Interfacial Surface Tension
advertisement
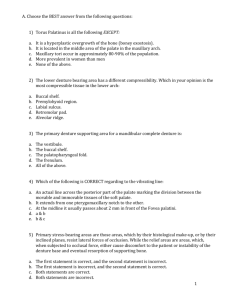
Rola M. Shadid, BDS, MSc Retention Resistance to denture removal in a direction opposite that of its insertion.* Stability Resistance of denture movement under the effect of horizontal or rotational forces. Support Resistance of movement of denture toward the basal seat area. The act of chewing foods Adhesive nature of certain foods Gravity (for upper denture) * Surrounding musculature Prematurities in occlusion Primary retention is from basal seat Secondary retention by improving stability & minimizing dislodging forces Physical means Mechanical means Adhesion Cohesion Interfacial surface tension Atmospheric pressure Capillary attraction Gravity Figure: retention due to pressure differential between saliva film & the air Relationship between the width of the buccal channel and resistance to flow of saliva: (a) wide channel, rapid flow, poor retention; (b) narrow channel, slow flow, good retention. Atmospheric pressure * Capillary attraction Saliva: quantity & quality * Surface area: the larger the surface area, the greater the retention.# Intimacy of contact: the closer the contact between the tissue and the impression surface of denture, the greater the retention. Peripheral seal The denture border should be shaped so that the channel between it and the sulcus tissues is as small as possible. It is not possible to maintain a close approximation between the border of a denture and the mucosal reflection in the sulcus at all times because the depth of the sulcus varies during function. The denture has to be constructed so that the border conforms to the shallowest point that the sulcus reflection reaches during normal function. * It is not possible to produce a facial seal along the posterior border of the upper denture as it crosses the palate. In this area, another approach to create the smallest possible space between denture and mucosa is adopted. A groove known as a post-dam is cut into the working cast so that the posterior border of the finished denture has a raised lip which becomes embedded a little way into the palatal mucosa. Right: denture poorly retained because the thin flanges failed to create a facial seal and the palatal coverage did not make the most of the area available. Left: the replacement denture corrected these errors and as a result had excellent retention. Undercuts Overdentures attachments Implants Mucosal inserts Rubber suction discs & suction chambers (No longer used) Magnets Selection of path of insertion to improve retention by utilising undercuts: (a) single path of insertion to engage labial undercut; (b) dual path of insertion to engage unilateral undercut. Mucosal insert or implant button: a nonreactive metal appliance that is affixed to the tissuebone surface of a denture and offers added retentive qualities to the denture. It consists of a base, cervix, and head. Rubber suction disc & suction chamber No longer used because they cause damage of soft tissues The surrounding musculature Occlusal schemes Proper patient instructions Psychological factor Neuromuscular control Denture fixative Long-term soft liners Cheek muscles Lips Modiolus can cause unseating of denture in premolar region Tongue Floor of the mouth Soft palate Masseter (affects the distobuccal region of mandibular denture) Neutral zone (zone of minimal conflict) o Explaining the central role of the tongue, lips and cheeks in controlling the denture and giving specific advice – such as supporting the posterior border of the upper denture with the tongue when incising. o Offering advice, for example, cutting food into smaller pieces before inserting them into the mouth. o Chewing on both sides of the dental arch simultaneously o Starting with softer ‘easier’ foods before progressing to more challenging morsels. As the patient incises, the upper denture is controlled by the tongue pressing against the posterior border. An aid to retention, particularly under difficult anatomical circumstances. Come in powder, paste or sheet form, the latter having the advantage of staying longest between the denture and mucosa. enable free, flexible margins to extend into the anatomical defect and engage tissue undercuts. can be constructed as an integral part of the denture base or as a separate obturator section retained on the denture base by rare earth magnets. Intimate contact (accuracy of fit) Residual ridge size & contour Residual ridge quality Palatal vault Neutral zone & surrounding musculature * Flange shape & contour: correct contouring the external surface of the denture base can enhance the stabilizing potential of surrounding musculature Occlusal factors Abnormal ridge relationships * Direct bone anchorage # Pressure from the bolus on the posterior part of the lower occlusal table, which overlies a sloping part of the ridge, causes the lower denture to slide forwards.* Firm resilient tissue covered by keratinized tissue & firmly attached to underlying bone Tissue of uniform thickness The bone be resistant to resorption The support areas should be at right angles to the occlusal surfaces All areas of denture bearing area should contribute to support except relief area Primary stress bearing areas Greater area of coverage puts less force per unit area (snow shoe principle) The larger surface area of maxillary denture (22.96cm2) allows a wider stress distribution compared with mandible (12.25cm2). Surface area Nature of supporting mucosa Impression procedure Accuracy of fit Direct bone anchorage * Retentive forces > displacing forces Adequate support Stability References: I. Complete Denture Prosthodontics, 1st Edition, 2006 by John Joy Manappallil, Chapter 2 II. Basker’s Prosthetic treatment of the edentulous patient. Fourth edition. Chapter 4.