Low cardiac output syndrome
advertisement

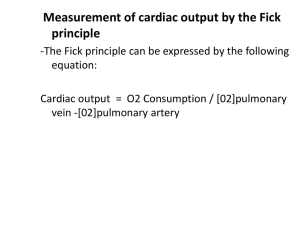
LOW CARDIAC OUTPUT SYNDROM IN CHILDREN AFTER CARDIAC SURGERY Hala EL-Mohamady, professor of anaesthesia, Ain Shams University Low cardiac output syndrome (LCOS) is a clinical syndrome seen commonly (25%) after pediatric cardiac surgery but also occurring secondary to acute myocarditis and septic shock. Regardless of aetiology, the resulting effects are shock and inadequate organ perfusion organ dysfunction Coincide With Postoperative decrease in cardiac index and increases in SVR and PVR reducing cardiac output This occurs typically 6–18 h after cardiopulmonary bypass, which is usually in the middle of the night! Causes of postoperative LCOS -Inflammatory cascade triggered by (CPB) -Aortic cross-clamp -Hypothermia -Reperfusion injury -Pericardial tamponade -Residual cardiac lesions, even when minor PREVENTION Because LCOS is common and contributes to postoperative morbidity and mortality, prevention of this predictable hemodynamic deterioration may have significant implications for clinical outcome Diagnosis OF LCOP SYNDROM Anticipation is the key to the diagnosis and management of LCOS So Diagnosis relies on anticipation, clinical features and investigation CLINICAL Features OF LOW COP SYNDROM - tachycardia - oliguria (0.5 ml/kg/h) - poor peripheral perfusion - low blood pressure The ability of clinicians to assess cardiac output from clinical examination alone is poor INVESTIGATIONS - Metabolic acidosis - Lactate - Mixed venous oxygen saturation - Echocardiography Management aimed at achieving the optimal balance between oxygen delivery and oxygen consumption A check list of immediately treatable causes is useful, as is a flow diagram to lead staff through a logical approach. Check list of causes of postoperative LCOS -Adequate airway (tube position, size and patency) and ventilation (atelectasis, pneumothorax) -Pericardial tamponade -Pulmonary hypertensive crisis -Arrhythmias (loss of AV synchrony, tachycardia or bradycardia) -Significant residual lesion -Electrolyte abnormality (e.g. hypocalcaemia) Preload Preload is traditionally assessed by: measuring filling pressures from right and left atrial lines. In addition, venous capacitance also affects venous return. Venodilatation often occurs on rewarming and may be exacerbated by drugs Finally, positive pressure ventilation (PPV) will tend to reduce RV preload by inhibiting venous return. Left ventricular afterload Reduction in LV afterload will improve cardiac output, as long as an adequate diastolic pressure is maintained for coronary perfusion. Left ventricular afterload Short Acting Vasodilators Nipride GTN Long Acting Vasodilators Phenoxybenzamin Captopril PPV Right ventricular afterload pulmonary hypertension Pulmonary hypertension Right ventricular Failure poor COP Preventive treatment strategies For PULMONARY HYPERTENSION -optimal sedation -neuromuscular -induced blockade respiratory or metabolic alkalosis -hyper-oxygenation Avoiding or ablating stimuli (trigger pulmonary hypertensive crises(e.g. administering fentanyl bolus prior to airway suction). -Nitric oxide Nitric Oxide a potent endogenous vasodilator that produces vascular relaxation via increases in the intracellular concentration of guanosine 3,5-cyclic monophosphate. It is a specific pulmonary vasodilator when delivered by inhalation (iNO), RV afterload is reduced, thereby improving RV ejection fraction and cardiac output. Nitric Oxide ? Rebound pulmonary hypertension Pharmacological treatment of systolic and diastolic dysfunction It should be remembered that all of these potent agents will increase myocardial oxygen demand, and that they should be titrated to the minimal dose that achieves the desired effect. They should not be commenced or increased prior to consideration of preload and afterload. Terms used for cardiovascular drugs Term Meaning Inotropy Increased force of myocardial contraction not related to preload or afterload Chronotropy Dromotopy Lusitropy Increased rate Increased speed of electrical conduction Increased effectiveness of active diastolic relaxation Agent Dobutamine Dopamine Noradrenalin e Dose range Stimulate (mcg/kg/mi n) 1–15 Main effects b14b2 Inotropy, chronotropy, dromotopy,VD 1–5 (low) 5–15 (high) B14a1 a14b1 Inotropy, chronotropy, dromotopy Vasoconstriction inotropy, chronotropy 0.1–0.5 a1bb1 Vasoconstriction with some inotropy Agent Adrenaline Dose range Stimulates (mcg/kg/min) 0.05–o.1(low) Main effects a1 ¼ b1 ¼ b2 Inotropy, 0.1–1 (high) a14b14b2 chronotropy, dromotopy, bronchodilation, multiple endocrine effects (increased glucose, lactate) As above plus potent vasoconstrictio Agent Dose range (mcg/kg/min Stimulates Main effects Milrinone 75 mcg/kg load, 0.25–1 Inhibits phosphodiester ase III Inotropy, lusitropy and vasodilation Vasopressin 0.02 U/min (not kg) V1, V2 Potent vasoconstrictio n Levosimendan 25 mcg/kg load, 0.2 for 24 h Ca2+ sensitivity of troponin C Inotropy, lusitropy and vasodilation Thyroid hormone Thyroid hormone has an essential role in cellular metabolism and in maintaining haemodynamic stability. It is required for the synthesis of contractile proteins and to maintain normal myocardial contraction. Suppression of thyroid hormone levels has been demonstrated in children following CPB, maximal between 12 and 48 h and lasting up to 7 days after CPB. Lack of evidence to demonstrate benefit. Nesiritide B-type natriuretic peptide is synthesized and excreted from the ventricular myocardium in response to myocardial stretch. It results in natriuresis, diuresis and vascular smooth muscle relaxation. Clinically it is said to augment preload and reduce afterload. Nonpharmacological treatment of Systolic and diastolic dysfunction Delayed sternal closure The aim is to allow the heart to recover, and become less oedematous without the added problem of ‘‘dry’’ tamponade. Delayed closure is associated with an increased risk of mediastinitis (particularly with gram negative organisms), and thyroid suppression from iodine absorption from iodine-based antiseptics. When the sternum is closed, significant haemodynamic and respiratory changes can occur and should be anticipated. Induced hypothermia Reducing the body temperature results in a reduction in metabolic rate, oxygen demand and heart rate, and may have a direct beneficial effect on cardiac function. SVR is increased and stroke volume and MAP are maintained. Although hypothermia is a useful rescue strategy, it is not without risks, including sepsis, coagulation disorders and altered pharmacokinetics. Neuromuscular paralysis is usually required to prevent shivering which, if unopposed, will increase oxygen consumption and lactate production Mechanical support The major benefit of mechanical circulatory support in the treatment of LCOS is allowing time for myocardial recovery whilst preventing ongoing damage to other organ systems Veno-arterial (VA) ECMO, and LV and/or RV assist devices are the two commonest methods of mechanical support. Selection and assessment of candidates for ECLS is extremely important. Bleeding is the most common complication, particularly from the wound, but intracranial haemorrhage can occur usually resulting in withdrawal of therapy. Pacing and arrhythmia management Arrhythmias that result in loss of AV synchrony, or significantly affect heart rate, are common (425%) and poorly tolerated in the setting of LCOS. Tachycardia can allow inadequate time for ventricular filling, especially with a poorly compliant ventricle; bradycardia is also poorly tolerated. AV synchrony is particularly important in LCOS as the effects of atrial systole (atrial kick) on ventricular preload can be significant, and contributing up to 20% of stroke volume. AV synchrony is particularly important in LCOS as the effects of atrial systole (atrial kick) on ventricular preload can be significant, and contributing up to 20% of stroke volume. Minimizing the consequences of LCOS Classically, a prolonged period of LCOS can lead to a -ventilator-dependant -oedematous -malnourished child -significant sedation problems -vascular access difficulties. Much can be done to minimize the effects of LCOS while awaiting intrinsic myocardial recovery. Renal failure Renal failure and fluid retention are common due to poor renal perfusion and low mean blood pressure. Diuretics are usually necessary after the first 24 h. Early peritoneal dialysis (PD) started prior to significant oedema formation, can prevent excessive fluid bolus administration, ionotrope escalation and frusemide toxicity. Respiratory failure Respiratory failure following LCOS is usually multifactorial, resulting from fluid overload, malnutrition, muscle weakness, critical illness polyneuropathy, atelectasis, upper airway oedema and intrinsic lung disease, with significant reduction in FRC secondary to sternotomy. Appropriate ventilation strategies that optimize PEEP, minimize tidal volume (6-8 ml/kg) and avoid paralysis are optimal. Nutrition, Sedation Optimal nutrition is often difficult due to fluid restriction and gut failure. Early enteral nutrition and the early use of jejunal feeding strategies are important. TPN is sometimes required but can often be avoided by jejunal feeding. It is often worth starting PD to make space for increased caloric intake. Optimal sedation and uncomplicated venous access are always strived for but rarely achieved. Flow diagram to guide management of LCOS. Low Cardiac Output State Exclude specific problem • Airway/ventilation • Tachycardia, oliguria, poor perfusion, low BP • Metabolic acidosis • Rising lactate • Low venous saturation • Pericardial tamponade • Pulmonary hypertension • Arrhythmia • Residual lesion • Electrolyte abnormality Evaluate and treat specific problem • ECHO • Atrial ECG • Surgical /medical intervention • Fluid challenge 5-10 Assess Preload clinical exam, CVP, LAP. ml/kg of 4% Albumin or give blood if: Hb<10-12 (acyanotic) or <12-14 (cyanotic) low • Reassess and repeat • Consider effects of ventilation on venous return Left Ventricle afterload Right Ventricle afterload high high(PHT) • Short/long acting vasodilators • Inodilators • Positive pressure ventilation • Sedation • High FiO2 • iNO • Optimal PEEP Systolic function Diastolic function reduced reduced Inotropy • dobutamine • low dose adrenaline • Increase preload • Lusitopy (milrinone) • Atrial “kick” Minimise effects of LCOS • Diuretics/PD not improving • Optimal nutrition • Optimal ventilation Consider • Sternal reopening • Hypothermia • Mechanical support CONCLUSION LCOS is a common problem in paediatric intensive care that is often predictable and sometimes preventable. Diagnosis relies on anticipation, clinical features and investigation. Management is aimed at achieving the optimal balance between oxygen delivery and oxygen consumption. Preload and afterload should be optimized prior to escalation of inotropic support. The effects of PPV and nonpharmacological strategies should not be underestimated.