Hospital Response to Disaster in a Rural Setting
advertisement

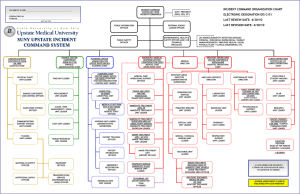
Hospital Disaster Response in a Rural Setting Presented by Barbara Ringhouse, RN MSN Assistant Administrator at Island Hospital In Anacortes, Washington Anacortes, Washington Far west end of Skagit County Population - 16,000+ Located on Fidalgo Island - connected to mainland and to Whidbey Island by bridges Medical Response Capabilities in Anacortes Three city-operated Fire Stations staffed with paramedic/firefighters or EMT/firefighters. Three volunteer fire districts with 5 volunteer fire stations. Hospital-owned ambulance used for non-stat transfers. Medical Facility in Anacortes Island Hospital 43 bed acute care hospital 10 bed Emergency Department Level III Trauma Center Board Certified ED physicians TNCC/ENPC trained Emergency Nurses Trauma Surgeons on staff 4 Surgical Suites Fully staffed ICU Hospitalists on staff Patient base - approx.40,000 Average daily census – 28 Annual ED visits – 14,000 Disaster Response Capability of Island Hospital ICS trained Incident Command Staff ICS/Disaster Trained Emergency Department Staff 16 person Team Delta Dedicated Hospital Decontamination Team Onsite Hospital Helicopter pad with additional off-site landing zones Bi-annual disaster exercises with community and regional partners Risks/Vulnerabilities for Anacortes Earthquakes Tsunami Winter storms Wind Storms Mass Casualty Incidents Potential sites for Mass Casualty Incidents Anacortes, Washington…A quiet, pleasant USA small town Until…………. April 2, 2010 at approximately 12:30 am an explosion awakened the sleepy Anacortes community. The explosion happened at one of the local refineries just across the bay from Anacortes in one of the naphtha production units. Many minutes passed before the sirens started blowing. The only person able to sound that alarm was one of the victims! Normal Staffing for night shift at Island Hospital Board Certified ED physician ON CALL: Two ED Registered nurses Trauma Surgeon, One Admissions clerk Night shift coordinator 3-4 Acute Care Registered nurses 2 Acute Care CAN 2-3 ICU Registered nurses 1 security guard Assorted housekeepers 1 radiology tech Anesthesiologist, CT tech, OR nursing staff, On-call Admin. person Hospital Response to this event…. What worked well. Code External Triage Communications with called overhead Incident Command opened by Night Nursing Coordinator ED prepared for burn patients immediately Hospital Emergency Preparedness Coordinator called in Field EMS triage officer consistent. Early notification of the severity of injuries. Airlift notified early so arrived almost simultaneously with first patient. Burn Center notified early in the event. Timing couldn’t have been better Called in more ED nurses Medics completed work at prior to patients arrival. ICU and Acute Care nurses able to come to ED to help Only one previous patient in the ED, awaiting a ride home. No other patients arrived in the ED that night except patients from explosion the scene and came to help. Received calls from Skagit Hospital and Providence Medical Center – Everett to offer help in caring for patients Diverted two patients from the scene to Skagit Valley Hospital Airlift able to divert helicopters enroute. Patient Conditions Patient #1 - Arrived at 0130 Patient #2 – Arrived at 0205 Full thickness burns to 80 Full thickness burns to 95 percent of BSA No history available No airway on arrival Surgical airway performed in ED Central line, Foley, and burn dressings applied Door to Departure time: 50 minutes percent of BSA No history available No airway and no IV line on arrival only I/O access (not working) Surgical Airway performed in ED ( Very difficult to obtain) Central line, Foley, burn dressings. Door to Departure time: 70 minutes The difficult part of response… Severe burns not common to our staff. Patients had full thickness burns to 80-95 percent of their bodies. Patients arrived awake and still talking to medics and staff. It was discovered on arrival of second patient that the patient was a relative of one of our house supervisors. Total response 22 members of Island Hospital staff took care of two severely burned patients: Trauma Surgeon, Anesthesiologist, ED physician, 5 ED nurses, Nursing Coordinator, Respiratory Therapist, ICU nurse, Acute care nurse, CNA, unit clerk, admissions clerk, radiology tech, security guard, and housekeeping staff (runners) Had two Airlift helicopters on site – one in a nearby landing zone set up by police department. Two full Airlift crews worked along side the ED staff. One of the medic units stayed and helped in the hospital. Is this how we would always respond? Our response would be the same regardless of size of the incident. We keep our staff trained. We exercise our plans. We review every exercise and every real event for the lessons learned. We work with 10 other regional facilities on a monthly basis. Consistency in the way any hospital prepares and responds to disaster is key. Code External Triage Our response would be the same regardless of size of the incident. Consistency in the way a hospital responds to disaster is key. Code External Triage paged overhead Incident Command opened – usually starts in the ED with Nursing Coordinator then moves to first arriving administrator and into our secure Incident Command Center. Incident Command decision Level of response needed is determined with input from ED physician and staff. Calls go out through either call trees or the hospital’s Everbridge Alert Network. Triage area is set up and assignments made. Communication is established with the EMS triage officer at the scene and maintained until incident is over. Island Hospital Level of Response Level 1 – Usually affects on the ED and the ED staff will determine how many personnel are needed from those already here at work and then notify Incident Command Center. Level 2 – A partial hospital call back system activation will occur after Incident Command Center has received reports from each department as to what the personnel needs are for the individual departments and orders that activation. Level 3 – An entire hospital call back system activation will occur after the Incident Command Center determines the disaster is large enough to warrant all hospital employees to respond. A level 3 activation requires the establishment of a labor pool. Level 3 response required Hospital lockdown initiated if deemed necessary by Incident Commander and staff are assigned to attend all doors. Incident Command opens labor pool and all staff not doing direct patient care report to labor pool. All elective procedures are cancelled. All inpatients are assessed for possible early discharge and Hospitalist is notified. Hospital PIO assignment area and location of press area is designated. But what if………………..? The actual number of victims from this incident were small but what if it had been a large number of victims. 50…75..100. We have several large community events annually, Tulip Festival, Art Festival, Jazz Festival, and Oyster Run 50 to 100 patients would quickly drain any facilities resources. This is the time that regional planning pays off. Region 1 Hospital Bed Control Region 1 Bed Control would be contacted by the Incident Command and Island Hospital response would be expanded to reach out to all other Region 1 facilities. Further information regarding Island Hospital Disaster Response is available through: Linda Seger, RN CEN Island Hospital Emergency Preparedness Coordinator 360-299-4226 or lseger@islandhospital.org