HFOV
advertisement

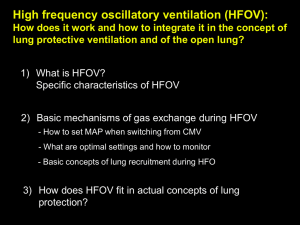
High-Frequency Oscillatory Ventilation Vin K. Gupta, MD Division of Pediatric Critical Care Medicine Mercy Children’s Hospital Toledo, Ohio Ira M. Cheifetz, MD Division of Pediatric Critical Care Medicine Duke Children's Hospital Durham, North Carolina Outline Review of Acute Lung Injury & Respiratory Mechanics HFOV: A General Overview Optimizing Oxygenation Optimizing Ventilation Routine Management of the Patient on HFOV Acute Lung Injury In acute lung injury (ALI) there are 3 regions of lung tissue: Severely diseased regions with a limited ability to "safely" recruit. Uninvolved regions with normal compliance and aeration. Possibility of overdistension with increased ventilatory support. Intermediate regions with reversible alveolar collapse and edema. Ware et al., NEJM, 2000 Respiratory Mechanics ALI is associated with a decrease in lung compliance. Less volume is delivered for the same pressure delivery during ALI as compared to normal conditions. Lower and upper inflection points: At the lower end of the curve, the alveoli are at risk for derecruitment and collapse. At the upper end of the curve, the alveoli are at risk of alveolar overdistension. Volume NORMAL Acute Lung Injury Pressure Ventilator Associated Lung Injury All forms of positive pressure ventilation (PPV) can cause ventilator associated lung injury (VALI). VALI is the result of a combination of the following processes: Barotrauma Volutrauma Atelectrauma Biotrauma Slutsky, Chest, 1999 Barotrauma High airway pressures during PPV can cause lung overdistension with gross tissue injury. This injury can allow the transfer of air into the interstitial tissues at the proximal airways. Clinically, barotrauma presents as pneumothorax, pneumomediastinum, pneumopericardium, and subcutaneous emphysema. Slutsky, Chest, 1999 Volutrauma Lung overdistension can cause diffuse alveolar damage at the pulmonary capillary membrane. This may result in increased epithelial and microvascular permeability, thus, allowing fluid filtration into the alveoli (pulmonary edema). Excessive end-inspiratory alveolar volumes are the major determinant of volutrauma. Atelectrauma Mechanical ventilation at low end-expiratory volumes may be inefficient to maintain the alveoli open. Repetitive alveolar collapse and reopening of the underrecruited alveoli result in atelectrauma. The quantitative and qualitative loss of surfactant may predispose to atelectrauma. Biotrauma In addition to the mechanical forms of injury, PPV activates an inflammatory reaction that perpetuates lung damage. Even ARDS from non-primary etiologies will result in activation of the inflammatory cascade that can potentially worsen lung function. This biological form of trauma is known as biotrauma. Capillary Leak Electron microscopy demonstrates the disruption of the alveolar-capillary membrane secondary to mechanical ventilation with lung distention. Note the leakage of RBCs and other material into the alveolar space. Fu Z, JAP, 1992; 73:123 Pressure-Volume Loop Froese, CCM, 1997 Open Lung Ventilation Strategy Zone of Overdistention Volume Safe window Zone of Derecruitment and atelectasis Goal is to avoid injury zones and operate in the safe window Pressure Froese, CCM, 1997 Outline Review of Acute Lung Injury & Respiratory Mechanics HFOV: A General Overview Optimizing Oxygenation Optimizing Ventilation Routine Management of the Patient on HFOV Pressure and Volume Swings During CMV, there are swings between the zones of injury from inspiration to expiration. During HFOV, the entire cycle operates in the “safe window” and avoids the injury zones. INJURY HFOV CMV INJURY Pressure Transmission With CMV, the pressures exerted by the ventilator propagate through the airway with little dampening. With HFOV, there is attenuation of the pressures as air moves toward the alveolar level. Thus, with CMV the alveoli receive the full pressure from the ventilator. Whereas in HFOV, there is minimal stretching of the alveoli and, therefore, less risk of trauma. HFOV Gerstmann D. Lung Protective Strategies Utilizing HFOV in an open lung strategy provides a more effective means to recruit and protect acutely injured lungs. The ability to recruit and maintain FRC with higher mean airway pressures may: improve lung compliance decrease pulmonary vascular resistance improve gas exchange With attenuation of P, there is less trauma to the lungs and, therefore, less risk of VALI. HFOV improves outcome by shear forces associated with the cyclic opening of collapsed alveoli. Arnold, PCCM, 2000 HFOV - General Principles A CPAP system with piston displacement of gas Active exhalation Tidal volume less than anatomic dead space (1 to 3 ml/kg) Rates of 180 – 900 breaths per minute Lower peak inspiratory pressures for a given mean airway pressure as compared to CMV Decoupling of oxygenation & ventilation Indications for HFOV Inadequate oxygenation that cannot safely be treated without potentially toxic ventilator settings and, thus, increased risk of VALI. Objectively defined by: Peak inspiratory pressure (PIP) > 30-35 cm H2O FiO2 > 0.60 or the inability to wean Mean airway pressure (Paw) > 15 cm H2O Peak end expiratory pressure (PEEP) > 10 cm H2O Oxygenation index > 13-15 (Paw FiO2) OI = PaO2 100 Relative Indications for HFOV (Regardless of ventilator settings or gas exchange) Alveolar hemorrhage (Pappas, Chest, 1996) Sickle cell disease in acute chest syndrome (Wratney, Resp Care, 2004) Large airleak with inability to keep lungs open (Clark, CCM, 1986) Inadequate alveolar ventilation with respiratory acidosis (Arnold, PCCM, 2000) Patient Selection The clinical goals and guidelines presented are for the “typical” patient with ALI/ARDS. The goals may differ for: Other disease states – reactive airway disease, acute chest syndrome, flail chest, congenital diaphragmatic hernia, sepsis, pulmonary hypertension. Certain patient groups – congenital cardiac disease, closed head injury. Clinical Goals Reasonable oxygenation to limit oxygen toxicity SaO2 86 to 92% PaO2 55 to 90 mm Hg Permissive hypercapnea Provide “just enough” ventilatory support to maintain normal cellular function. Monitor cardiac function, perfusion, lactate, pH Allow PaCO2 to rise but keep arterial pH 7.25 to 7.30. (Derdak, CCM, 2003) This strategy helps to minimize VALI. (Hickling, CCM, 1998) ‘Normal’ pH, PaCO2, & PaO2 are indictors of OVERventilation!! Outline Review of Acute Lung Injury & Respiratory Mechanics HFOV: A General Overview Optimizing Oxygenation Optimizing Ventilation Routine Management of the Patient on HFOV Variables in Oxygenation The two primarily variables that control oxygenation are: FiO2 Mean airway pressure (Paw) Paw is displayed here 23 Mean Airway Pressure (Paw) is controlled here 35 33 7.5 Mean Airway Pressure (Paw) Use to optimize lung volume and, thus, alveolar surface area for gas exchange. Utilize Paw to: recruit atelectatic alveoli prevent alveoli from collapsing (derecruitment) Although the lung must be recruited, guard against overdistension. Alveolar atelectasis or overdistension can result in pulmonary vascular resistance (PVR). Effect of Lung Volume on PVR Overexpansion PVR Atelectasis Total PVR Small Vessels Large Vessels FRC Lung Volume Overexpansion of Atelectasis of large PVR is the lowest small at FRC vessels PVR vessels PVR Oxygenation – Clinical Tips Initiate HFOV with FiO2 1.0 Paw 5-8 cm H2O greater than Paw on CMV Increase Paw by 1 - 4 cm H2O to achieve optimal lung volume. Optimal lung volume is determined by: increase in SaO2 allowing the FiO2 to be weaned diaphragm is at T9 on chest radiograph Maintain the Paw and wean the FiO2 until ≤ 0.60. Oxygenation – Clinical Tips Follow CXR’s to assess lung expansion. If the diaphragm is between 8 and 8½, continue to wean the oxygen. If the diaphragm is between 9 and 9½, wean the Paw by 1 cm H2O. You should be able to wean the FiO2 to < 0.60 within the first 12 hours of HFOV. If unable to wean FiO2, consider: a recruitment maneuver (sustained inflation) increasing the Paw Oxygenation – Clinical Tips Lung perfusion must be matched to ventilation for adequate oxygenation (V/Q matching). Ensure adequate intravascular volume & cardiac output. The higher intrathoracic pressure may adversely affect cardiac preload. Consider volume loading ( 5 mL/kg) or initiating inotropes. Closely monitor hemodynamic status. Utilize pulse oximetry and transcutaneous monitors to wean FiO2 between blood gas analyses. Outline Review of Acute Lung Injury & Respiratory Mechanics HFOV: A General Overview Optimizing Oxygenation Optimizing Ventilation Routine Management of the Patient on HFOV Ventilation The two primarily variables that control ventilation are: Tidal volume (P or amplitude) Controlled by the force with which the oscillatory piston moves. (represented as stroke volume or P) Frequency () Referenced in Hertz (1 Hz = 60 breaths/second) Range: 3 - 15 Hz Variables in Ventilation f x Vt In CMV, ventilation is defined as: In HFOV, ventilation is defined as: f x Vt1.5-2.5 Therefore, changes in Vt delivery have a larger effect on ventilation than changes in frequency. Amplitude (P) The power control regulates the force and distance with which the piston moves from baseline. The degree of deflection of the piston (amplitude) determines the tidal volume. This deflection is clinically demonstrated as the “wiggle” seen in the patient. The wiggle factor can be utilized in assessing the patient. “Wiggle Factor” Reassess after positional changes If chest oscillation is diminished or absent consider: decreased pulmonary compliance ETT disconnect ETT obstruction severe bronchospasm If the chest oscillation is unilateral, consider: ETT displacement (right mainstem) pneumothorax Amplitude Selection Start amplitude in the 30’s and adjust until the “wiggle” extends to the lower level of patient’s groin. Adjust in increments of 3 to 5 cm H2O Subjectively follow the wiggle Objectively follow transcutaneous CO2 and PaCO2 Remember, the goal is not to achieve ‘normal’ PaCO2 and pH, but to minimize VALI. This is displayed as the amplitude or P 23 The power dial controls the degree of piston deflection 35 33 7.5 Resonance Frequency There is a resonance frequency of the lungs in which optimal ventilation (CO2 removal) occurs. Resonance frequency varies based on: lung size the degree of lung injury Katz, AJRCCM, 2001 Resonance Frequency In this example, 7 Hz represents the resonance frequency at which a greater tidal volume delivery occurs for the same amplitude (i.e., piston deflection). Heliox 60 Heliox 40 O2/N2 Katz, AJRCCM, 2001 Resonance Frequency The resonance frequency depends on: the amount of functional lung the type and extent of the disease state the size of the patient Therefore, the resonance frequency can vary between patients and in the same patient over the time. Initial Frequency Settings Guidelines for setting the initial frequency. Patient Weight Preterm Neonates Term Neonates Children Adults Hertz 10 to 15 8 to 10 6 to 8 5 to 6 Adjustments in frequency are made in steps of ½ to 1 Hz. Frequency () To evaluate the effects of changes in frequency with regards to CO2 elimination, let us look at 2 different frequencies. 4 Hz 8 Hz Frequency () Time X 4 Hz Lets consider a time interval of X 8 Hz Frequency () 4 Hz The lower the frequency setting, the larger the volume displacement. 8 Hz Time X Frequency () 4 Hz The higher the frequency setting, the smaller the volume displacement. 8 Hz Time X Frequency () Therefore, lower frequencies have a larger volume displacement and improved CO2 elimination. Time X The frequency is controlled and read here 23 35 33 7.5 Improving Ventilation To improve ventilation first increase the amplitude. If this does not improve CO2 elimination, consider decreasing the frequency. Although controversial, some centers consider decreasing the frequency by 1 Hz once the amplitude is 3 times the Paw. Ventilation - Clinical Tips With cuffed endotracheal tubes, minimally deflating the cuff may improve ventilation. Monitor for a loss in Paw with the airleak created by deflating the cuff. Inspiratory Time The initial inspiratory time setting is 33%. If carbon dioxide elimination is inadequate, despite deflating the ETT cuff (or if the patient has an uncuffed tube), consider increasing the itime (max 50%). Increasing the i-time allows for a larger tidal volume delivery. The inspiratory time is controlled and read here 23 35 33 7.5 Improved Ventilation If there is appropriate chest wiggle and the PaCO2 is too low, consider increasing the frequency. Once you have improved ventilation or are in the weaning phase, do not forget to: decrease i-time to 33%. reinflate the ETT cuff (if deflated). raise/adjust the frequency as the resonance frequency of the lungs changes. wean the amplitude. Outline Review of Acute Lung Injury & Respiratory Mechanics HFOV: A General Overview Optimizing Oxygenation Optimizing Ventilation Routine Management of the Patient on HFOV Sedation/Neuromuscular Blockade Transitioning a patient from CMV to HFOV typically indicates that the patient’s respiratory distress has worsened. To facilitate ‘capturing’ the patient, additional sedation may be required. Neuromuscular blockade may be required. As the patient improves, discontinue the paralysis and wean the sedation as tolerated. Auscultation Listen to the lung fields to primarily assess the presence and symmetry of piston sounds. Asymmetry may indicate improper ETT placement, pneumothorax, heterogeneous gross lung disease, or mucus plugging. Pause the piston to perform a cardiac exam and assess heart sounds. With the piston paused you have placed the patient in a CPAP mode and will have maintained Paw. Chest Radiographs Typically obtain a chest radiograph 1 hour after initiating HFOV and then Q12-24 hours. Assess ETT placement Rib expansion (goal is 9 ribs) Pneumothorax / airleak syndrome Change in lung disease Suctioning Indications: Routine suctioning to ensure the ETT remains patent Frequency of suctioning varies by institution. Our policy is every 12 to 24 hours and prn. Decreased/absent wiggle Possibly from mucus plugs/secretions Decrease in SpO2 or transcutaneous O2 level Increase in transcutaneous CO2 level Suctioning de-recruits lung volume May be minimized but not fully eliminated with closed suction system. May require a sustained inflation recruitment maneuver following suctioning. Sustained Inflation (SI) A sustained inflation is a lung recruitment maneuver. There are several ways in which to perform a SI maneuver. In our institution, the piston is paused (thus leaving the patient in CPAP) and the Paw is increased by 8-10 cm H2O for 30-60 seconds. Once the SI maneuver is completed, the piston is restarted. Potential complications: Pneumothorax CV compromise / altered hemodynamics When To Utilize A SI Maneuver When initiating HFOV to recruit lung After a disconnect or loss of FRC/Paw After suctioning (even with a closed suction system) Inability to wean FiO2 When considering increasing Paw A recruitment maneuver may recruit lung allowing you to maintain the baseline Paw and, thus, not increase support. Potential Complications of HFOV The higher intrathoracic pressures with HFOV may decrease RV preload and require volume administration ± inotropic support. Pneumothorax Migration/displacement of ETT Bronchospasm Acute airway obstruction from mucus plugging, secretions, hemorrhage or clot. Summary Open the lungs and keep them open HFOV improves outcome by shear forces associated with the cyclic opening of collapsed alveoli. (Krishnan, Chest, 2000) Minimize P (i.e., shear injury) to the lungs by minimizing the swings from inspiration to expiration. Ventilate in the “safe window”. Oxygenation and ventilation are dissociated. Adjust Paw independently of P Looking towards the future A great deal remains unknown about HFOV: the exact mechanism of gas exchange the most effective strategy to manipulate ventilator settings the safest approach to manipulate ventilator settings a reliable method to measure tidal volume the appropriate use of sedation and neuromuscular blockade to optimize patient-ventilator interactions Additional research in these and other issues related to HFOV are necessary to maximize the benefit and minimize the potential risks associated with HFOV. Looking towards the future A great deal remains unknown about ARDS in the pediatric patient. Although there has been a substantial quantity of research performed in using various treatment options in adults (prone positioning, steroids, iNO, tidal volume, etc.), many of these therapies have not been evaluated in pediatric patients with ARDS. Additional research in the pathophysiology of pediatric ARDS and various treatment options is necessary. References Priebe GP, Arnold JH: High-frequency oscillatory ventilation in pediatric patients. Respir Care Clin N Am 2001; 7(4):633-645 Arnold JH, Anas NG, Luckett P, Cheifetz IM, Reyes G, Newth CJ, Kocis KC, Heidemann SM, Hanson JH, Brogan TV, et al.: Highfrequency oscillatory ventilation in pediatric respiratory failure: a multicenter experience. Crit Care Med 2000; 28(12):3913-3919 Arnold JH: High-frequency ventilation in the pediatric intensive care unit. Pediatr Crit Care Med 2000; 1(2):93-99 Slutsky, AS: Lung Injury Caused by Mechanical Ventilation. Chest 1999; 116(1):9S-14S dos Santos CC, Slutsky AS: Overview of high-frequency ventilation modes, clinical rationale, and gas transport mechanisms. Respir Care Clin N Am 2001; 7(4):549-575 Duke PICU Handbook (revised 2003) Duke Ventilator Management Protocol (2004)