Massive Transfusion Protocol in Trauma Why

Management of Massive
Bleeding in the ICU
Ibrahim Al-Sanouri, MD, FCCP, FAAAAI
Key Discussion Points
Definition
Complications of massive transfusion: coagulopathy.
Therapy goals
Haemostatic resuscitation
Introduction of Massive Transfusion (MMT) protocol and RBC:FFP:Plts ratio.
Bleeding in the ICU
Bleeding in the ICU: massive or not massive.
Mucosal or several.
Immediate or delayed.
GI bleed, Trauma or post surgical intervention
Massive blood transfusion: control the source
Definition of Massive Transfusion
Importance of Massive Transfusion
39% of trauma related deaths – uncontrollable bleeding
(Leading cause of preventable death)
1.
2.
2% of trauma patients – need massive transfusion
Bleeding 2 main causes
Vascular injury (surgical)
Coagulopathy (non-surgical)
Massive Blood Transfusion complications
Fluid overload
Thrombocytopnea
Hypocalcemia
Decreased oxygen release by transfused red cells due to 2,3-bisphosphoglycerate
(2,3-BPG) levels (left shift in Hg-O2 curve).
Hypothermia
Coagulopathy in massive bleeding:
Coagulopathy
Hypothermia
Haemorrhage
Haemodilution
Complications of massive transfusion
Hypotension
Resuscitation
Massive Blood Transfusion Management
Haemostatic Resuscitation
Fluid management
Metabolic acid base correction
Normal temperature
Calcium management
Therapeutic goals:
Maintenance of tissue perfusion and oxygenation by restoration of blood volume and haemoglobin.
Arrest of bleeding by treating any traumatic, surgical or obstetric source
Judicious use of blood component therapy to correct coagulopathy
Massive bleeding management
Treating team
Lab services
Blood products supplying service
1-Restore circulating volume:
Insert wide bore peripheral or central cannulae
Give pre-warmed crystalloid or colloid as needed, keep patient warm.
Avoid hypotension or urine output <0.5 ml/kg/h
Concealed blood loss is often underestimated
2Contact key personnel
A named senior person must take responsibility for communication and documentation.
Consultant anaesthetist
Blood transfusion Biomedical Scientist
Haematologist
Arrange Intensive Care Unit bed
3- Stop the bleeding:
Early surgical or obstetric intervention
Interventional radiology
4-Labs investigation:
CBC, PT, APTT, Thrombin time,
Fibrinogen, DIC profile.
Blood gases and pulse oximetry
Ensure correct sample identification
Repeat tests after blood component infusion
Results may be affected by colloid infusion
May need to give components before results available
5-Maintain Hb> 8 g.dl
Assess degree of urgency
Employ blood salvage to minimize allogeneic blood use
Give red cells
Group O Rh D negative In extreme emergency Until ABO and Rh D groups known
Use blood warmer and/or rapid infusion device if flow rate >50 ml/kg/h in adult
6Maintain adequate coagualtion
Anticipate platelet count <50 after 2 blood volume replacement.
Maintain PT & APTT < 1.5 · mean control
Give FFP 12 –15 ml/kg guided by tests
Anticipate need for FFP after 1 –1.5 blood volume replacement
Allow for 30 min thawing time
6-Maintain adequate coagulation
Maintain Fibrinogen > 1.0 g/l
If not corrected by FFP give cryoprecipitate (Two packs of pooled cryoprecipitate for an adult)
Allow for 30 min thawing time
Keep ionised Ca2+ > 1Æ13 mmol/l
7-Hospital protocol:
Multidisplinary services: Hospital
Transfusion Committee.
Improve awareness and confidence and ensure that the blood transfusion chain works efficiently.
Rapid communication cascade.
Safe and jusdicious use of blood components.
What is Haemostatic Resuscitation?
Prevents post massive transfusion coagulopathy.
Aims to reduce use of blood products in the intensive care phase.
With 5-7 unitis PRBC’s Plt count decreases to less than 50 %
With 5 units PRBC PT is increased to more than 1.5 control.
Haemostatic Resuscitation: RBC
Erythrocytes promote marginalization of platelets so the platelet concentrates along the endothelium and remains almost seven times that of the average blood concentration
Erythrocytes support thrombin generation by activating platelets by liberating ADP.
Oxygenation delivery.
Haemostatic Resuscitation: FFP
It remains controversial when and in what dose plasma should be transfused to massively bleeding trauma patients.
The optimal ratio of FFP to RBCs remains to be established: FFP:RBC ratio greater than 1:2 is associated with improved survival compared to one lower than 1:2.
Haemostatic Resuscitation: FFP
Meta-analysis from 2010-2012: Patients undergoing massive transfusion, high FFP to RBC ratios was associated with a significant reduction in the risk of death
(odds ratio (OR) 0.38 (95%CI 0.24-0.60) and multiorgan failure (OR 0.40 (95%CI
0.26-0.60).
Murad MH, Stubbs JR, Gandhi MJ, Wang AT, Paul A, Erwin PJ, Montori VM, Roback
JD: The effect of plasma transfusion on morbidity and mortality: a systematic review and meta-analysis. Transfusion 2010, 50:1370-1383
Haemostatic Resuscitation: FFP
Meta-analysis from 2012 reports of reduced mortality in trauma patients treated with the highest FFP or PLT to
RBC ratios.
Johansson PI, Oliveri R, Ostrowski SR: Hemostatic resuscitation with plasma and platelets in trauma. A meta-analysis. J Emerg Trauma Shock
2012, 5:120-125.
Coagulopathy of Massive Transfusion
Mortality Vs FFP/RBC ratio
Retrospective review of 246 patients receiving a massive transfusion (> 10 units of blood)
80%
60%
40%
20%
0%
65%
34%
19%
1:8 1:2.5 1:1.4
Borgman MA. et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital J trauma, 2007. 66:805-813
Haemostatic Resuscitation: Plts
Platelets are also pivotal for hemostasis: low Plts increases mortality.
The highest survival was established in patients who received both a high
PLT:RBC and a high FFP:RBC ratio.
Holcomb JB, Wade CE, Michalek JE, Chisholm GB, Zarzabal LA, Schreiber MA,
Gonzalez EA, Pomper GJ, Perkins JG, Spinella PC, Williams KL, Park MS: Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg 2008, 248:447-458.
Haemostatic Resuscitation: plt
Retrospective study of massively transfused patients: As apharesis platelet to RBC ratio increased, a stepwise improvement in survival was seen and a high apheresis PLT:RBC ratio was independently associated with improved survival.
Zink KA, Sambasivan CN, et al: A high ratio of plasma and platelets to packed red blood cells in the first 6 hours of massive transfusion
improves outcomes in a large multicenter study. Am J Surg 2009,
197: 565-570.
Massive transfusion protocols and ratios:
10 RBC, 4 FFP and 2 apheresis PLT for trauma patients.
211 trauma patients of who 94 received TEP and 117 were historic controls.
The TEP patients received more RBC (16 vs. 11), FFP (8 vs. 4), and PLT (2 vs. 1) intraoperatively than the controls.
The protocol group displayed lower 30-day mortality (51% vs. 66%).
After controlling for age, sex, mechanism of injury, Trauma and
Injury Severity Score (TRISS), and 24-hour blood product usage, a
74% reduction in the odds ratio of mortality was found among patients in the TEP group .
Cotton BA, Gunter OL, Isbell J, Au BK, Robertson AM, Morris JA: St Jacques P, Young PP:
Damage control hematology: the impact of a trauma exsanguination protocol on survival and blood product utilization. J Trauma 2008, 64:1177-1182.
Pre-defined Massive Transfusion Protocols are associated with REDUCTION of organ failure and post injury complication J Trauma 2009 Jan ; 66(1) 41-48
Ratio 10-4-2: RBC-FFP-PLts
24hr survival (%)
30d survival (%)
Hospital length of stay d (+/-SD)
ICU stay, (days)
Ventilator (days)
IO crystalloid, Litres
IO blood products units
24hr blood products
Pre-MMT (n-141)
61
37.6
16.4(+/-12.1)
6.6(+/-9.4)
8.2 (+/-9.7)
7L
11U
38.7U
MMT (n=129)
69
56.8
12 (+/-12.1)
5.0 (+/- 8.3)
5.7 (+/-7.2)
4.8L
14.7U
31.2U
P-values
0.185
0.001
0.049
0.239
0.017
<0.001
0.001
0.05
Complications comparison
Pre-MMT (n-141) MMT (n=129) P-values
Systemic inflammatory response syndrome
SIRS (%)
Severe sepsis/septic shock (%)
Ventilator-dependent respiratory failure(%)
55.3
19.8
62.4
52.8
10
60.8
0.682
0.019
0.787
VAP(%)
Abdominal compartment syndrome(%)
39
9.9
Open abdomen(%)
Need of Renal replacement therapy(%)
30.5
2.8
27.2
0
6.4
3.2
0.041
<0.001
<0.001
0.826
Pre-defined Massive Transfusion Protocols are associated with REDUCTION of organ failure and post injury complication J Trauma 2009 Jan ; 66(1) 41-48
Ratio 10-4-2: RBC-FFP-PLts
Fresh Whole Blood:
Routine use of fresh whole blood (FWB) for resuscitation of bleeding patients was abandoned in the civilian setting.
In the combat setting, however, FWB has been used.
In a report of US military patients in Iraq and Afghanistan from January 2004 to October 2007, those with hemorrhagic shock, a resuscitation strategy that included
FWB was associated with improved 30-day survival
(95% vs. 82%, p=0.002).
Spinella PC, Perkins JG, Grathwohl KW, Beekley AC, Holcomb JB: Warm fresh whole blood is independently associated with improved survival for patients with combat-related traumatic injuries. J Trauma 2009, 66:S69-S76.
Haemostatic Agents:
Antifibrinolytis:
Shakur H, et al: CRASH-2 Trial collaborators: Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant hemorrhage (CRASH-2): a randomized, placebo-controlled trial. Lancet 2010,
376:23-32.
Recombinant factor VII
: Hauser CJ at al: Results of the
CONTROL trial: efficacy and safety of recombinant activated Factor VII in the management of refractory traumatic hemorrhage. J Trauma 2010, 69:489-500.
Fibrinogen concentrate
Prothrombin complex concentrate
Hospital Alert:
Active Hemorrhage
SBP < 90
HR > 100
Ph < 7.35
BE < - 2
Uncontrollable active bleeding
Poor responder to fluid
Activation of MMT by team leader only- Registrar or above.
E
N
T
P
R
E
V
O
S
I
S
A
C
I
D
U
L
O
P
C
O
A
G
A
T
H
Y
T
H
E
R
H
Y
P
O
M
I
A
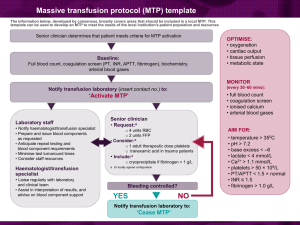
MANAGEMENT of MASSIVE TRANSFUSION (MMT) for
TRAUMA
Pre-hospital MMT alert:
• Systolic BP < 90
• Poor response to initial fluid resuscitation
• Suspected active haemorrhage
If so activate MMT (match 3 of the ocriteria)
MMT ACTIVATION
For Trauma
Hospital MMT alert confirmation
(patient requiring urgent transfusion)
- SBP < 90, - HR > 100
- Ph < 7.35
- BE < - 2
- Obvious signs of uncontrollable active bleeding
- Poor responder to fluid resuscitation
(Trauma Team leader must declare
MMT Activation to blood bank
,
Co-ordinate Porter urgently to standby for
Collection of MMT pack one
HAEMOSTASIS
PATIENT ARRIVAL
Take bloods (FBC, U&E, Clotting, fibrinogen and X-match and ABG)
Send pink bottle with X-match form to blood bank urgently ( please obtain 2 samples for x-match at different time if possible)
THERAPY TARGET end point:
HAEMORRHAGE CONTROL :
Surgery
Stabilize fractures
Pelvic brace
PREVENT HYPOTHERMIA
MMT PACK 1
4 x O –ve RBC ( female) or
O+ve(Male)
2 FFP
(or Group specific if possible)
HAEMOSTATIC DRUGS:
Consider the following if bleeding persist despite surgical interventions:
Activated factor VII
Beriplex (consider when patient who is on anti-coagulant)
Antifibrinolitic agents
Please discuss any of these therapeutic measures with Haematologist on call)
RE-ASSESSMENT
ABCDE
If haemorrhage continue
Activate MMT PACK 2
Please, specify location of patient
Fail to reach targets
Hb: 8-10 g/dl
Platelets > 100
PT&APTT (INR)< 1.5
Fibrinogen > 1.0 g/l
Ca² ⁺ > 1 mmol/l pH: 7.35-7.45
BE:
± 2
Tª > 36 °C
2 x packs of Cryoprecipitate if Fibrinogen is < 1.0 g/l
INTRA-OPERATIVE CELL SALVAGE:
Transfuse 1 x FFP every 250 ml of blood
Transfuse 1 x ATD platelets every 1000 ml of blood
4 X RBC
4 X FFP
MMT PACK 2
1 pharased
Platelets
Once administered check:
FBC, Clotting, fibrinogen and ABG
When MMT stops
Notify blood bank Return any unused products Resume standard ordering practices
Summery:
Immediate labs service is important to identify coagulopathy, and guide ongoing transfusion therapy.
Massive hemorrhage could results in serious life threatening complications
Massive bleeding and massive transfusion could lead to severe coagulaopthy which tight a viscous cycle that could cause mortality
Summery:
While resuscitation your patient keep patient warm with normal calcium level
Identify and correct source of bleeding.
Implementation of a homeostatic control resuscitation strategy to massively bleeding patients seems both reasonable and lifesaving.
Thank You!
Questions?