file
advertisement
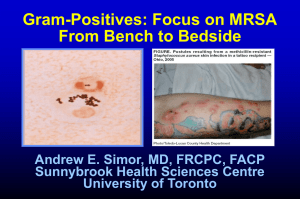
Antibiotic Basics Steven Bradley, MD Harborview Chief Medical Resident Inpatient Services Antimicrobial Considerations 1. 2. Likely organism and susceptibilities Site of infection - SSTI, bacteremia, pneumonia, meningitis, UTI 3. Host factors - Immune deficiencies, age, allergies, renal and hepatic function 4. Antimicrobial factors - Dosage, route, drug interactions, tissue penetration, toxicity, cost 5. Public health considerations - Selection of resistance Antimicrobial Case 1 20 yo woman presents with 3 days of fever, sore throat, and cervical adenopathy. Rapid strep test is positive. What is the preferred therapy? A. Azithromycin for 5 days B. Penicillin V for 10 days C. Levofloxacin 500 mg for 10 days D. Vancomycin 1 gm BID for 7 days Antimicrobials: Site of Action Cell Wall - Beta-Lactams - Glycopeptides Cell Membrane - Daptomycin - Polymixin DNA Inhibitor - Fluoroquinolone - TMP-SMX - Metronidazole Protein Synthesis 50S Ribosome - Macrolides/Ketolides - Clindamycin - Chloramphenicol - Quinupristin-Dalfopristin 30S Ribosome - Aminoglycosides - Tetracyclines - Glycylcyclines 70S Initiation Complex - Linezolid Adapted from David Spach, MD Bacteria: Cell Wall Synthesis Cell Wall Synthesis Penicillin Binding Proteins Penicillin Binding Protein DNA Cell Membrane Cell Wall Adapted from David Spach,MD Beta-lactam Antimicrobials Penicillins Cephalosporins Carbapenems Monobactams Site of β-lactamase Activity O R1 C S NH HC H 2C C N O β-lactamase CH3 C CH3 C COOH Beta-Lactam: Mechanism of Action Cell Wall Synthesis Beta-Lactam DNA Cell Membrane Penicillin Binding Proteins Cell Wall Adapted from David Spach, MD Penicillins Penicillin G and penicillin V Aminopenicillins Streptococcus pyogenes Pharyngitis, syphilis Ampicillin and amoxicillin H. influenzae, Enterococcus, Listeria Acute otitis media, acute bacterial sinusitis Penicillinase-resistant penicillins Methicillin, nafcillin, oxacillin, dicloxacillin Staphylococcus aureus (MSSA), Streptococcus No gram-negative activity SSTI, osteomyelitis, septic arthritis Extended-spectrum Penicillins Carboxypenicillins (Ticarcillin) Ureidopenicillins (Piperacillin) Gram-negative coverage including Pseudomonas Gram-negative coverage including Pseudomonas Penicillin β-lactamase inhibitor combinations Amox-clav, amp-sulb, ticar-clav, pip-tazo Increase Staphylococcus and anaerobic coverage Increasing Gram-negative Coverage First Generation Second Generation Cefuroxime Cefamycins: cefoxitin, cefotetan Third Generation Cefazolin, cephalexin Ceftriaxone, ceftazidime Fourth Generation Cefepime Increasing Gram-positive Coverage Cephalosporins Carbapenems Imipenem/cilastin, meropenem Ertapenem Broad spectrum of activity including Pseudomonas Meropenem less likely to provoke seizures Not active against Pseudomonas, Acinetobacter, and Enterococcus faecalis Most reliable activity against ESBL and ampC containing organisms Monobactams Aztreonam Activity restricted to aerobic gramnegative bacteria including most Pseudomonas Does not display cross-reactive hypersensitivity reactions in patients with penicillin allergies Beta-Lactam Allergy 10-20% of those reporting PCN allergy are truly allergic when assessed by skin testing Potential cross-reactivity with cephalosporins (8%) and carbapenems, but not monobactams Skin test for major (benzylpenicilloyl polylysine) and minor determinants Positive predictive value of 14% Positive skin test: 41-67% risk of significant allergy Negative skin test: 1-4% risk, none life threatening Desensitization when no other options Antimicrobial Case 1 20 yo woman presents with 3 days of fever, sore throat, and cervical adenopathy. Rapid strep test is positive. What is the preferred therapy? A. Azithromycin for 5 days B. Penicillin V for 10 days C. Levofloxacin 500 mg for 10 days D. Vancomycin 1 gm BID for 7 days Antimicrobial Case 2 45 y o woman presents with 3 day history of acute onset of fever 39 C, chills, cough productive of green phlegm, SOB, and right-sided chest pain. CXR demonstrates RLL infiltrate. Community-Acquired Pneumonia Most common pathogens S. pneumoniae, H. influenzae, Moraxella with concern for C. pneumonia, M. pneumoniae, and Legionella 2002-2003 US Survey revealed 34% nonsusceptible (16% intermediate, 18% resistant) WA 2003: 16% intermediate, 7% resistant S. pneumoniae do not produce beta-lactamase Alteration in penicillin binding protein with decreased affinity for beta-lactam Beta-lactamase inhibitors (clavulanate or sulbactam) will not improve efficacy Streptococcus pneumoniae Resistance Antimicrobial Percent Resistant Macrolide 29% TMP/SMX 32% Tetracyclines *21.9% of 16% S. pneumoniae isolates in 2002-2003 had fluoroquinolone mutations in parC and/or gyrA compared to 4.7% in 1997-1998. Fluoroquinolones* 2.3% Clin Infect Dis 2005;41:139-48 Community-Acquired Pneumonia Outpatient Macrolide or doxycycline Respiratory fluoroquinolone, if recent antimicrobial tx Inpatient medical ward -lactam + macrolide vs. fluoroquinolone Retrospective analysis of 14,000 Medicare patients found lower mortality with cephalosporin + macrolide or fluoroquinolone compared to cephalosporin alone (Arch Intern Med 1999;159:2562-72) Lower in-hospital mortality among patients with bacteremic pneumococcal pneumonia treated with lactam + macrolide compared to -lactam alone (Clin Infect Dis 2003;36:389-95) Clin Infect Dis 2003;37:1405-33. Fluoroquinolone: Mechanism of Action Fluoroquinolone DNA Topoisomerase IV DNA Gyrase DNA Cell Membrane Cell Wall Adapted from David Spach, MD Fluoroquinolones Concentration-dependent killing (AUC:MIC) Moxifloxacin is hepatically eliminated, not for urinary infections Adverse events GI CNS Photosensitivity Prolonged QTc Tendonitis/arthropathies Hyperglycemia or hypoglycemia, particularly elderly with DM S. pneumoniae and Fluoroquinolones Drug MIC90 AUCFree AUC:MICFree Ciprofloxacin (750 bid) Levofloxacin (500 qd) Levofloxacin (750 qd) Gatifloxacin (400 qd) Gemifloxacin (320 qd) 280 Moxifloxacin (400 qd) 1.0 1.0 1.0 0.25 0.03 28 34 70 26 28 34 70 106 140- 0.12 24 200 Cutoff criterion of AUC:MIC >33.7 for gram-positives? Clin Infect Dis 2005;41:S127-35 High-dose, Short-course Levofloxacin for CAP Attempt to increase AUC:MIC ratio while decreasing overall drug exposure Multi-center, randomized, double-blind study comparing 750 mg qd x 5 days vs. 500 mg qd x 10 days in the treatment of CAP Found equivalent clinical and microbiological outcomes Clin Infect Dis 2003;37:752-60 Case Modified The patient decompensated and required intubation. He became afebrile after 48 hours. They remained intubated at 96 hours and developed a new fever and infiltrate on CXR. What infection are you concerned for? What pathogens need to be considered in this setting? What antibiotic choices are appropriate? Nosocomial Pneumonia/Ventilator Associated Pneumonia Common pathogens include coliforms, Staph and Pseudomonas aeruginosa Coverage should now cover broadly for gram positives, gram negatives, and Pseudomonas Anti-pseudomonal penicillin (pip/tazo) or fluoroquinolone MRSA coverage (vanco) Eight day therapy equivalent to 14 day Pseudomonas and Fluoroquinolones Drug Dose Ciprofloxacin 400 400 750 400 400 Levofloxacin Gatifloxacin Moxifloxacin q12 q8 q24 q12 q24 Cmax 4.1 4.1 12.1 4.6 4.2 MIC 0.125 0.125 0.5 1.0 2.0 AUCfree:MIC 144 184 152 28 10 New IDSA and ATS Guidelines for HAP/VAP recommend Ciprofloxacin 400mg IV q8hr or Levofloxacin 750 mg qd Am J Respir Crit Care Med 2005;171:388-416 Antimicrobial Case 6 20 y o woman presents with 2 day h/o dysuria, urgency, and frequency. UA with >50 WBC/hpf, +leukocyte esterase Cystitis treatment options: Amoxicillin, 40-50% resistance among E. coli Nitrofurantoin x 7 days -cystitis only, does not achieve adequate blood levels TMP-SMX x 3 days, though increasing resistance -culture selection bias reflecting hospital setting -85% predicted clinical cure rate with 30% resistance Fluoroquinolone, ? if >10-20% resistance to TMP-SMX Clin Infect Dis 1999;29:745-58 Antimicrobial Case #3 What if this patient was 75 and had a chronic foley catheter? Complicated UTI In the setting of obstruction (BPH), reflux, catheter Similar pathogen profile Enterobacteriaceae (E.coli), enterococci Nosocomial bugs Treat for extended period (2 weeks) and remove obstruction if possible Beware of asymptomatic bacteruria Treatment leads to resistance Antimicrobial Case 5 35 y o man with a history of methamphetamine use presents to clinic with a right biceps abscess. Previous “Standard of Care” If abscess appreciated, I&D performed without culturing Depending on severity of SSTI, either admitted for IV beta-lactam (cefazolin or nafcillin), or discharged empirically on cephelexin without concern for resistant organisms This approach is no longer appropriate Proportion of S. aureus Nosocomial Infections Resistant to Oxacillin (MRSA) Among Intensive Care Unit Patients, 1989-2003* Percent Resistance 70 60 50 40 30 20 10 0 1989 1991 1993 1995 1997 1999 2001 Year *Source: NNIS System, data for 2003 are incomplete 2003 Community-Associated MRSA Clinical manifestations Predominantly skin and soft tissue Necrotizing fasciitis Necrotizing pneumonia (JAMA 2003;290:2976-2984) 53) 2005;40:100-7) Different (N Engl J Med 2005;352:1445(Clin Infect Dis from HA-MRSA Panton-Valentine Leukocidin exotoxin associated with tissue necrosis and leukocyte destruction (JAMA 2003;290:2976-2984) Nasal Carriage of S. aureus 20-40% of people colonized with S. aureus –20% persistent, 60% intermittent, 20% never Increased Rates of MRSA Healthcare contact Surgery Dialysis Indwelling devices IDDM HIV Long-term care facilities IDU (Clin Infect Dis 2002;34:425-33) Correction facilities (Clin Infect Dis 2003;37:1384-8) MSM (Clin Infect Dis 2005;40:1529-34) Native Americans, Pacific Islanders Other close contact Athletic (N Engl J Med 2005;352:468-75) Antimicrobial Susceptibility Patterns Clindamycin Erythromycin Fluoroquinolone Rifampin 94 Tetracycline TMP/SMX Vancomycin JAMA 2003;290:2976-2984 CA-MRSA 83 44 79 96 92 95 100 HC-MRSA 21 9 16 92 90 100 Treatment Options for MRSA Infections Intravenous* Vancomycin Linezolid Daptomycin Quinupristin/dalfopr istin Tigecycline Oral* TMP-SMX Minocycline/Dox y Clindamycin Fluoroquinolone Linezolid *with or without rifampin, however NEVER use rifampin monotherapy due to rapid emergence of resistance TMP/SMX Mechanism The Folic Acid Pathway Sulfonamides PABA // Trimethroprim Dihydrofolic Acid Tetrahydropteroic acid synthetase // Tetrahydrofolic Acid Dihydrofolate reductase Adverse Events: -Hypersensitivity reaction -Marrow suppression -Hemolysis (G6PD deficiency) -Displace bilirubin from albumin Purines DNA Oxazolidinone: Mechanism of Action 50S Ribosome 30S Ribosome fMet-tRNA Oxazolidinone 50 S 30 S 70 S Initiation Complex DNA Modified from David Spach, MD Linezolid Oxazolidinone Active against MSSA, MRSA, VRSA, coag-neg Staph, S. pyogenes, S. pneumoniae, E. faecalis, E. faecium including VRE, as well as some Nocardia and mycobacteria Oral bioavailability 100% Adverse events: GI (nausea and vomiting) marrow suppression (thrombocytopenia, anemia, leukopenia) serotonin syndrome (weak monoamine oxidase inhibitor) lactic acidosis optic neuritis Linezolid-resistant VRE and MRSA reported due to mutation in 23S rRNA Concerns with Vancomycin Association between increasing MIC and clinical failure, particularly prolonged bacteremia Monitoring of serum levels No clear relationship between level, efficacy and toxicity Routine monitoring not necessary Changing renal function or renal insufficiency Peak levels should not be measured as vancomycin is not “concentration-dependent” Trough of 15-20 mg/L in endocarditis, osteomyelitis, and VAP though clinical data is limited Clin Infect Dis 2006;42:S51-7 Am J Respir Crit Care Med 2005;171:388-416 MRSA Nosocomial Pneumonia Retrospective analysis of a prospective, randomized, double-blind study Vancomycin +/- aztreonam vs. linezolid +/aztreonam Survival benefit with linezolid in the subset of patients with MRSA pneumonia Vancomycin group with higher rates of bacteremia and co-morbidities (cardiac, diabetes, renal) Role of toxin inhibition with linezolid or clindamycin? Awaiting prospective confirmation Chest 2003;124:1789-1797 Chest 2005;128:2732-2738 Antimicrobial Case X 60 yo male admitted to the hospital with one day history of fever, headache, photophobia, and neck stiffness. CSF reveals WBC 542 with neutrophil predominance, protein 90, and glucose 30. What empiric antibiotics should be started? Bacterial Meningitis Condition Pathogen Antimicrobials 2-50 years S. pneumoniae, N. meningitidis Vanco + ceftriaxone > 50 years S. pneumoniae, N. meningitidis, L. monocytogenes Vanco + ceftriaxone+ amp Post-neuroSurgery Gram-neg (Pseudomonas), S. aureus, Coag-neg Staph < 1 month S. agalactiae, E. coli L. moncytogenes Clin Infect Dis 2004;29:1267-84 Ampicillin + cefotaxime Ampicillin +aminoglycoside Vanco + (cefepime, ceftazidime, or meropenem) Antimicrobial Case 4 70 y o woman with bronchitis treated with moxifloxacin who develops fever, abdominal pain, and profuse, watery, maloderous diarrhea. WBC 24K. Clostridium difficile Colonization Unintended consequence of antimicrobial therapy 3% healthy adults 20-40% of hospitalized patients Perturbation of competing flora Cephalosporins, clindamycin, and fluoroquinolones Recent reports of increasing frequency and severity Epidemic strain with 18-bp tcdC deletion and binary toxin Metronidazole or oral vancomycin 90% vs. 88% response rates (Lancet 1983;2:1043-6) ?Increasing recurrence and failure with metronidazole Clin Infect Dis 2005;40:1586-90 Clin Infect Dis 2005;40:1591-7 N Engl J Med 2005;353:2433-41 N Engl J Med 2005;353:2442-9 Metronidazole Reduced metabolites damage bacterial DNA Active against anaerobic gram-negative bacilli and most Clostridium Favored in management of C. difficile Absorbed well with good CSF penetration (used in CNS abscess as opposed to clindamycin which has poor CSF penetration) Adverse events: Nausea, metallic taste Disulfiram-like reaction Antimicrobial Case 7 42 y o sexually active man presents with 3 day h/o dysuria and purulent urethral discharge. Increasing fluoroquinolone resistance IM ceftriaxone or PO cefpodoxime 15% co-infection with Chlamydia -azithromycin or doxycycline Neisseria gonorrheae Bad Bugs, No Drugs Gram-positive bacteria MRSA and VRE Emergence of vancomycin-resistant S. aureus and linezolid-resistant Enterococcus Gram-negative bacteria Pan-resistant Acinetobacter and Pseudomonas Colistin/Polymixin E nephrotoxicity 20-30% neurotoxicity 7% Extended-spectrum β-lactamase organisms Clin Infect Dis 2006;42:657-68 Antimicrobial Principles Judicious use of antimicrobial therapy to optimize clinical outcomes while minimizing unintended consequences Toxicity, drug-drug interactions Emergence of resistance C. difficile Understanding antimicrobial pharmocokinetics/dynamics and resistance mechanisms can help guide appropriate usage Knowledge of local susceptibility patterns is essential Development of antimicrobial resistance is directly related to antimicrobial usage Paucity of new drugs in the pipeline