4) HFOV for LPV and OLC
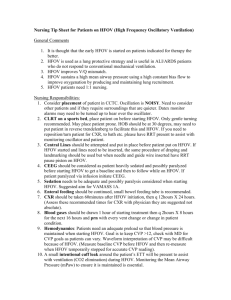
advertisement

High frequency oscillatory ventilation (HFOV): How does it work and how to integrate it in the concept of lung protective ventilation and of the open lung? 1) What is HFOV? Specific characteristics of HFOV 2) Basic mechanisms of gas exchange during HFOV - How to set MAP when switching from CMV - What are optimal settings and how to monitor - Basic concepts of lung recruitment during HFO 3) How does HFOV fit in actual concepts of lung protection? HFO =/ HFJV =/ HFPPV Humidifed Bias Flow Patient “Elimination” of tidal ventilation Slutsky AS ARRD 1988;138:175-83 Gas transport mechanisms during HFOV Bouchut JC et al. Anesthesiology 2004; 100:1007-12 Pressure transmission CMV / HFOV : Tracheal pressure Endinspiration Gerstman et al Endexpiration CMV HFO PEEP 10, Vt 6 CDP 16 CMV HFOV CMV HFOV HFO Lung volumes The Paw is used to inflate the lung and optimize the alveolar surface area for gas exchange. Paw = Lung Volume Oxygenation Oxygenation is primarily controlled by the mean airway pressure (Paw) and the FiO2 for “Diffuse Alveolar Disease”. The Paw is used to inflate the lung and optimize the alveolar surface area for gas exchange. Paw = Lung Volume From the lab to the bedside: The principal concepts Adapted from Suzuki H Acta Pediatr Japan 1992; 34:494-500 Lung Recruitment Using Oxygenation during Open Lung High-Frequency Ventilation in Preterm Infants Adapted from Suzuki H Acta Pediatr Japan 1992; 34:494-500 De Jaegere Ann et al. Am J Respir Crit Care Med 2006: 174; 639–645 Lung Recruitment Using Oxygenation during Open Lung High-Frequency Ventilation in Preterm Infants Adapted from Suzuki H Acta Pediatr Japan 1992; 34:494-500 De Jaegere Ann et al. Am J Respir Crit Care Med 2006: 174; 639–645 Lung Recruitment Using Oxygenation during Open Lung High-Frequency Ventilation in Preterm Infants before surfactant De Jaegere Ann et al. AJRCCM 2006: 174; 639–645 after surfactant The Open Lung Approach with HFOV (Lung-Lavaged Rabbits) McCulloch, Forkert, Froese ARRD 137:1185-1192,1988 Percentage airways with lesions 100 80 60 4+ Epithelial injury Hyaline Membranes 40 20 0 HFO-Hi HFO-Lo CMV Ventilation Ventilation is primarily determined by the stroke volume (Delta-P) or the frequency of the ventilator. Alveolar ventilation during CMV is defined as: F x Vt Alveolar Ventilation during HFV is defined as: F x Vt 2 Therefore, changes in volume delivery (as a function of pressure-amplitude, frequency, or % inspiratory time) have the most significant affect on CO2 elimination Frequency controls the time allowed (distance) for the piston to move. Therefore, the lower the frequency, the greater the volume displaced, and the higher the frequency, the smaller the volume displaced. Theory of operation Oxygenation and CO2 elimination have been demonstrated to be decoupled with HFOV 5 Hz versus 15 Hz: does it matter? Meyer J et al. PediatrRes 2006; 60: 401–406 5 Hz versus 15 Hz: does it matter? Meyer J et al. PediatrRes 2006; 60: 401–406 Mean airway pressure, amplitude and frequency MAP (CDP): recruits alveoli/airways and maintains alveolar volume it is closely related to lung volumes and oxygenation Amplitude: there is a close relationship between pressure amplitude and tidal volume tidal volume depends on: 1) the volume displaced by the piston or diaphragm, 2) the resistance of the airways, 3) the compliance of the ventilator circuit, and 4) the patient’s lung mechanics therefore: search for visible chest vibrations change amplitude to control ventilation (PaCO2) Bouchut JC et al. Anesthesiology 2004; 100:1007-12 How to set initial MAP when switching to HFOV 100 90 90 80 80 70 70 volume (ml) 100 60 50 40 30 60 50 40 30 20 20 10 10 0 0 0 5 10 15 20 25 pressure (cmH2O) 30 35 0 5 10 15 20 25 pressure (cmH2O) 30 35 Recruitment concept during HFO And reduce FiO2! Adapted from Suzuki H Acta Pediatr Japan 1992; 34:494-500 Volume above FRC by respitrace A recruitment procedure in iRDS Drop in SO2 5 10 10 15 20 Airway pressures 25 30 35 Recruit first the lung and then keep open the lung at the lowest pressure necessary! Some bedside rules: 1) Lower FiO2 before CDP (=MAP) 2) Always try to define lung closing pressure to assure that you will use lowest pressures required 3) Try to work always the highest frequency possible - increase the amplitude in a first step to correct for high pCO2 Adapted from Suzuki H Acta Pediatr Japan 1992; 34:494-500 4) If you’re “lost” - always decrease CDP first! The clinical experience: HFO vs CMV Elective HFOV vs CMV: Death or CLD at 36 w GA or discharge All trials Favors HFO Favors CMV With volume recruitment Cumulative Meta-Analysis: Incidence of CLD Bollen et al. AJRCCM 2003; 168: 1150–1155 Elective HFOV versus CMV CLD at 36-37 wks PMA or discharge Henderson-Smart DJ Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No.: CD000104. DOI: 10.1002/14651858.CD000104.pub2. Elective HFOV versus CMV CLD at 36-37 wks PMA or discharge Henderson-Smart DJ Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No.: CD000104. DOI: 10.1002/14651858.CD000104.pub2. 35% 39% NNT 25 Elective HFOV versus CMV Combined Outcome: Death or CLD at 36-37 wks PMA or discharge Henderson-Smart DJ Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No.: CD000104. DOI: 10.1002/14651858.CD000104.pub2. HFOV compared with CMV for Diffuse Alveolar Disease or Air Leak in Pediatrics Arnold et al. Crit Care Med 1994;22 58 Children (29 CMV, 29 HFO) Protocol: MAP was set 4-8 cm H2O > CMV-MAP Decrease FiO2 before MAP Results: No difference in Death, Length of Vent., Air Leak. Significant improvement in oxygenation with HFO over time.* Less need for O2 at 30 days with HFO.* HFOV is safe and improves oxygenation as well as outcome * p<0.05 MOAT II: Overall Survival N P/F HFOV CV 75 114 (37) 73 111 (42) 1 30d p=0.057 90d p=0.078 Proportion of Survivors 0.9 0.8 0.7 HFOV 0.6 0.5 0.4 CV 0.3 0.2 0 10 20 30 40 50 60 70 80 Days Af te r Random izat ion 90 Derdak S Am J Respir Crit Care Med 2002; 166:801–808 Predictors of Outcome 1) Oxygenation Index Response MAP x FiO2 x 100 (OI = ) PaO2 2) Entry Indicators of Compliance (Peak Inspiratory Pressure) MOAT II: Predictors of Outcome Derdak S Am J Respir Crit Care Med 2002; 166:801–808 MOAT II: Survival - PIP 38 cmH20 (post-hoc) 1 30d p=0.019 90d p=0.026 Proportion of Survivors 0.9 0.8 0.7 HFOV 0.6 0.5 CV 0.4 0.3 0.2 0 10 20 30 40 50 60 70 80 Days Af te r Random izat ion 90 HFV-Meeting 2001 Early (< 24 h) versus late (>24 hours) intervention in pediatric ARDS Fedora M Bratisl Lek Listy 2000; 101: 8-13 Metha S et al. Crit Care Med 2001; 29:1360 –1369 Time concepts for lung protection Katzenstein AL et al. Surgical pathology of non-neoplastic lung disease. Saunders, Philadelphia, 1982 Neither a ventilation strategy nor a mode can repair the injured lungs First Intention HFO with early lung volume recruitment Demographic data and severity of lung disease all patients HFO (n=32) CMV (n=39) p - value Birth weight (g) 981 ± 242 965 ± 254 n.s.* Estimated gestational age (weeks) 27.7 ± 2.0 27.7 ± 1.8 n.s.* Antenatal steroid treatment, no (%) 13 (41) 14 (36) n.s.# APGAR score < 4 at 1 min, no (%) 13 (44) 17 (44) n.s.# APGAR score < 6 at 5 min, no (%) 7 (22) 5 (13) n.s.# 2.9 ± 0.8 3 ± 0.9 n.s.* 0.16 ± 0.09 0.20 ± 0.16 n.s.* Degree of HMD (1 - 4) on CXR aA-ratio (first blood gas analysis) Values are given as mean ± SD, or as the number (percentage) of patients; * unpaired t-test; ** Chi-square; # Fisher's exact Rimensberger PC et al. Pediatrics 2000; 105:1202-1208 First Intention HFO with early lung volume recruitment Observational study, historical cohort: 71 premature infants with RDS at birth Mean airway pressure PaO2/FiO2 ratio 30 300 25 250 20 200 HFO 15 HFO 150 CMV 100 10 CMV 5 50 0 0 0 2 4 6 8 10 12 14 16 18 20 22 24 time (h) 0 2 4 6 8 10 12 14 16 18 20 22 24 time (h) Rimensberger PC et al. Pediatrics 2000; 105:1202-1208 First Intention HFO with early lung volume recruitment days of ventilation 100 oxygen dependency • HFO • CMV 80 60 100 • HFO • CMV 80 60 p = 0.0004 40 P < 0.0001 40 20 20 n=3 0 0 0 20 40 60 80 days 100 120 140 0 20 40 60 80 days 100 120 140 Rimensberger PC et al. Pediatrics 2000; 105:1202-1208 First Intention HFO with early lung volume recruitment Survival and CLD Morbidity all patients HFO (n=32) CMV (n=39) survivors to 30 days Ventilation (days) Oxygen dependency (days) Oxygen at 28 d, no (%) HFO (n=27) CMV (n=35) 5 (3-6) 14 (6-23) 0.0004 * 12 (4-17) 51 (20-60) <0.0001 * 6 (22) 22 (63) 0.002 # survivors to 36 weeks PCA HFO (n=27) CMV (n=34) CLD; Oxygen > 36 weeks PCA, no (%) 0 (0) 12 (35) p - value 0.0006 # Values are given as the median (95% CI) or the number (percentage) of patients; * Mantel-Cox log-rank; # Fisher's exact Rimensberger PC et al. Pediatrics 2000; 105:1202-1208 Recruitment bei der Hyalinen Membranenkrankheit (RDS) 28 wks GA, 8 hours after birth, on HFOV, no surfactant received MAP 26 cmH2O MAP 12 cmH2O, Amplitude 40, FiO2 0.8 08’10 MAP 16 cmH2O, Amplitude 28, FiO2 0.21 08’25 Recruitment during both, HFO and CMV, follows similar concepts when using small tidal volume ventilation 100 100 90 90 80 70 volume (ml) 80 HFO after recruitment 60 60 50 50 40 40 30 30 20 20 10 10 0 0 0 5 10 15 CMV after recruitment 70 20 25 pressure (cmH2O) 30 35 0 5 10 15 20 25 30 35 pressure (cmH2O) Rimensberger PC Intensive Care Med 2000; 26; 745-755 1. Similar effect on oxygenation 2. Similar protective effect on histology Rimensberger PC Intensive Care Med 2000; 26; 745-755 Lung recruitment (open lung concept) during both, CMV and HFO reduces VILI in newborn piglets Lavaged PPVOLC HFOOLC PPVCON Van Kaam A Ped Research 2003 Lung recruitment (open lung concept) during both, CMV and HFO reduces VILI in newborn piglets PPVcon PPVOLC HVOOLC Controls Van Kaam A Ped Research 2003 OLV improves gas exchange and attenuates secondary lung injury in a piglet model of meconium aspiration pO2 pCO2 Van Kaam A et al. Crit Care Med 2004; 32:443–449 OLC in a neonatal piglet lavage model Van Kaam A Biol Neonate 2003;83:273-80 Recruitment and the Open Lung Concept is all about avoiding collapse and overdistention Recruitment and the Open Lung Concept during HFOV is all about keeping the lung open at the least pressure cost Volume (l) The difficulty to place the ventilatory cycle within the safe window during CMV when compared to HFOV ALI (surfactant depleted lung) severe (A)RDS Airway pressure (cmH2O) Adapted from Suzuki H Acta Pediatr Japan 1992; 34:494-500 Hickling KG et al. AJRCCM 2001; 163:69-78 “The beauty of simplicity” HFOV: Turn 1 knob … and observe 2 parameters (O2, CO2) CMV: chose your allowable Vt Turn then 1 (or 2 knobs) … and observe 3 parameters (O2, CO2, Cdyn) and remember to adapt Ti and Te Time constant: T = Crs x Rrs Adapted from Suzuki H Acta Pediatr Japan 1992; 34:494-500