Cat-scratch disease
advertisement

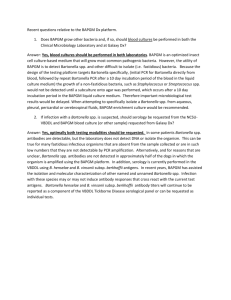
CAMPYLOBACTER LEGIONELLA BARTONELLA Campylobacter sp. Organism Source(s) Human disease(s) C. coli Pigs, poultry, sheep, bulls, birds Gastroenteritis, septicemia C. jejuni ssp. jejuni Poultry, pigs, bulls, dogs, cats, birds, others Gastroenteritis, septicemia, meningitis, proctitis C. jejuni ssp. doylei Humans Gastroenteritis, gastritis, septicemia C. fetus ssp. fetus Cattle, sheep Septicemia, gastroenteritis, abortion, meningitis Clinical characteristics • C. coli and C. fetus cause most human disease • Transmitted through contaminated food, milk, or water • Campylobacter does not multiply in food • Person-to-person transmission is rare Clinical characteristics, cont. • Seasonality in the U.S.; late summer-early fall peak • Most common etiology of gastroenteritis in U.S. • GI disease is typically self-limiting • Post-infectious complications can include Guillain-Barré Laboratory Diagnosis Specimen collection • No special requirements; stool and blood 1° specimens • For stool delayed more than 2 hrs: Cary-Blair transport Campy thio (thio broth with 0.16% agar and vancomycin, trimethoprim, cephalothin, polymyxin B and amphotericin B) Laboratory Diagnosis, cont. Stool Culture • Selective media and optimal conditions required • Campy-CVA at UMHS Brucella agar base with antibiotics (cefoparazone, vancomycin, and amphotericin B) 5% sheep blood • 42°C, microaerobic (10% CO2, 5% O2, 85% N2), 72 hrs Laboratory Diagnosis, cont. Blood Culture • Can routinely be detected in commercial systems • Some isolates may require 2 weeks to be detected • Subcultures require incubation microaerobically Laboratory Diagnosis, cont. Microbiologic characteristics • Growth at 42°C, microaerobically, grayish colonies • Gram-negative bacillus; faintly staining • Small rods, curved or seagull-winged • Motile (darting on wet prep) • Oxidase and catalase positive • Reported as Campylobacter sp. CDC Public Health Image Library (PHIL) http://www.lf3.cuni.cz/ustavy/mikrobiologie/rep/caje.htm Treatment Antimicrobial Susceptibility Testing • Standardized methods recently made available, but not routinely performed Therapy • Susceptible to macrolides, tetracyclines, aminoglycosides, and quinolones • Erythromycin is drug of choice for severe GI illness, with Ciprofloxacin as an alternative • Parenteral therapy required for systemic infections Legionella sp. Species isolated from humans Species isolated from environment only L. pneumophila, serotypes 1-15 L. micdadei L. bozemanii L. dumoffii L. feelei L. gormanii L. hackeliae L. longbeachae L. oakridgensis L. wadsworthii L. cherrii L. erythra L. gratiana L. jamestowniensis L. brunensis L. brunensis L. fairfieldensis L. santicrusis • Over 40 species in the genus • L. pneumophila is the predominant pathogen Epidemiology and pathogenesis • Ubiquitous in environment; primarily aquatic habitat • Widely distributed in natural and man-made environments • Acquired environmentally, not person-to-person • Exposure through inhalation of aerosolized organisms • Can infect and multiply within free-living parasites - survival in environment • Resist destruction following phagocytosis - survival in host Clinical characteristics • Causative agent of Legionnaires’ Disease - identified in 1976 following outbreak of severe respiratory illness at an American Legion convention in Philadelphia - organism did not grow on routine media - identification required months by CDC • Fever, pneumonia; case-fatality rate of 10-20% Clinical characteristics, cont. • Pontiac fever - identified in Pontiac, MI - self-limiting, not-fatal respiratory infection • Other infections - wound abscesses, encephalitis, endocarditis Clinical characteristics, cont. • Highest at-risk populations Immunocompromised Heavy smoker Over age 60 • Same organisms may manifest itself differently in different individuals • Also impacted by baseline immunity and dose Laboratory Diagnosis Specimen collection • Respiratory tract specimens - sputum, BAL, pleural fluid • Blood, tissue, biopsy material Specimen processing • Standard precautions (BSC) • Concentration of dilute specimens Laboratory Diagnosis, cont. Direct detection • DFA for organism in respiratory specimens • Urine antigen test Immunochromatographic commercial test Only detects L. pneumophila, serogroup 1 Legionella DFA Legionella Urine Ag Laboratory Diagnosis, cont. Culture • Include Buffered Charcoal Yeast Extract (BCYE) Agar Charcoal to detoxify specimen Cysteine Inhibitors (polymixin B, anisomycin, cefamandole) • Incubate 35 – 37°C, room air, for 7-10 days Laboratory Diagnosis, cont. Identification • Small, gray-white to blue-green colonies wet, ground-glass speckling • Gram stain yields thin, gram-negative rods • ID of colony using FA reagents • Report as Legionella sp. Colonies on BCYE http://www.rivm.nl/infectieziektenbulletin/bul1212/diagnose_en_preventie.html Gram stain http://reaannecy.free.fr/Documents/infectio/legionellose.htm Laboratory Diagnosis, cont. Serodiagnosis • Turkey RBCs sensitized with Legionella antigens • Set up in pools for screening purposes • Incubate with patient serum and look for agglutination • Test against individual antigens for type-specificity • Only available at MDCH Treatment Antimicrobial Susceptibility Testing • In vitro results do not correlate with clinical outcome, so not routinely performed Therapy • Azithromycin is effective against this and other causes of “atypical pneumonia” • Fluoroquinolone for severely ill • Penicillins, cephalosporins, and aminoglycosides are not effective Bartonella sp. Organism Resevoir Transmission Disease(s) B. bacilliformis ?humans Sand flies Carrión’s disease B. quintana ?humans ?rodents Human body louse Trench fever, relapsing fever, bacteremia, endocarditis, bacillary angiomatosis, lymphadenopathy B. henselae Domestic cats Cat bites or scratches Cat-scratch disease, bacteremia, endocarditis, bacillary angiomatosis, peliosis hepatitis • Bartonella currently includes 16 species, only 5 cause human disease Epidemiology and pathogenesis • Agent primarily of zoonotic infections • Increasing in importance as a pathogen in immunocompromised hosts • Pathogenesis is not well understood, but diseases caused by all species seem to be pathologically similar Clinical characteristics • Trench fever (B. quintana) - transmitted from infected body louse - affected many soldiers in battle - influenza-like headache, bone pain, splenomegaly, maculopapular rash Clinical characteristics • Cat-scratch disease (B. henselae) - papule or pustule develops at site of cat bite/scratch - regional tender lymphadenopathy develops in 1-7 weeks - disease ranges from chronic, self-limited adenopathy, to severe systemic illness Cat-scratch disease Los Angeles Co. West Vector Control District http://www.lawestvector.org/bartonella.htm http://www.uvp5.univ-paris5.fr/ MICROBES/Diagnostic/Bartonella/Bartonella.asp Clinical characteristics • Bacillary angiomatosis (B. quintana and B. henselae) - vascular proliferative disease (organisms stimulate angiogenesis) - small papules enlarge to form red – purple nodules - can occur on the skin surface, in subcutaneous tissue, or in visceral organs - primarily seen in HIV+; some reports in transplant patients Bacillary angiomatosis http://www.emedicine.com/derm/topic44.htm Laboratory Diagnosis Specimen collection • Blood, tissue, biopsy material Direct detection • Histopathologic detection in tissue using WarthinStarry silver stain • PCR for detection in tissue and body fluids Demonstration of Bartonella henselae in cardiac valve of a patient with blood culture-negative endocarditis. The bacilli appear as black granulations (Warthin Starry, original magnification X250). http://www.cdc.gov/ncidod/eid/vol8no2/01-0141-G2.htm Laboratory Diagnosis, cont. Culture • Fastidious organism; culture infrequently performed Laboratory Diagnosis, cont. Serodiagnosis • Main method for diagnosis • IFA using antigen prepared from co-cultures • HIV-infected patients may not mount an antibody response to infection Treatment Antimicrobial Susceptibility Testing • In vitro testing is difficult because of limited availability of strains and fastidious nature of organism Therapy • Aminoglycosides, beta-lactam agents, erythromycin, and doxycycline • At-risk individuals should avoid exposures to cats