INTERNATIONAL CLASSIFICATION
of
HEADACHE DISORDERS
2nd edition
(ICHD-II)
Headache
Headache:
a clinical
tour
clinical part
tour2:
foraresidents
Secondary for
headache
disorders
residents
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
March 2010
Lucy Vieira MD
©International Headache Society 2003/4
Headache is the Most Common Symptom that
Humans Experience
Primary headaches (No underlying cause)
Migraine
Tension-type
TACs
Other
Secondary headaches (Underlying cause)
Medication overuse
Head/neck injury
Space-occupying lesion (i.e. brain tumour)
Vascular cause (i.e. Subarachnoid hemorrhage, intracranial
bleed)
>65% in
Infectious cause (i.e. meningitis patients
or upper respiratory tract
infection)
older
than 50
+ many others
Headache Classification Committee of the International Headache Society,1988
Any secondary
Headache disorder
can mimic a primary
headache disorder
Wolff HG, et al., 2001
1876 consec pts (38yo); 2/3 non acute:1.2%
◦ 99% had normal neuro exam
◦ Pituitary adenoma, arachnoid cyct, meningioma,
hydrocephalus, chiari I, stroke, cavernoma, glioma..
◦ Half treated surgically
◦ Only one lesion not appreciated on CT
US headache consortium meta-analysis of
patient with migraine and normal exam:
0.18% rate of significant pathology therefore
imaging not indicated.
Cephalalgia 2005;25:30-35. Neurology 1994;44:1353-54
Chronic Migraine
New Daily
Persistent Headache
(NDPH)
+/- medication
overuse
Chronic
Daily Headache
(CDH)
Chronic
Tension
Type
Headache
Headache Classification Subcommittee of the International Headache Society, 2004
Hemicrania
Continua
Other
What are the Secondary Causes of Chronic
Headaches?
Medication Overuse
Headache (MOH)
Sleep apnea
Cervicogenic
headache
Chronic
Daily Headache
(CDH)
Post-traumatic
headache
Decreased ICP
(spontaneous intracranial
hypotension)
Increased ICP
Other
(tumour/mass,
pseudotumour cerebri,
hydrocephalus)
What are the Headache “Red Flags”?
Systemic symptoms (fever, weight loss)
Secondary risk factors (cancer,
HIV/immunocompromised)
Neurologic symptoms or abnormal signs
Onset (i.e. new-onset chronic headache)
Older patient (i.e. new headaches at age >50 yrs)
Previous headache different (i.e. significant
change in headache frequency or clinical
features)
Positional component (i.e. increases when
upright)
Provocative factors (precipitated by coughing,
exercise, sex)
Vitals (particularly BP)
Pupil symmetry, reactivity and fundoscopy
Visual fields
Eye movements
Motor – look for asymmetrical weakness R vs L
Reflexes – look for asymmetry (increased
reflexes) R vs L
Sensation – extinction to double simultaneous
tactile stimuli
Coordination – finger-nose-finger, gain and
tandem gait
Examine/touch the head and neck
Olesen J , et al., 2006
Pryse –Phyllips WEM, et al., 1997
Part 2:
The secondary headaches
5. Headache attributed to head and/or neck trauma
6. Headache attributed to cranial or cervical vascular
disorder
7. Headache attributed to non-vascular intracranial
disorder
8. Headache attributed to a substance or its withdrawal
9. Headache attributed to infection
10. Headache attributed to disorder of homoeostasis
11. Headache or facial pain attributed to disorder of
cranium, neck, eyes, ears, nose, sinuses, teeth, mouth
or other facial or cranial structures
12. Headache attributed to psychiatric disorder
Part 2:
The secondary headaches
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
Primary or secondary
headache?
Primary:
• no other causative disorder
Primary or secondary
Secondary headache?
(ie, caused by another disorder):
• new headache occurring in close temporal
relation to another disorder that is a known
cause of headache
• coded as attributed to that disorder
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
Diagnosis
Primary
Headache only
Primary and
Secondary
Temporal relation of
the other disorder to
headache worsening
Loose
Close
Degree of worsening
Slight
Marked
Evidence disorder
causes secondary
headaches
Weak
Strong
Other disorder
eliminated
Headache
unchanged
Headache
improves
The Headaches, 3rd edition. Lippincott Williams and Wilkins 2006
5. Headache attributed to
head and/or neck trauma
5.1 Acute post-traumatic headache
5.2 Chronic
post-traumaticattributed
headache
5. Headache
to
5.3 Acute headache attributed to whiplash injury
head
and/or
neck
trauma
5.4 Chronic headache attributed to whiplash injury
5.5 Headache attributed to traumatic intracranial
haematoma
5.6 Headache attributed to other head and/or neck
trauma
5.7 Post-craniotomy headache
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
Secondary headache after injury
Should begin within 7 days of head
injury (to meet IHS criteria)
Consider diagnosis: subdural, CSF
leak, dissection
Headaches may resemble primary
headache disorders (i.e. migraine,
tension)
Often assoc with other “postconcussive” symptoms: vertigo,
tinnitus, cognitive changes, sleep
problems, depression, medication
overuse
There is no evidence-based
approach and no guidelines
6. Headache attributed to cranial
or cervical vascular disorder
6.1 Headache attributed to ischaemic stroke or
transient ischaemic attack
Up to 1/3 pts with stroke
6.2 Headache attributed to non-traumatic intracranial
haemorrhage
6.3 Headache attributed to unruptured vascular
malformation
6.4 Headache attributed to arteritis
6.5 Carotid or vertebral artery pain
6.6 Headache attributed to cerebral venous thrombosis
6.7 Headache attributed to other intracranial vascular
disorder
6. Headache attributed to
cranial or cervical vascular
disorder
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
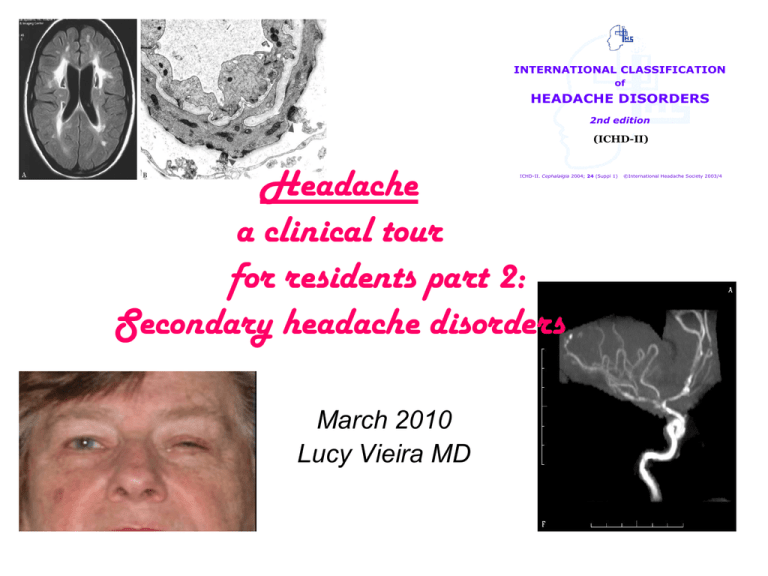
-anterior communicating artery
(30-35%),
-the bifurcation of the internal
carotid and posterior
communicating artery (30-35%) -the bifurcation of the middle
cerebral artery (20%)
-bifurcation of the basilar artery,
and the remaining posterior
circulation arteries (5%)
Utility of CT and LP in SAH
• CT: 90-95% sensitivity within 24h
• 80% at 3 days, 50% at 1 week.
• MRI FLAIR (3-14 d more sensitive than CT)
• LP may be negative less than 2 hours after the bleed;
– most sensitive at 12 hours after symptom onset.
– Xanthochromia (yellow-to-pink CSF supernatant)
usually is seen by 12 hours
Symptoms
•
•
•
•
Headache
Neck stiffness
n/v, photophobia
Mental status
85-95%
74-84%
48%
43%
• Less common:
– Focal deficit, seizures, coma, CN palsy, papilledema, ocular
hemorrhage
*sentinel bleed
First primary sexual or exertional
headache
• SAH has to be excluded as 1/3 of SAHs
occur during activities such as bending,
lifting, defecation or sexual intercourse.
Case 1
• 44 year old woman
• right sided headache and facial pain
• Onset to peak pain – 1-2 minutes
– 1 week ago
• Characterized as an intense aching throb “unlike
my other headaches”
• Associated with intermittent right sided pulsatile
tinnitus
adapted from D. Capobianco June 2006 AHS and Wityk, R. J. JAMA 2001;285:2757-2762
• Why coming now to MD?
– “My husband thought I should because of
ringing in my ear.”
• Phx: migraine with/without aura
• Neurological exam: normal
• Ct scan and LP normal. Sent home after getting a
little better with metoclopramide and meperidine
IV.
• Next day driving car and started to drive on the
median and eventually taken to hospital by the
police. There she was found to have a subtle right
Horner's syndrome, mild slowing of left fine finger
movements and left visual extinction.
• A diagnostic test was done
Imaging of Stroke
Wityk, R. J. JAMA 2001;285:2757-2762.
Copyright restrictions may apply.
Anatomy of Carotid Artery Dissection
2cm distal to carotid origin
-ends at skull base
Subintimal dissection
-stenosis
Mickey mouse ears:
expansion by hyperintense
hematoma of the outer
lumen of the artery
Wityk, R. J. JAMA 2001;285:2757-2762.
Copyright restrictions may apply.
Carotid Dissection
• Fronto-orbital headache before ischemia: 55-100%
• Painful Horner’s, Painful tinnitus
• Carotid bruit, dysguesia, ipsilateral neck pain,
cerebral or retinal ischemia
• Triggers: cough, sneeze, trauma
• Risks: syphilis, Marfans, Ehlers-Danlos, FMD
• Prognosis: good (60% resolve spont.;85% do well)
37 year old after a motorcycle accident
Sara Mazzucco, MD; and Nicolo` Rizzuto, MD
Neurology 2006
cavernoma
MRI demonstrating a left-sided cavernoma (a and b) with an associated
developmental venous anomaly (c) in the dorsal midbrain region adjacent to the
periaqueductal grey matter.
Cephalalgia, Vol. 22, No. 2, 107-111 (2002)
MS
MS patients with a plaque located within
the midbrain, in proximity to the PAG,
showed a four-fold increase in migrainelike headaches (odds ratio 3.91, 95%
confidence interval 2.01 to 7.32; P <
.0001) when compared to MS patients
without a plaque in this location
Headache 2005 Jun;45(6):670-7
occipital arteriovenous
malformation
34-year-old man started to
experience monthly headaches:
visual prodrome consisting of
scintillating bright lights in the
left visual field that slowly
expanded over several minutes.
Shortly after the visual symptom
subsided, right-sided throbbing
headaches developed along
with nausea and vomiting,
which usually lasted 2 to 4
hours. Normal neuro exam.
He was treated by radiosurgery
with obliteration of the AVM and
resolution of the headaches
Kurita, H. et al. Arch Neurol 2000;57:1219
CASE IN THE ER
A 23 year-old man with known migraine
Cc: generalized tonic-clonic seizure.
He had a second seizure in the emergency room.
He complained of severe dull occipital headaches of
recent onset, different from his usual migraines. He
denied head injury.
Clinical examination was unremarkable.
CT brain was significant for hemorrhage in the left
frontal lobe and MRI shows bi-frontal (parasagital)
hemorrhages.
Erle C.H. Lim, Raymond C.S. Seet: Sudden-Onset Headache And Seizures In A Young Man. The
Internet Journal of Neurology. 2005. Volume 4 Number 2
6.6 Cerebral Venous Sinus thrombosis
5 patterns of presentation
1. Isolated Intracranial hypertension
1. Progressive onset over days to weeks
2. Papilledema
3. CN6 palsy, tinnitus, visual obscurations
2. Venous infarction with focal signs
1. Mimics arterial stroke
2. Chronic and progressive like a tumor or abscess
3. Subacute encephalopathy
1. Diffuse HA with decr LOC
2. Focal signs
3. Seizures
4. +/-papilledema
4. Cavernous sinus thrombosis
1. Frontal headache
2. Chemosis, proptosis, opthalmoparesis
5. Thunderclap headache mimics SAH
Secondary causes of CVST
• Hypercoagable state
– Factor V Leiden, Protein C & S,ATIII
deficiency, prothrombin gene
mutation,etc
•
•
•
•
•
Cancer
Sepsis, dehydration, infections
Behcet’s
SLE
Estrogen – pregnancy, puerperium
6.4 Headache attributed to
arteritis
6.4.1
Headache
attributedattributed
to giant cell arteritis
6.4
Headache
to
(GCA)
arteritis
6.4.2 Headache attributed
to primary central
nervous system (CNS) angiitis
6.4.3 Headache attributed to secondary central
nervous system (CNS) angiitis
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
Arteritis Headache
• Cerebral vasculitis
–
–
–
–
–
Primary angiitis of the CNS
AIDS, zoster
Fungal, viral, parasitic, treponemal meningitis
Drug related - amphetamines, cocaine,
Lymphoma (angioendotheliosis)
• Systemic vasculitis
–
–
–
–
–
Behcet’s - genital ulcers, arthritis, eye
PAN - fever, arthralgias, myalgias, mononeuropathies
Churg-Strauss - asthma, eosinophilia, neuropathy
Wegener’s – lower/upper resp, ANCA, neuropathy
SLE - fever, rash, arthritis, pleuritis, encephalopathy
6.4.1 Headache attributed to giant
cell arteritis
A. Any new persisting headache fulfilling criteria C and D
B. At least one of the following:
1. swollen tender scalp artery with elevated
erythrocyte sedimentation rate (ESR) and/or
C reactive protein (CRP)
2. temporal artery biopsy demonstrating giant cell
arteritis
C. Headache develops in close temporal relation to other
symptoms and signs of giant cell arteritis
D. Headache resolves or greatly improves within 3 d of
high-dose steroid treatment
6.4.1 Headache attributed to
giant cell arteritis
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
GCA
• Rare: 15/100000 adults>50
• (mean age 70)
• Steroid responsive patchy granulomatous
vasculitis of BV media with destruction of the
internal elastic lamina.
• Esp involves: superficial temporal, posterior
ciliary, ophthalmic and vertebral arteries
(parallels amount of elastic tissue in the media)
• Usually not involve intradural BVs.
• PMR
• Most common symptom: new headache in
older pt.
• Local symptoms: headache, visual loss,
temporal artery ( beading, irregularities,
tenderness, pulselessness), jaw
claudication and scalp tenderness.
• Systemic symptoms: fever, weight loss,
PMR
Schmerling RH JAMA 2006 295: 2525-2534
Table. Clinical Predictors of Temporal Arteritis
__
Likelihood Ratio
Variable
(95% Confidence Interval)
Positive
Negative
Symptoms and Signs
Beaded temporal artery
Prominent or enlarged temporal artery
Tender temporal artery
Absent temporal artery pulse
Any temporal artery finding
Diploplia
Jaw claudication
4.6 (1.1-18.4)
4.3 (2.1-8.9)
2.6 (1.9-3.7)
2.7 (0.55-13.4)
2.0 (1.4-3.0)
3.4 (1.3-8.6)
4.2 (2.8-6.2)
0.93 (0.88-0.99)
0.67 (0.5-0.89)
0.82 (0.74-0.92)
0.71 (0.38-1.3)
0.53 (0.38-0.75)
0.95 (0.91-0.99)
0.72 (0.65-0.81)
Laboratory Data
Erythrocyte sedimentation rate
normal
>50 mm/h
>100 mm/h
1.1 (1.02-1.2)
1.2 (1.0-1.4)
1.9 (1.1-3.3)
0.2 (0.08-0.51)
0.35 (0.18-0.67)
0.8 (0.68-0.95)
Schmerling RH JAMA 2006-295
6.7 Headache attributed to other
intracranial vascular disorder
6.7.1
Cerebral
Autosomal Dominant
6.7
Headache
attributed to
Arteriopathy with Subcortical Infarcts and
other intracranial
vascular
Leukoencephalopathy
(CADASIL)
6.7.2 Mitochondrial
Encephalopathy, Lactic
disorder
Acidosis and Stroke-like episodes (MELAS)
6.7.3 Headache attributed to benign angiopathy
of the central nervous system
6.7.4 Headache attributed to pituitary apoplexy
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
6.7.1 CADASIL
A. Attacks of migraine with aura, with or without other
neurological signs
B. Typical white matter changes on MRI T2WI
C. Diagnostic confirmation from skin biopsy evidence or
genetic testing (Notch 3 mutations) (Chrom. 19)
6.7.1 CADASIL
*Migraine with aura in 1/3 and may precede MRI
changes up to 15 y.
*Typical aura except higher freq. long auras and can
©International
Headache Society 2003/4
be hemiplegic or
basilar-like.
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
Figure 1a. Transverse FLAIR MR images
Auer, D. P. et al. Radiology 2001;218:443-451
Copyright ©Radiological Society of North America, 2001
Figure. Fluid-attenuated inversion recovery MRI scans from a patient with a notch3
mutation shows typical involvement of the anterior temporal poles (arrow in A) and the
external capsule (arrow in B), and characteristic images at the level of the lateral ventricles
(C)
Markus, H. S. et al. Neurology 2002;59:1134-1138
Figure. (A) FLAIR MR image showing extensive white matter signal hyperintensities in
temporopolar regions and cystic changes
Smith, B. W. et al. Neurology 2002;59:961
6.7.3 Benign or Reversible Angiopathy (reversible vasoconstriction)
Diffuse severe HA (can be TCH), string and beads on MRA, CSF normal, 1-2months
**confused with SAH and with vasculitis**
Associated conditions
Pregnancy and puerperium
Early puerperium, late pregnancy, eclampsia, preeclampsia, and delayed
postpartum eclampsia
Exposure to drugs and blood products
Phenylpropanolamine, pseudoephedrine, ergotamine tartrate, methergine,
bromocriptine, lisuride, selective serotonin reuptake inhibitors,
sumatriptan, isometheptine, cocaine, ecstasy, amphetamine derivatives,
marijuana, lysergic acid diethylamide, tacrolimus (FK-506),
cyclophosphamide, erythropoetin, intravenous immune globulin, and
red blood cell transfusions
Miscellaneous
Hypercalcemia, porphyria, pheochromocytoma, bronchial carcinoid tumor,
unruptured saccular cerebral aneurysm, head trauma, spinal subdural
hematoma, postcarotid endarterectomy, and neurosurgical procedures
Idiopathic
No identifiable precipitating factor
Associated with headache disorders, such as migraine, primary
thunderclap headache, benign exertional headache, benign sexual
headache, and primary cough headache
Singhal AB, Bernstein RA. Neurocrit Care. 2005;3:91-7.
Clinical features
•CTA or MRA documenting multifocal segmental cerebral artery
vasoconstriction
•No evidence for aneurysmal subarachnoid hemorrhage
•Normal or near-normal cerebrospinal fluid analysis
•Severe, acute headaches, with or without additional neurologic signs or
symptoms
•Reversibility of angiographic abnormalities within 12 weeks after onset.
Leonard H. Calabrese, DO; David W. Dodick, MD; Todd J. Schwedt, MD; and Aneesh B. Singhal, MD
Ann Intern Med. 2007;146:34-44.
ESR
GCA
CSF
N
Primary CNS
angiitis
N
ALWAYS
ABNORMAL
Benign CNS
angiopathy
N
N
FHM
N
+/-
7.
7. Headache
Headache attributed
attributed to
to
non-vascular
non-vascular intracranial
intracranial disorder
disorder
7.1
7.1 Headache
Headache attributed
attributed to
to high
high cerebrospinal
cerebrospinal fluid
fluid pressure
pressure
7.2
7.2 Headache
Headache attributed
attributed to
to low
low cerebrospinal
cerebrospinal fluid
fluid pressure
pressure
7.3
7.3 Headache
Headache attributed
attributed to
to non-infectious
non-infectious inflammatory
inflammatory
disease
disease
7.4
7.4 Headache
Headache attributed
attributed to
to intracranial
intracranial neoplasm
neoplasm
7.5
7.5 Headache
Headache attributed
attributed to
to intrathecal
intrathecal injection
injection
7.6
7.6 Headache
Headache attributed
attributed to
to epileptic
epileptic seizure
seizure
7.7 Headache attributed to Chiari malformation type I
7.8 Syndrome of transient Headache and Neurological
Deficits with cerebrospinal fluid Lymphocytosis (HaNDL)
7.9 Headache attributed to other non-vascular intracranial
disorder
7. Headache attributed to
non-vascular intracranial
disorder
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
7.1.1 Headache attributed to IIH
A. Progressive headache with 1 of the following
characteristics and fulfilling criteria C and D:
1. daily occurrence
2. diffuse and/or constant (non-pulsating) pain
3. aggravated by coughing or straining
B. Intracranial hypertension (criteria on next slide)
C. Headache develops in close temporal relation to
increased intracranial pressure
D. Headache improves after withdrawal of CSF to reduce
pressure to 120-170 mm H2O and resolves within 72 h
of persistent normalisation of intracranial pressure
7.1.1 Headache attributed to
IIH
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
7.1.1 Headache attributed to IIH
A. Diffuse constant headache worsened by coughing or straining
B. Intracranial hypertension fulfilling the following criteria:
1. alert patient with neurological examination that either is normal or
demonstrates any of the following abnormalities:
a) papilloedema
b) enlarged blind spot
c) visual field defect (progressive if untreated)
d) sixth nerve palsy
2. increased CSF pressure (>200 mm H2O [non-obese], >250 mm
H2O [obese]) measured by lumbar puncture in the recumbent
position or by epidural or intraventricular pressure monitoring
3. normal CSF chemistry (low CSF protein acceptable) and cellularity
4. intracranial diseases (including venous sinus thrombosis) ruled out
by appropriate investigations
5. no metabolic, toxic or hormonal cause of intracranial hypertension
7.1.1 Headache attributed to
IIH
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
MRI images
Pathophysiology
• Disorder of homeostasis where there may
be:
–
–
–
–
Increased brain water content
Incr. cerebral blood volume
Incr CSF production
Venous outflow obstruction (increased
resistance to CSF outflow)
Secondary causes
Disruption of outflow
-venous thrombosis, dural fistula
-radical neck dissection
-right heart failure
-COPD
-(obesity)
Hormonal
-hypoparathyroidism
-hyper/hypothyroidism
-Cushing's ?Addison's
-PCO
Toxins/meds
-vitamin A
-Nalidixic acid,tetracycline,nitrofurantoin,indocid,steroids/withdrawal,others
Medical conditions
CRF, SLE, Anemia/polycythemia
Infectiousmeningitis,encephalitis,Lyme,HIV
Trauma
CASE
40-year-old woman:
posterior neck pain and orthostatic
headaches (severe at times, dull or
throbbing), worse with cough.
Tinnitus, and distortion of hearing.
Neurologic examination normal.
Head MRI showed….
Classic
Brain MRI
features
Diffuse pachymeningeal enhancement (T1 with gado)
Descent of the brain – tonsils, loss of cisterns, post fossa crowding
Pituitary Enlargement
Flattening of the chiasm
Subdural collections
Engorged venous sinuses and small ventricles.
CSF opening pressure was
3cm H2O
A lumbar epidural blood patch
offered no relief.
Myelo –
meningeal
diverticulum
Water-soluble
myelogram/CT-myelogram
showed frank extravasation
of contrast to the paraspinal
soft tissues at the L C7 root
sleeve.
Subsequently, the leak was
surgically repaired via a left
sixth through seventh
cervical hemilaminectomy
B. Mokri Mayo Clin Proc. 1999;74:1113-1123
7.2 Headache attributed to
low cerebrospinal fluid pressure
7.2 Headache attributed to
7.2.1 Post-dural puncture headache
lowfistula
cerebrospinal
fluid
7.2.2 CSF
headache
pressure
7.2.3 Headache attributed
to spontaneous (or
idiopathic) low CSF pressure
(CSF below 5-9 cm H2O)
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
7.2.1 Post-dural (post-lumbar)
puncture headache
A. Headache that worsens within 15 min after sitting or
standing and improves within 15 min after lying, with
1 of the following and fulfilling criteria C and D:
1. neck stiffness; 2. tinnitus; 3. hypacusia;
4. photophobia; 5. nausea
B. Dural puncture has been performed
C. Headache develops within 5 d after dural puncture
D. Headache resolves either:
1. spontaneously within 1 wk
2. within 48 h after effective treatment of the spinal
fluid leak
7.2.1 Post-dural (post-lumbar)
puncture headache
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
47 year old executive, father of 3.
According to wife had a longstanding history
of migraine.
Headache continuous for 9 weeks and taking
daily analgesics.
Presented to the ER on the weekend as
headache no longer responding.
Had been working until the Friday before.
In ER, physician described that the patient
was behaving in a bizarre fashion, seemed
agitated and inconsolable..?drug seeking.
Given Maxeran then Dilaudid then Toradol
with no improvement.
The next morning a CT scan of the brain was
ordered…
Nice couple completely convinced that this
was a terrible migraine that would eventually
improve.
Patient unable to lie down. Sitting in the
chair grabbing his head and intermittently
crying out in pain.
Unable to answer direct questions on
orientation and distractible.
Pupils equal and reactive. Left babinski.
Decreased LOC
Hypertension/bradycardia?
Ipsilateral parasympathetic dysfunction
(dilated pupil)…
8.1.1 – NO donor: NTG, nitrates, nitrites
8.1.2 – Phosphodiesterase inhibitor: Viagra,
etc – migraineurs most at risk; lower doses
better.
10.1 Headache attributed to
hypoxia and/or hypercapnia
10.1 Headache attributed to
10.1.1 High-altitude headache
hypoxia
and/or
hypercapnia
10.1.2 Diving headache
10.1.3 Sleep apnoea headache
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
10.3 Headache attributed to
arterial hypertension
10.3.1 Headache attributed to phaeochromocytoma
10.3.2
Headache
attributed to
hypertensive crisis
10.3
Headache
attributed
to
without hypertensive encephalopathy
arterial
hypertension
10.3.3 Headache
attributed
to hypertensive
encephalopathy
10.3.4 Headache attributed to pre-eclampsia
10.3.5 Headache attributed to eclampsia
10.3.6 Headache attributed to acute pressor
response to an exogenous agent
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
11. Headache or facial pain attributed to
disorder of cranium, neck, eyes, ears, nose,
sinuses, teeth, mouth or other facial or
cranial structures
11. Headache
or facial pain
attributed
to disorder
of cranium,
11.1 Headache
attributed
to disorder
of cranial bone
11.2 Headache
attributed
to disorder
neck
neck, eyes,
ears,
nose, of
sinuses,
11.3 Headache attributed to disorder of eyes
mouth
or other
facialofor
cranial
11.4teeth,
Headache
attributed
to disorder
ears
structures
11.5 Headache attributed
to rhinosinusitis
11.6 Headache attributed to disorder of teeth, jaws or
related structures
11.7 Headache or facial pain attributed to
temporomandibular joint (TMJ) disorder
11.8 Headache attributed to other disorder of the above
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
Part 3:
Cranial neuralgias, central
and primary
facial
pain
and
Part 3:
other headaches
Cranial neuralgias, central and
primary
facial
pain
and
other
13. Cranial neuralgias and central causes of
facial pain headaches
14. Other headache, cranial neuralgia, central or
primary facial pain
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
13. Cranial neuralgias and
central causes of facial pain
13.1 Trigeminal neuralgia
13.2 Glossopharyngeal neuralgia
13.313.
Nervus
intermedius
neuralgia and
Cranial
neuralgias
13.4 Superior laryngeal neuralgia
central
causes
13.5
Nasociliary
neuralgiaof facial pain
13.6 Supraorbital neuralgia
13.7 Other terminal branch neuralgias
13.8 Occipital neuralgia
13.9 Neck-tongue syndrome
13.10 External compression headache
13.11 Cold-stimulus headache
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
13. Cranial neuralgias and
central causes of facial pain
13.12 Constant pain caused by compression,
irritation or distortion of cranial nerves or upper
cervical
by structural
lesions
13. roots
Cranial
neuralgias
and
13.13 Optic neuritis
causes
of facial pain
13.14central
Ocular diabetic
neuropathy
13.15 Head or facial pain attributed to herpes zoster
13.16 Tolosa-Hunt syndrome
13.17 Ophthalmoplegic ‘migraine’
13.18 Central causes of facial pain
13.19 Other cranial neuralgia or other centrally
mediated facial pain
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4
14.2 Headache unspecified
A. Headache is or has been present
14.2 Headache unspecified
B. Not enough information is available to classify the
headache at any level of this classification
WE don’t need to use this code most of the time!
ICHD-II. Cephalalgia 2004; 24 (Suppl 1)
©International Headache Society 2003/4