35616752
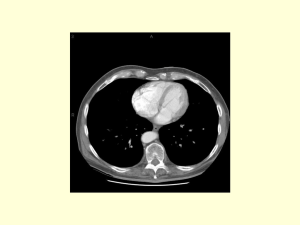
advertisement

The Pancreas The pancreas is a gland organ in the digestive and endocrine system.It’s both endocrine organ producing several important hormones, including insulin, glucagons, & somatostatin, as well as an exocrine organ, secreting pancreatic juice containing digestive enzymes that pass to the small intestine. These enzymes help in the further breakdown of the carbohydrates, fat &protein. Pancreatic parts It is long and irregularly prismatic in shape; its right extremity, being broad, and is lodged within the curve of the duodenum & called the head with lower prolongation called the uncinate process , the head is connected to the main portion of the organ, or body, by a slight constriction, the neck; while its left extremity gradually tapers to form the tail. It is situated transversely across the posterior wall of the abdomen, at the back of the epigastrium and left hypochondrium. Pancreatic ducts The Major pancreatic duct, or Duct of Wirsung joins the common bile duct just prior to the ampulla of Vater, after which both ducts perforate the medial side of the second portion of the duodenum at the major duodenal papilla. Accessory pancreatic duct or the Duct of Santorini opens into the duodenum about 2.5 cm. above the duodenal papilla. It receives the ducts from the lower part of the head, What are the peritoneal coverings of the pancreas ?? Pancreas is a Retroperitoneal organ!!!! Blood vessels related to pancreas Aorta & IVC lie behind the neck & body of the pancreas, Both superior mesenteric artery and vein pass anteriorly to the uncinate process . Splenic vein moves at the at the posterior aspect of the pancreas & unites with superior mesenteric vein to form the portal vein which lie behind the neck of pancreas. The splenic artery lie at the upper border of the pancreas. Histology of the pancreas Under a microscope, stained sections of the pancreas reveal two different types of parenchymal tissue Lightly staining clusters of cells are called islets of langerhans, which produce hormones (e.g Insulin) Darker staining cells form acini connected to ducts. Acinar cells belong to the exocrine function and secrete digestive enzymes into the gut via a system of ducts. Imaging Modalities of pancreas imaging of the pancreas can be divided into two categories Indirect imaging involves non-invasive radiologic techniques including: plain film, US, CT, MRI, MRCP. Direct imaging involves invasive radiologic procedures, which include: ERCP operative pancreatography. Plain Film The pancreas is not directly visualized on plain films of the abdomen. Calcifications in the pancreatic region or biliary lithiasis can sometimes be demonstrated. The presence of adynamic ileus of the duodenum& the proximal small bowel loops (sentinel loop) can be an important sign in acute disorders. Ultrasonography (US) How can you identify the pancreas at US? The body of the pancreas is usually found anterior to the splenic vein. In some patients however, body habitus and bowel gas may limit complete visualization. Computed Tomography (CT) is used to evaluate the differences in the density, texture, and contour of the pancreas. Secondary signs such as dilation of the bile or pancreatic duct, or changes in the peripancreatic fat density, are also used in the determination of a diagnosis. IV contrast enhancement is also used, especially in analysis of pancreatic masses. During CT examination of the pancreas thin pancreatic cuts are needed (3-5mm) to accurately identify pancreatic lesions. Magnetic resonance imaging (MRI) MRI shows soft tissue with super clarity, while avoiding the potential risks of ionizing radiation. Densities in an MR image are based on tissue water and lipid content (while CT densities are based on varying absorption of X-rays by different tissue). Magnetic resonance cholangiopancreatography (MRCP) MRCP is a non-invasive technique that delineates the pancreatic and biliary ductal systems, while providing projectional and cross sectional images of the ducts. MRCP does not require administration of intravenous contrast material; it is based on T2-weighted images, which depict static fluid (including bile and pancreatic secretions), with a higher signal intensity. MRCP also avoids the invasive complications of ERCP. With the recent improvements in MRCP, it is superceding ERCP for many of its diagnostic indications. MRCP is inferior to ERCP in several respects however. The spatial resolution of MRCP is lower than that of ERCP. Furthermore, ascites or fluid collections in the upper abdomen can interfere with the visualization of the pancreatic and biliary ducts. Endoscopic Retrograde Cholangiopancreatography (ERCP) ERCP is a combined endoscopic and radiographic procedure that images the biliary and pancreatic ducts. ERCP is performed with a side-viewing duodenoscope which has an instrumentation channel that allows for the insertion of the cannulation catheter into the major or minor duodenal papilla. A water-soluble contrast agent (60 % iodine) is injected into the ductal system using fluoroscopy for imaging. It is important to obtain adequate ductal filling without over-distending the system. (During interventional procedures, a guide-wire can be inserted through the cannulation catheter, for subsequent insertion of additional instruments like papillotomes, drainage devices, cytology brush, etc.) Althought ERCP is an important diagnostic tool in the evaluation of patients with suspected biliary and pancreatic disorders,MRCP is superceding ERCP for some of its indications. ERCP Indications >Pancreatic Diseases --Acute gallstone pancreatitis --Recurrent acute pancreatitis --Chronic pancreatitis --Pancreatic pseudocyst, abcess --Pancreatic tumors ERCP Pancreatography: The pancreatic ducts are filled with contrast (under fluoroscopy) until the tail and the first order side branches are visualized. Since the pancreatic duct empties relatively quickly, images are acquired while the endoscope is in situ. A normal pancreatogram shows the main pancreatic duct to be in the shape of a pistol. The mean diameter of the duct is 4mm at its distal end, which decreases towards the tail. (This diameter increases significantly with age.) Normal ducts have a smooth lining, with small, regular side-branches. Interpretation of a pancreatogram may be complicated by different congenital ductal variations. operative pancreatography Developmental anatomy, normal variants& congenital anomalies of the pancreas The pancreas develops from dorsal and ventral diverticula that buds from the primitive foregut. These 2 buds fuse after the rotation of the duodenum adjoins the two structures. The ventral bud develops from the hepatic duct, and forms the uncinate process and the posterior/inferior head of the pancreas. The dorsal bud develops directly from the foregut, forming the anterior head, body and tail of the pancreas. The distal duct system of the dorsal bud joins with that of the ventral bud to form the main pancreatic duct (of Wirsung), which joins with the common bile duct at the level of the ampulla of Vater. The distal duct system of the dorsal bud may persist as the accessory pancreatic duct (of Santorini), and empties into the duodenum at the minor duodenal papilla. The "normal" short axis measurement of the pancreas is 2.5 cm at the head, and 1.5 cm at the tail; there are normal variations. In general, the pancreas decreases with size with age. Pancreas Divisum Pancreas divisum represents an anomaly of the fusion of the two pancreatic buds and their respective ducts. It is the most common pancreatic ductal system anomaly; it is seen in 4-6% of ERCP patients. The duct of ventral bud does not fuse with the duct system of the dorsal pancreatic bud; it joins the common bile duct at the level of the ampulla of Vater. The dorsal duct of pancreas, which drains the anterior head, body and tail, terminates more cephalad, at the minor duodenal papilla. The narrow size of the os in the minor papilla may result in inefficient drainage of pancreatic secretions. It is widely believed that pancreas divisum predisposes to chronic pancreatitis Pancreas Divisum ERCP is the main diagnostic modality Cannulation of the major duodenal papilla and injection of contrast material reveals only a short segment of the main pancreatic duct Cannulation of the minor duodenal papilla and opacification of the dorsal pancreatic duct Annular Pancreas Annular pancreas results from a band of pancreatic parenchyma that encircles a section of the second part of the duodenum. The embryologic anomaly is secondary to the malrotation of the ventral bud, which wraps around the duodenum to fuse with the dorsal bud. This malformation can be isolated or can be accompanied by a digestive tract malrotation or atresia. Its frequency is also increased by Trisomy 21. Annular Pancreas The clinical consequences of annular pancreas depend on the degree of duodenal obstruction. In cases of complete obstruction, the diagnosis is readily evident in the neonate. Plain films reveal two asymmetrical air-fluid levels, one gastric, the other duodenal, with little distal bowel gas. This is the "double bubble" sign. The diagnosis can be suggested by prenatal US, which would demonstrate the two constant liquid-containing abdominal structures, possibly accompanied by hydroamnios. This anomaly may present later, and into adulthood, as partial duodenal obstruction or pancreatitis. The treatment of significant obstruction is always surgical. Common Variations in Ductal Anatomy