Oxygen Delivery
advertisement
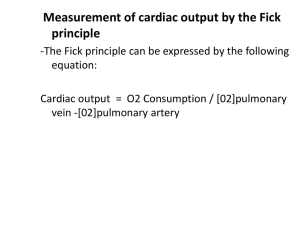
Oxygen Delivery Jenny Boyd, MD Case #1 12 mo male with a history of truncus arteriosus type I s/p repair with placement of a 12 mo maleconduit who just heart surgery RV-PA ashad a newborn who isand nowis s/p veryconduit sick. We have to take care of until 7AM replacement. Patient is him being when the morning admitted to the crew PCCUarrives. post-operatively. What are the goals of our care? Images from American Heart Association Care of the PCCU Patient 2 main goals of critical care: Ensure adequate oxygen delivery! Buy time! Why Is Oxygen Important? Used in cellular respiration Needed for energy production by cells and tissues Glucose GLYCOLYSIS 2 ATP Oxygen Pyruvate KREB’S CYCLE + ELECTRON TRANSPORT 34 ATP Case #1 (cont.) Initial assessment: PERRL, clear BS bilaterally, RRR, soft belly, warm extremities, well-perfused, 2+ pulses, brisk cap refill. Initial CXR looks good, all tubes and lines in expected places. Initial ABG: pH 7.32, pCO2 52, pO2 142, BE 0.2, lactate 3.9 (nl <2) Initial elevation of lactate very common postbypass, should resolve within 4 hours Case #1 (cont.) Over the next few hours, patient is hemodynamically stable with good perfusion, decent UOP and minimal bleeding from surgical site. Repeat ABGs are normal except the lactate rises from 3.9 4.4 5.1 Are you worried? Is an elevated lactate harmful? Where Does Lactate Come From? Glucose GLYCOLYSIS 2 ATP Oxygen Pyruvate KREB’S CYCLE Lactate + ELECTRON TRANSPORT 34 ATP So, why is our patient’s lactate elevated? Oxygen Delivery O2 delivery dependent on cardiac output and O2 content of the blood . . DO2 = CaO2 * Q O2 content is primarily due to hemoglobin saturation with little contribution of dissolved O2 in blood CaO2 = (SaO2* Hb * 1.34)+(0.003 * PaO2) Oxygen Delivery (cont.) From previous equations, we can simplify to: . O2 Delivery ≈ Hgb x SaO2 x Q So, there are 3 reasons for poor O2 delivery: 1) anemic anoxemia (low Hgb) 2) anoxic anoxemia (low SaO2) . 3) stagnant anoxemia (low Q) How much O2 delivery does our patient need? Oxygen Consumption Goal: O2 delivery > O2 consumption Adequate O2 delivery may become insufficient if tissue O2 consumption increases! Fever increases O2 consumption 10% per degree Agitation can increase O2 consumption by 40% Back to the Patient! Due to the elevated lactate, we minimize O2 consumption by ensuring our patient is afebrile and well sedated. However, our next lactate has risen to 7.0. What’s wrong with our patient? Anemic? Low sats? Low cardiac output? Our Patient (cont.) Since return from the OR, our patient’s Hgb has been > 10 and SaO2 has been >95% How do we know what our cardiac output is? What determines cardiac output? Measuring Cardiac Output Thermodilution Echocardiography Need cardiac catheterization Need an echocardiographer Shortening fraction Surrogate markers Oxygen extraction Oxygen Extraction Measure O2 consumption by looking at O2 extraction: SaO2 – SvO2 Should be ~20 - 30 mmHg Need arterial line and right atrial line Increased O2 extraction can be due to increased O2 consumption (hungry mouths) or decreased O2 delivery (not enough food) Regional Oxygen Extraction NIRS (Near-Infrared Spectroscopy) Monitoring Measures organspecific oxygen extraction Kidney – Surrogate for cardiac output ≈ SaO2 – 15 Brain – Because the brain is important! ≈SaO2 – 30 Image from Children’s Hospital of Wisconsin . Understanding Cardiac Output (Q) . Q = Heart Rate x Stroke Volume What determines stroke volume? Preload Contractility Afterload Increasing preload increases myosin-actin overlap, resulting in increased stroke volume Increasing contractility increases stroke volume for a given preload Increasing afterload decreases stroke volume for a given preload Stroke Volume Frank-Starling Curve Preload . Increasing cardiac output (Q) . Remember: Q = Heart Rate x Stroke Volume Increase heart rate Increase preload Preload ≈ CVP Increase contractility Pacing Inotropes Inotropes Decrease afterload Vasodilators Where were we? Our patient was having rising lactates despite minimizing O2 consumption and having normal Hgb and SaO2. As we check on him, we note that he is normotensive, warm and wellperfused, with good peripheral pulses and brisk capillary refill. He has had adequate urine output since return from the OR. What other information do you want/need? Arterial SO2 = 100% Mixed venous SO2 = 75% Renal SO2 = 90% Cerebral SO2 = 80% CVP = 14 So why is our lactate so high? Increased production Dead tissue? Decreased clearance Liver failure? Conclusion As the nurse is drawing a hepatic function panel, your patient begins to seize. After terminating his seizure, an emergent head CT is performed, revealing left-sided cerebral infarction, probably a bypass-related complication. Patient discharged to home on POD #8 on Keppra with weakness of RUE