Oral Pictorial Essay Sample
advertisement
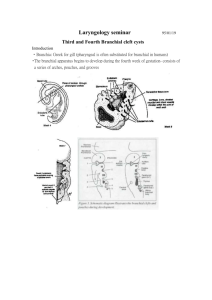
Pictoral Essay: Congenital Anomalies of the Branchial Apparatus Authors Institutions Objectives: Understand Embryology of the branchial apparatus and embryogenesis of its anomalies. Understand various classifications of branchial anomalies. Recognize and interpret imaging findings associated with anomalies of the branchial apparatus. Direct workup using various imaging modalities used in evaluation of branchial anomalies. Embryology of Branchial Apparatus 4th week of gestation. Six mesodermal arches Branchial clefts – ectodermally lined. Pharygeal pouches – endodermally lined. CN and Aortic arch accompany each branchial arch. Branchial Apparatus Development of Branchial Apparatus 1st Arch, Cleft, and Pouch persist. 2nd Arch increases in thickness and proliferates caudally 2nd, 3rd, and 4th Cleft form cervical sinus of His. Sinus of His lined by ectoderm. Further Differentiation 1st Branchial cleft becomes external auditory canal Cervical Sinus of His obliterated Pharyngeal pouches develop into thymus, parathyroid glands, and ultimobranchial body, then migrate to their final position. Branchial Derivatives Embryogenesis Vestigial remnants – resulting from incomplete or failed obliteration of branchial apparatus. Buried cell rests – cells are trapped in branchial apparatus and form branchial cleft cysts later in life. Branchial Anomalies Sinus – incomplete tract, opens externally Fistula – communicated both externally and internally from persistence of both cleft and pouch. Cyst – no internal or external comunication. Radiographic Evaluation Begins with Ultrasound CT Non ionizing, non invasive. Determines cystic vs. solid; size, and extent. Color doppler – vascularity. Morphologic characterization and staging. Bone structures, calcifications, deep soft tissue anatomy Low dose neck CT to avoid excess radiation. MRI Multiplanar capability Absence of ionizing radiation. Superior contrast resolution and anatomic characterization of soft tissues. Often requires sedation. First Branchial Anomalies 5-8 % of all defects. Middle aged women. 1st Branchial structures: maxilla, mandible, eustacian tube, external auditory canal, middle ear structures. Completed by 6-7 wks. Can insinuate within Parotid gland. 10 year old female presenting with fistula. Second Brancial Apparatus Anomalies Vast majority (>95%) of branchial anomalies. ¾ of anomalies are cysts. Fistulas and sinuses present earlier. Passes between internal and external carotid arteries and ends near tonsillar fossa. External communication with cervical sinus of His. Four types of nd 2 Bailey type I: Classic location Bailey type III: most superficial Anterior surface SCM Bailey type II: BCC Extends medially between ICA and ECA bifurcation Bailey type IV: Lies in pharyngeal mucosal space. 41 year old male with neck mass. Bailey type II: most common. Remnant of cervical sinus of His. Classic location: Anterior to SCM Lateral to carotid space Posterior to submandibular gland. 10 mo. Child presented with neck mass. Suspected abscess. Third Branchial Apparatus Anomalies. Very rare. Requires careful anatomic examination. Pierces the thyrohyoid membrane and enters pyriform sinus Posterior to carotid vessels Anterior to Vegus nerve. Posterior compartment behind SCM. Joins Cervical Sinus of His. Child with Neck Fullness. Cystic mass in left posterior compartment Beneath SCM. Posterior to Carotid vessels. Fourth Branchial Apparatus Anomalies. Very rare: complete fistula not reported. Origin at apex of pyriform sinus, penetrates thyrohyoid membrane. Descends below aortic arch Inferior to superior lanryngeal nerve. Superior to recurrent laryngeal nerve. Cervical sinus of His. 3 yo with recurrent neck abscess. Infected cyst anterior to carotid artery May communicate with pyriform sinus or cervical sinus of His Track descends below aortic arch. Case 1: Child with right facial mass. Submandibular Gland Carotid Sheath Sternocleidomastoid Case 2: Child with purulent drainage from EAC. Case 3: Child presenting with neck mass. Review Defects in branchial apparatus include branchial, thymic, and parathyroid anomalies. Manifest as cysts, sinuses, fistulas, and ectopic glands. Embryogenesis: vestigial remnants from incomplete obliteration or buried cell rests. Radiography, US, CT, MRI used for evaluation Review Branchial Cleft Anomalies: Fistulae, cysts, sinuses. Four types: Type II Branchial Cleft Cysts most common. Classic location BCC II: anterio-medial to SCM, displacing submandibular glands anteriorly, lateral to carotid vessels. Types II – IV merge externally as Cervical sinus of His. Types III and IV are rare and require careful anatomic examination for differentiation. References 1. Benson MT, Dalen K, Mancuso AA, et al.: Congenital abnormalities of the branchial apparatus: embryology and pathologic anatomy. Radiographics 12:739-748, 1992. 2. Meuwly JY, Lepori D, Theumann N, et al.: Multimodality Imaging Evaluation of the Pediatric Neck: Techniques and Spectrum of Findings. Radiographics 25:931-948, 2005. 3. Koeller K, Alamo L, Adair C, Smirniotopoulos J.: Congenital Cystic Masses of the Neck: Radiologic-Pathologic Correlation. Radiographics 19:121-146, 1999. 4. Langman J. Medical Embryology 3rd Ed. Baltimore: Williams & Wilkins, 1975; 234-236. 5. Barry H. The aortic arch derivatives in the human adult. Anat Rec 1951; 111:221-238.