthesia Make a 90 degree stab incision with #11 scalpel blade Apply pressure to expel purulent material If no purulent material, reassess and try again Break up loculations with swab, hemostat or curette +/- Pack with nu-gauze * Apply dressing I&D Procedure CPT – 10060 - I & D of single or simple abscess I & D Follow-up/Patient Education Quick shower and change outer dressing Expect additional drainage Return visit 1-2 days Management options at revisit – Remove packing and repack – Remove packing completely – Partially remove packing Follow-up as needed for resolution Warm H2O soaks? Complete healing takes 7-21 days or longer Fingernail/Toenail Paronychia Infection of the nail fold. Usually S. aureus if acute; may be Candida albicans if chronic (>6 weeks). Toenail paronychia often associated with ingrown toenail and requires partial toenail removal. Usually no anesthetic needed. May use ethyl chloride as local anesthesia Insert #11 blade into area of fluctuance Apply pressure and drain Warm H20 soaks until resolved Draining Paronychia CPT – 10060 – I & D of single or simple abscess Punch Biopsy Fast and easy procedure to obtain a full thickness specimen for pathology. Indicated for unknown and malignant lesions. Great for diagnostic purposes for flat lesions. Useful to remove small, flat nevi. Usually good cosmetic results Useful to diagnose inflammatory disease Indications for Punch Biopsy Diagnosis – Inflammatory skin disease – Skin cancer Removal – Small nevi – Dermatofibromas challenging/often better to not remove Contraindications of Punch Biopsy Less than optimal biopsy technique for SCC and BCC Must Know Anatomy!!!!!!!!!!!!!! – Facial nerve – Trigeminal nerve – Eyelid – Digits – Areas with little soft tissue – tibia, digits, ulna, etc Equipment for Punch Biopsy Punch – 2-8mm. Choose the punch that can completely excise the lesion – < 3mm may not need sutures – > 6mm , best to use an elliptical excision. Fine, sharp-sharp scissors Forceps Needle holder Suture material Local anesthesia Punch Biopsy Procedure Sterile Technique Choose a punch to remove entire lesion Local anesthesia 1% lidocaine Apply tension perpendicular to Kraissel’s lines with hand not performing the punch. Apply punch completely over the lesion, apply pressure, and rotate through the dermis – expose the subq. Adipose tissue. Remove the plug, cut with sharp-sharp scissors and send for pathology Undermine if needed Close with simple interrupted sutures Dress and provide follow-up instructions Punch Biopsy CPT – 11100 – Biopsy of skin, subcutaneous CPT – 11101 – Biopsy of each separate or additional lesion. Shave Biopsy Indicated for raised lesion removal Advantages – minimal time, simple, no suturing, generally good cosmetic results Shave Biopsy Consider for – – – – skin tags seborrheic keratosis nevi actinic keratosis Not indicated for suspected melanoma!! Shave Biopsy Prep skin Local anesthesia to elevate lesion Use #15 blade or DermaBlade Excise the lesion level or minimally depressed in relation to the surrounding skin. Achieve hemostasis – Pressure – Electrodessication – Topical agents Aluminum chloride Monsel’s solution Silver nitrate Submit for pathology Shave Biopsy Shave Biopsy - DermaBlade CPT – Depends on site and size. 11300 – Trunk, arm, leg < 0.6 cm 11301 - Trunk, arm, leg 0.6 – 1.0 cm Many others, see CPT code book. Elliptical Excision Used when lesion is too large for punch Removes full thickness lesion Major steps – Planning – Anesthesia – Incision – Undermining – Hemostasis – Closure Planning the Elliptical Excision Avoid vital structures! Know anatomy! Know Kraissel’s lines and plan accordingly Incisional margin 3x diameter of lesion Anesthesia Incision with # 15 blade perpendicular to the skin surface through epidermis and dermis Undermine to allow closure of the incised area Surgical Blades Elliptical Excision Hemostasis – pressure, electrocautery, local anesthesia with epinephrine if indicated!!!! Wound closure – vertical mattress, 2 layer closure, single layer closure. Send specimen for pathology Elliptical Excision Remember………… Skin tension lines!!!! Elliptical Excision Elliptical Excision CPT – 11400 – Benign excision, TAL. < 0.6 cm CPT - 11401 – Benign excision. TAL 0.6 – 1.0 cm Additional CPT depending on size and location. Common Office Procedures References American Heart Association (2007, April 19). Prevention of Infective Endocarditis: Guidelines From the American Heart Association, by the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease. Circulation Buttaravoli, P (2012) Minor Emergencies. Splinters to Fractures, 3rd Edit. Mosby Blair, RE (2007, March) “Surgical Management of Soft Tissue MRSA Abscesses”, Family Physician News Mayeaux, EJ (2009)The Essential Guide to Primary Care Procedures. Wolters/Lippincott/Williams &Wilkins Pfenninger, JL (2011) Procedures for Primary Care, 3rd Edition: Mosby Trott, AT (2012) Wounds and Lacerations, 4th Edit. Mosby