Synthesis, storage and release of thyroid hormones
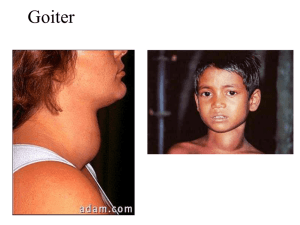
advertisement

Thyroid hormones and antithyroid drugs normal amount of thyroid hormones are essential for normal growth and development by maintaining the level of energy metabolism in the tissue. Either too little or too much thyroid hormones will bring disorders to the body. Part 1 Thyroid hormones Two major thyroid hormones are: triiodothyronine(T3, the most active form) thyroxin(T4) The characteristic of their chemical structure is that they all contain iodine as an essential part of the molecule. Structure inadequate secretion of thyroid hormone (hypothyroidism) can bring many disorders to the body (eg. bradycardia, poor resistance to cold, both mental and physical slowing.) [Synthesis, storage and release of thyroid hormones] Synthesis Iodine is the raw material of the thyroid biosynthesis. Once taken up by the thyroid gland, iodine undergoes a series of enzymatic reactions before it converts into active thyroid hormones. Synthesis; four steps 1. iodine trapping :uptake of iodine by the thyroid gland 2. oxidation of iodine: (to its active form) thyroid peroxidase (key enzyme of the synthesis) 3. iodide organification :the iodination of tyrosyl groups of thyroglobulin productions: MIT and DIT 4. formation of T4 and T3 from MIT and DIT : thyroid peroxidase storage store in the colloid droplets of thyroglobulin release The hormones are released by proteolysis of thyroglobulin . Enzyme: thyroglobulin hydrolase The ratio of T4 to T3 within thyroglobulin is about 5:1 Differences between T3 and T4 the effect of T3 is much faster, stronger and shorter than that of T4. conversion T4 can converse to T3 through deniodonite in peripheral tissues as well as in the thyroid. (catalyzed by deiodinase) Regulation: TRH Hypothalamus TSH pituitary T3,T4 thyroid Controled by HPT(hypothalamic-pituitary-thyroid) axis Regulation TRH (thyrotropin releasing hormone) TSH (thyroid stimulating hormone or thyrotropin) [Pharmacokinetics] Pharmacological actions Effects on growth and development Calorigenic effects : Hypersensitivity to catecholamine : Pharmacological actions 1.Effects on growth and development : responsible for normal growth and maturation of human being , especially for nervous and skeletal tissues. so the absence of thyroid hormones before birth leads to both mental and physical retardation(cretinism) Pharmacological actions 2.Calorigenic effects: T3 /T4 can increase oxygen consumption, promote metabolism and BMR(basal metabolic rate) ,↓utility. So hyperthyroidism will result in excess heat production and body wasting. Pharmacological actions 3. hypersensitivity to catecholamine Cardiovascular effects: Tachycardia, hypertension nervous Effects: anxiety, nervous. mechanism TR CBP NUCLEAR R Clinical uses the major indications for the therapeutic use of thyroid hormones are for hormone replacement therapy in patients with hypothyroidism . Clinical uses 1.Cretinism :congenital hypothyroidism often happens in newborn babies, mainly caused by iodine deficiency before birth . Success in the treatment of cretinism depends on the age at which therapy is started. The earlier, the better. Cretinism Symptoms: 1.Physical slow: dwarf, with short extremities , 2.mentally retarded: inactive, uncomplaining and listless. incidence :about 1 per 400 births Prevention and therapy: Prevention: Iodine replacement is the best method prior to pregnancy. Therapy: thyroid hormones replacement(T4 is more often used than T3) Clinical uses 2.Myxedema: adult hypothyroidism Happens after individual development Slow in mentality With special edema Mortality :60% Clinical uses 3.Simple goiter: A kind of prevalent disease caused by insufficient dietary iodine TSH can promote hyperplasy and hypertrophy of thyroid gland. 4. Differential diagnosis of simple goiter and hyperthyroidism Simple goiter adverse reactions hyperthyroidism Part 2 Antithyroid drugs Grave’s syndrome Treatment of hyperthyroidism The goal of therapy is to decrease the additional hormone and attend to normal levels. Can be accomplished by removing part of the gland Inhibiting synthesis Blocking releasing four categories of anti-thyroid drugs Ⅰ Thioureas : (硫脲类) interfere directly with the synthesis of thyroid hormones Ⅱ High concentrations of iodine : decrease the release of thyroid hormones Ⅲ Radioactive iodine : damage the gland with ionizing radiation Ⅳ β- receptor antagonists: control the manifestations Ⅰ Thioureas(硫脲类) Thiouracils: methythiouracil , propylthiouracil Imidazoles: methimazole , carbimazole. Ⅰ Thioureas Pharmacological action : Decrease the level of thyroid hormones Mechanism 1.inhibit the thyroid peroxidase : (key enzyme of synthesis) interfere the oxidation of iodine and the coupling of MIT and DIT to form T3/T4 2. inhibit conversion from T4 to T3 3.immunosupressive effect: TSI Pharmacokinetics: Absorption Distribution Excretion Pass through placenta, milk Therapeutic uses 1.As definitive treatment to control hyperthyroidism 2.Preoperative preparations for subtotal thyroidectomy: to control the disorder in preparation for surgical treatment. (thioureas plus large dose of iodine) 3. Thyroid crisis Propylthiouracil is the first choice. Adverse reactions 1.allergic response 2.GI reaction 3.granulocytopenia (0.3%-0.6%) 4.Longterm use: goiter and hypothyroidism Drug interactions ↑ Li,sulfasulfonamide,PAS, paraminan(对氨苯甲酸), phenylbutazone,barbital, phentolamine,sulfonyl urea,vitB12 ↓ iodine Ⅱ Iodine and iodide Oldest agent have completely different effects due to different doses Pharmacological effects in small dose: ↑ synthesis of thyroid hormones in large dose : antithyroid 1) ↓the release of thyroid hormones into the circulation: strong Mechanism: Inhibit thyroglobulin hydrolase 2)↓synthesis of thyroid hormones: weak Mechanism: Inhibit thyroid peroxidase Therapeutic uses 1.Simple goiter : in small dose 2.In preparation for thyroidectomy : used after the hyperthyroidism has been controlled by thioureas, given for 7 to 10 days immediately preceding the operation. (The changes after a fairly long term of administration include: the vascularity of the thyroid gland is reduced, the gland becomes much firmer and smaller.) 3.Thryotoxic crisis Adverse reactions 1. Chronic iodism 2.Acute allergic action : angioneurotic edema and larynx edema 3. Thyroid dysfunction Ⅲ Radioactive iodine 131I : most often used isotope of iodine γ rays(1%): β particles(99%): destructive Effects on the thyroid gland 131I is rapidly and efficiently trapped by the thyroid gland and slowly emitsβparticles and γrays. The destructive βparticles can destroy the thyroid cells with little damage to surrounding tissues (the penetration range is only 0.4-2.0mm). Theγrays can pass through the tissue and be quantified by external detection Clinical uses 1.hyperthyroidism: administrated orally and the effective dose differs for individual patients. 2.diagnosis of thyroid functions Adverse reactions: hypothyroidism contraindications pregnancy and milk mothers IV β-adrenergic receptor antagonists ------ adjuvant therapy many of the symptoms of hyperthyroidism are associated with sympathetic stimulation, so β-R blockers are effective in antagonizing the catecholaminegic symptoms such as tachycardia, palpitations ,anxiety and tension. Action: (1)block 1-R of heart (2)block -R of CNS (3) block -R of presynaptic membrane of peripheral nerve. (4) Inhibit T4 converted into T3 Uses: 1.Control the symptoms of hyperthyroidism before confirmed diagnosis 2.Thyroid crisis 3.Preoperation of hyperthyroidism 4.Hyperthyroidism Section 3 TSH and TRH Thank you!