脑血管疾病
Cerebrovascular Disease
(CVD)
Department of Neurology
2nd hospital of Kunming Medical
University
Section 1 Introduction
Definition
CVD: The term of CVD designates
any abnormality of the brain
resulting from various pathological
process of the blood vessels.
脑血管病是各种脑血管病变引起脑
部疾病的总称。
Definition
Stroke: The stroke is a syndrome
characterized by the acute onset of a
neurologic deficit that reflects focal/diffused
involvement of the CNS and is the result of
a disturbance of the cerebral circulation.
脑卒中是指急性起病 、迅速出现局限性
或弥漫性脑功能缺失征象的脑血管性事件。
Epidemiology:
CVD is the third most common cause of
death after heart disease and cancer.
Incidence: 100~300/100,000
morbidity: 100~740/100,000
mortality: 50~100/100,000
About 50%~70% of survivors shows
disability in different degree.
Classification of CVD
According to the lasting time of neurologic deficit:
TIA (<24h)
stroke (>24h).
According to the severity of neurologic deficit:
minor stroke
major stroke
silent stroke
According to the pathological features:
ischemic stroke
hemorrhagic stroke (see table 8-1)
脑部的血液供应-Blood supply in brain
颈内动脉系统 - internal carotid artery (ICA) S.
眼动脉-ophthalmic artery
后交通动脉-post communicating artery
脉络膜前动脉-anterior choroidal artery
大脑前动脉-anterior cerebral artery (ACA)
大脑中动脉-middle cerebral artery (MCA)
供应眼部及大脑半球前3/5部分即额叶、颞叶、顶叶及基
地节的血液
见图the circle of Willis环
见图脑基底部动脉
椎-基底动脉系统-vertebral-basilar artery S.
椎动脉(VA): Which is divided into
anterior
spinal artery (脊髓前动脉)
posterior
spinal artery (脊髓后动脉)
medullary
artery (延髓动脉)
posterior inferior cerebellar artery (小脑
后下动脉)
基底动脉(BA): Which has branches
of
anterior inferior cerebellar artery
(小脑前下动脉)
branches of pons(脑桥支)
internal auditory artery(内听动脉)
superior cerebellar artery (小脑上
动脉)
大脑后动脉 (posterior cerebral artery,
PCA) , which is the terminal division of
BA
椎基底动脉系统供应脑干,小脑及大脑 半球
后2/5部分即枕叶及颞叶的基底面,枕叶的
内侧及丘脑等。
Etiology of CVD
Vascular disorder
Atherosclerosis
Inflammatory disorders (TB,syphilitic
arteritis, SLE, etc.)
Congenital vascular malformation
(aneurysm, AVM )
Lesions of any cause
Etiology of CVD
Heart diseases and blood kinetics
changes
Hypertention or hypotension
Atrial fibrillation, Rheumatic heart
disease, arrhythmias etc.
Changes in blood constituent and
hemodynamics
Increase in blood viscosity
Abnormality in blood coagulation
mechanism
Others
Such as emboli of air , fat, cancer cells.
Blood vessel spasm, trauma, etc.
Risk factors
Several factors are known to increase the
liability to stroke. The most important of
these are:
Hypertention
Heart diseases
Diabetes
TIA or stroke history
Risk factors
Smoking and alcohol
Hyperlipidmia
Others: food, symptomless ICA bruit,
overweight, drug abuse, contraceptive,
age, sex, family history, race, etc.
Section 2
Transient Ischemic Attack, TIA
(短暂性脑缺血发作)
Concept
Etiology and mechanism
Clinical findings
Investigative studies
Diagnosis and differentiation
Treatment and prevention
TIA-Concept
TIA is brief, repeated, reversible
episodes of focal ischemic neurologic
disturbance. The duration of which
should be less than 24h (usually lasting
about several min to 1h).
Repeated TIAs of uniform type are more
often a warning sign of ischemic stroke.
TIA-Etiology and mechanism
There is little doubt that they are due to
transient focal ischemia.
Their mechanism is not fully understood. But they might be thought of as
follows:
– Micro-emboli
– Vascular spasm
– Hemotologic disorders and blood
constituent changes
– Others
TIA-Clinical findings
Age of onset, 50~70, male > female
Basic features:
Transient episode (<24h)
Reversible
resolve completely
repeated and uniform type
Clinical features of carotid artery TIA
Common symptom/sign:
weakness of opposite limbs. (对侧单肢无力
或轻偏瘫)。
Characteristic symptom/sign:
ophthalmic artery crossing paralysis (眼动
脉交叉瘫)
Horner’s crossing paralysis (Horner 氏交
叉瘫)
Aphasia (dominant hemisphere is involved)
Clinical features of carotid artery TIA
Possible symptoms:
contralateral single limb- or hemisensory deficit
contralateral homonymous
hemianopia
TIA of Vertebra-basilar artery
Common symptom/sign:
vertigo, dysequilibrium, usually no tinnitus (
眩晕,平衡失调,多不伴有耳鸣 )
Characteristic symptom/sign:
drop attack (跌倒发作)
transient global amnesia( TGA,短暂性全
面性遗忘)
bioccular vision disorder (双眼视力障碍)
TIA of Vertebral-basilar artery
Possible symptom/sign:
swallowing disorder, dysarthria/dysphagia
(吞咽障碍、构音不清)
incoordination (共济失调)
disturbence of consciousness with /without
small pupils (意识障碍伴或不伴瞳孔缩小)
TIA of Vertebral-basilar artery
Possible symptom/sign:
unilateral/bilateral facial/perioral numbness
or crossing sensory deficit (一侧或双侧面部
/口周麻木或交叉性感觉障碍)
extraocular palsy or diplopia (眼外肌麻痹
或复视)
crossed paralysis (交叉性瘫痪)
TIA Symptoms Related
to Cerebral Circulation
Circulation Involved
Anterior Either Posterior
Symptom
Dysphasia
Unilateral weakness
Usually
Unilateral sensory disturbance
Usually
Dysarthria
Plus other
Homonymous hemianopia
Unsteadiness/ataxia
Plus other
Dysphagia
Plus other
Diplopia
Plus other
Vertigo
Plus other
Bilateral simultaneous visual loss
Bilateral simultaneous weakness
Bilateral simultaneous sensory disturbance
Crossed sensory/motor loss
TIA-Diagnosis and differentiation
Diagnosis:
mainly depend upon history. But the
causes of TIA are very important.
differentiation:
partial seizure (局限性癫痫)
Méniere Disease (美尼耳氏病)
Heart diseases: Adams-stokes
syndrome, severe arrhythmia, etc.
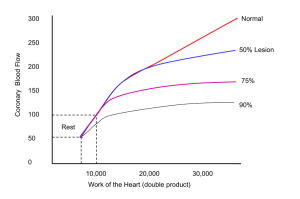
Management
Diagnosis of Carotid Stenosis
Percent of patients
Carotid bruit related to stenosis
40%
No Bruit
30%
Bruit
20%
10%
0%
Normal
1 - 24
25 - 49
50 - 74
75 - 99
Occluded
Percent stenosis of symptomatic ICA
Investigative study
Blood Test: Blood count, ESR, blood
glucose, etc.
EEG, CT or MIR
ECG, Cardiac Ultralsound
Carotid Duplex Ultrasound
Others
TIA-treatment and prevention
Treatment in terms of etiology
Drugs for prevention
Antiplatelet agents: Aspirin (ASA),
Ticlopidine, Dipyridamole, Clopidogre
Anticoagulation therapy: 肝素
(heparin), 低分子肝素 (lower
molecule heparin),华法林 (warfarin)
TIA-treatment and prevention
Drugs for prevention
Others: Chinese traditional medicines,
vasodilatation agents, blood volume
enlargement doses and surgical
treatment(carotid endoarterectomy,
intralumenal stents)
Cerebral protective agents
Prognosis
1/3 will develop into cerebral
Infarction afterward
1/3 recurrence
1/3 resolved
Summary
the most important parts need to be
emphasized are:
clinical findings,
diagnosis
menagement
Case Example
A 55 year old male presents to the
emergency department with acute onset
of
Left arm weakness: Unable to lift left
arm off of lap
Symptoms improved on the way to
the hospital
Case Example
PMHx: Hypertension
Takes enalapril
Social Hx:
Smokes 1 ppd
Case Example
Physical Exam
Overweight
160/90, 80, 14, 37.5C
Right carotid bruit
Heart with regular rate and rhythm;
No murmur
Case
Example
Neuro exam
30 min after the onset of symptoms
Motor 4/5 strength in left upper
extremity.
Sensory subjective decrease in
pinprick in left upper extremity
compared to the right
Reflexes were 2+ except for the left
biceps, which was 3+, Gait steady
Case Example
Neuro exam
After an immediate CT scan, The
patient’s symptoms had completely
resolved and he had a normal
neurologic exam
Questions
What is the possible diagnosis of the
patient?
Which artery territory is involved?
What is the probable cause?
How should you menage the problem?
Section 3 脑梗塞-cerebral infarction
Concept: Cerebral infarction (CI) is
necrosis and malacia of brain tissues due
to ischemia and anoxia of the brain ,
which is in turn caused by deprived or
insufficient blood supply in brain.
是指脑部血液供应障碍,缺血、缺氧引
起脑组织坏死软化。
cerebral infarction
Common types: 脑血栓形成 (cerebral
thrombosis, CT)
脑栓塞 (cerebral embolism)
脑分水岭梗塞 (cerebral
watershed infarction, CWSI)
腔隙性梗塞 (lacunar infarct)
脑血栓形成-cerebralthrombosis(CT)
Etiology
Pathology
Clinical Features
Diagnosis and differentiation
treatment
Prognosis and prevention
Etiology
Stenosis of artery thrombosis
Atherosclerosis-the most common cause of
CT
Arteritis
Others: vascular malformation, blood
dyscrasia (高凝状态-hypercoagulable state、
真性红细胞增多症-polycythemia vera, 血小
板增多-thrombocytosis、DIC等)
Etiology
vascular spasm: SAH, migraine,
eclampsia (子痫), trauma, etc.
Indeterminate
Pathology
好发部位 :
大脑中动脉
颈动脉虹吸部及起始部
椎动脉及基底动脉中下段
4/5 located in region of ICA territory,
1/5 located in region of V-B A
Pathology
超早期(1~6h):脑组织改变不明显。
急性期(6~24h):脑组织苍白、轻度肿胀,
NC、胶质细胞及血管内皮细胞缺血
坏死期(24~48h):组织结构不清神经
细胞消失及胶质细胞坏变,炎细胞浸润,
脑组织明显肿胀
Pathology
软化期(3d~4w):脑组织开始液化变软
恢复期(3~4w):胶质细胞、胶质纤维
及毛细血管增生,形成胶质瘢痕和中风
囊
Pathophysiology
Blood flow blockage >30 seconds-metabolic change, >1 min -- cease of
neuron activity, >5min -- cerebral infarct.
Ischemic penumbra (缺血半暗带)
time window (6h)
Pathophysiology
Reperfusion damage: possible
mechanisms:
自由基 (free radical)形成及其瀑布式
反应
神经细胞内钙超载(calcium overload)
EAA毒性作用(toxic effect of
excitatory amino acid)
酸中毒(acidosis)
Types
大面积脑梗死(a large area CI)
分水岭脑梗死 (cerebral watershed
infarction, CWSI)
出血性脑梗死 (hemorrhagic infarct, HI)
多发性脑梗死 (multiple infarct, MI)
Clinical features
Clinical types
Complete stroke: reaches peak within
several hours (<6h)
progressive stroke: reaches peak within 48h
reversible ischemic neurological deficit
(RIND): Lasting >24h and recovering
within 3ws
Clinical features
General features:
Middle-aged or elderly people (caused
by Atherosclerosis), youth or middleaged people (caused by arteritis).
Stroke onset at quiet state and reaches
the peak within several hours to 1~2
days.
Clinical features
General features:
Usually, the patients are awake and
alert except for those with a large
area of CI or infarction in brainstem.
Clinical syndromes of CI
Occlusion syndrome of carotid artery
Carotid artery occlusion may be
asymptomatic. Symptomatic
occlusion results in syndromes follow:
Transient monocular blindness caused
by ipsilateral retinal artery ischemia.
Horner’s sign.
Clinical syndromes of CI
Occlusion syndrome of carotid artery
Carotid artery or ophthalmic artery bruit
and a weakened pulse in carotid artery.
Contralateral hemiplegia, hemisensory
deficit, and homonymous hemianopia.
Aphasia, if dominant hemisphere
involvement.
Clinical syndromes of CI
Oclusion syndrome of MCA
主干闭塞 (Occlusion in stem): is a
severe stroke syndrome which
combines the features of superior and
inferior division stroke.
三偏症状 (contralateral hemiparesis,
hemisensory deficit, and
homonymous hemianopia).
Clinical
syndromes
of
CI
Oclusion syndrome of MCA
失语症、体象障碍
(globle aphasia,
if dominant hemisphere is involved,
and body image disturbence )
意识障碍、颅内压增高、脑疝可导
致死亡
(disturbence of consciousness,
increased ICP, and herniation)
Clinical syndromes of CI
Oclusion syndrome of MCA
皮层支闭塞(occlusion in superior
division)
中枢性面舌瘫和偏瘫,偏瘫上肢重
于下肢 (contralateral hemiparesis
that affects the face, hand, and arm
but less severe in the leg).
Clinical syndromes of CI
Oclusion syndrome of MCA
皮层支闭塞(occlusion in superior division)
伴感觉障碍,主要是皮质感觉障碍
(contralateral hemisensory deficit,mainly
shows cortical sensory deficit)
失语、体象障碍 (aphasia and body
image disturbence)
Clinical syndromes of CI
Oclusion syndrome of MCA
深穿支闭塞(occlusion in inferior division)
对侧偏瘫(contralateral hemiparesis, upper
and lower limbs evenly affected)
对侧偏身感觉障碍及偏盲(contralateral
hemisensory deficit and homonymous
hemianopia)
可有失语(dominant hemisphere involved)
Clinical syndromes of CI
Occlusion syndrome of ACA
主干闭塞(occlusion in stem)
中枢性面舌瘫、偏瘫下肢重于上肢
(挑扁担样瘫) (Shoulde-pole-carrylike), 伴轻度感觉障碍
尿便障碍或尿急(旁中央小叶损),
(incontinence , paracentral lobule is
affected)
Clinical syndromes of CI
Occlusion syndrome of ACA
主干闭塞 (occlusion in stem)
精神症状 (psychiatric symptom) (颞
极与胼胝体受累,temporal pole
andcorpus callosum are affected),
常可见强握、吸吮反射 (额叶病变)
(grasp reflex, suck reflex are
common signs, lision in frontal lobe).
Clinical syndromes of CI
Occlusion syndrome of ACA
皮层支闭塞(occlusion in superior
division)
对侧偏瘫,下肢重于上肢
(sensorimotor deficit of the opposite
leg and foot and , to less degree, of
the shoulder and arm )
Clinical syndromes of CI
Occlusion syndrome of ACA
深穿支闭塞 (occlusion in inferior
division)
面、舌、肩瘫 (contralateral paresis
includes face, lingua, shoulder)
Clinical syndromes of CI
Occlusion syndrome of PCA
主干闭塞 (occlusion in stem ):
对侧偏盲、偏瘫及偏身感觉障碍(较
轻)
丘脑综合症 (thalamic syndrome)
主侧半球病变可有失读症(alexia).
Clinical syndromes of CI
Occlusion syndrome of PCA
皮层支闭塞( occlusion in superior
division )
对侧同向性偏盲(contralateral
homonymous hemianopia)、象限盲
(quadrant hemianopia)、皮质盲
(cortical blidness, bilateral
involvment)
Clinical syndromes of CI
Occlusion syndrome of PCA
皮层支闭塞( occlusion in superior
division )
主侧颞下动脉闭塞时可见视觉性失认症
(visual agnosia)和颜色失认
(achromatopsia)
主侧半球顶枕动脉闭塞可有对侧偏盲,
失语。
Clinical
syndromes
of
CI
PCA occlusion syndrome
深穿支闭塞 (occlusion in inferior division)
丘脑穿通动脉闭塞:红核综合征
(Claude syndrome)
丘脑综合征(thalamic syndrome): snesory
loss, spontaneous pain and dysesthesias,
choreoathetosis, intention tremor, spasm
of hand, mild hemiparesis.
Clinical syndromes of CI
PCA occlusion syndrome
深穿支闭塞 (occlusion in inferior
division)
中脑分支闭塞:Weber syndrome:
third nerve palsy ad contralateral
hemiplegia.
Clinical syndromes of CI
Syndrome of vertebral- basilar artery
occlusion
主干闭塞:广泛脑干梗死。Shows
symptoms of cranial nerves, pyramidal
tract, and cerebellum.
Clinical syndromes of CI
Syndrome of vertebral- basilar artery
occlusion
基底动脉尖综合征(Top of the basilar
Syndrome):
Abnormality in eye movement and pupils
disturbance of consciousness (loss of
consciousness)
homonymous hemianopia or cortical
blindness
severe memory disorder
Clincal syndromes of CI
Syndrome of vertebral- basilar artery
occlusion
脑干分支闭塞
Weber syndrome
Millard-Gubler syndrome
Foville syndrome
Clincal
syndromes
of
CI
Syndrome of vertebral- basilar artery
occlusion
小脑后下动脉闭塞-延髓背外侧综合症
(Wallenberg syndrome)
眼球震颤 (nystagmus)
交叉性感觉障碍 (crossed sensory
deficit)
球麻痹 (bulbar paralysis)
病灶侧Horner征 (ipslateral Hornor
sign)
病灶侧小脑性共济失调 (ipslateral
cerebellar ataxia)
Clincal syndromes of CI
Syndrome of vertebral- basilar artery
occlusion
闭锁综合征(Locked -in syndrome): 基底动
脉分支双侧闭塞
Cerebellar infarction
由小脑上动脉(superior cerebellar artery)、
小脑后下动脉(posterior inferior
cerebellar artery)、小脑前下动脉闭塞
(anterior inferior cerebellar artery)所致。
Laboratory findings
CT scan:normal at the day of onset of
the stroke, shows the low density of the
infarct after 24~48h. CT is preferred for
initial diagnosis since it can make the
critical distinction between ischemia and
hemorrhage (见图 )
Laboratory findings
MRI:may be superior to CT scan for
demonstrating early ischemic infarcts,
showing ischemic stroke in brainstem or
cerebellum and detecting thrombosis
occlusion of venous sinuses.
Laboratory findings
Cerebral angiography:MRA, DSA
Blood tests and ECG: Serum glucose,
cholesterol and lipid ,hemorheology.
TCD and CSF
Diagnosis and differentiation
Diagnosis
diagnosis can be made depending on
the clinical features (Patients
presenting with focal central nervous
system dysfunction of sudden onset,
Lasting more than 24h)
CT and MRI changes
Diagnosis and differentiation
Differential diagnosis:
Cerebral hemorrhage
cerebral embolism
Other structural brain lesions:
tumor,abscess, etc.
脑出血和脑梗塞的鉴别要点
脑出血
脑梗塞
1.发病年龄
60岁以下
多60岁以上
2.TIA史
多无
常有
3.起病状态
活动中
安静状态或睡眠中
4.起病速度
急(分、时)
较缓(时、日)
5.血压
明显增高
正常或增高
6.全脑症状
明显
多无
7.意识障碍
较重
较轻或无
8.颈强直
可有
无
9.头颅CT
高密度病灶
低密度病灶
10.脑脊液
血性,洗肉水样 无色透明
其中最重要的是2、3.两条。
Treatment
急性期治疗(Treatment in acute stage)
治疗原则: 超早期治疗--力争溶栓;
综合保护治疗;
个体化治疗;
整体化治疗;
对危险因素及时予以预防性干预措
施。
Treatment
超早期溶栓治疗
目的:溶解血栓;迅速恢复梗死区血
流灌注;减轻神经元损伤。(6h)
complications: Hemorrhage,
reperfusion damage and brain edema,
reocclusion.
Treatment
超早期溶栓治疗
Thrombolytic agents :Urokinase (UK),
Straptokinase (SK), recombinant tissue
plasminogen activator (rt-PA)
Treatment
超早期溶栓治疗
Indications:
Age < 75
no disturbance of consciousness
within 6h(or 12h for progressive stroke)
of onset
Bp < 200/120mmHg
no hemorrhage shown on CT scanning
exclusion of TIA
no other hemorrhagic diseases
Treatment
Antiplatelet agents
The regime is as described in the section of
TIA.
Anticoagulation agents: to prevent the
progression of thrombosis. The agents used are
the same as mentioned in the section of TIA.
Fibrinogen degradation therapy: 降纤酶
(Defibrase), 巴曲酶 (Batroxobin), 安洛克酶
(Ancrod)和引激酶。
Treatment
Neuroprotective agents:
抗自由基:V-E V-C 甘露醇 激素等
抑制脑代谢—急性期时应降低脑代谢,减
少脑细胞耗氧量使缺血区血流量增加
钙离子拮抗剂:西比灵 尼莫地平等
亚低温
胰岛素维持血糖正常低限水平
Treatment
Other forms of medical treatment: such
as therapies aimed at improving blood
flow: hemodilution, metabolic improving
agents-ATP, Co-A, 脑活素等。
Treatment
Surgical treatment
General treatment
ICU: monitoring ECG, Bp, R, P, etc.
Antiedema agents
Preventing infection
Physical therapy and rehabilitation
Preventive measures
腔隙性脑梗塞-Lacunar
Infarction
Concept:
Small penetrating arteries located deep in the brain
may become occluded as a result of changes in the
vessel wall induced by chronic hypertension and
atherosclerosis.
是指发生在大脑半球深部白质及脑干的缺血性微
梗死因脑组织缺血、坏死、液化并由吞噬细胞移
走而形成腔隙,占脑梗死的。多见于基底节区、
放射冠、丘脑、脑干等部位。
腔隙性脑梗塞-Lacunar Infarction
Common types:
纯运动性卒中(Pure motor hemiparesis,
PMH)
纯感觉性卒(Pure sensory stroke, PSS)
共济失调性轻偏瘫(Ataxic-hemiparesis,
AH)
构音障碍-手笨拙综合征 (Dysarthricclumsy hand syndrome, DCHS)
感觉运动性卒中(Sensorimotor stroke,
SMS)
腔隙状态(Lacunar state)
脑栓塞-Cerebral embolism
Concept
Etiology and mechanism
Clinical findings
Investigative studies
Diagnosis and differentiation
Treatment and prognosis
脑栓塞-Cerebral
embolism
Concept:
embolism produces stroke when
cerebral arteries occluded by the distal
passage of thrombus from the
heart,aortic arch, or large cerebral
arteries.
脑栓塞指各种栓子随血流进入颅内动
脉系统使血管腔急性闭塞引起相应供
血区脑组织缺血坏死及脑功能障碍。
脑栓塞-Cerebral
embolism
Etiology
心源性 (Cardiogenic)
非心源性 (non-cardiogenic)
来源不明 (source unknown)
Pathology
多见于颈内动脉系统,尤其是左侧大
脑中动脉,病理上与脑血栓形成基本
相同。但栓子常为多发切易破碎。
Clinical findings
发病急骤,症状在数秒或数分钟内达高峰,
是血管病中最快的
多属完全性中风,栓塞部位继发血栓时病情
可逐渐进展
可有头痛、局灶性癫痫和不同程度的意识障
碍
神经系统定位体征
原发病的症状和体征
易发生梗塞后出血
Laboratory Findings
CT, MRI: indicate ischemic Infarct or
hemorrhagic infarct
MRA shows the stenosis of large cerebral
arteries.
CSF examination: Can be normal, or with
increased ICP. Red blood cells can be seen
grossly or under microscope.
Laboratory Findings
ECG: 心律失常 (arrhythmia)、心肌梗塞
(myocardical infarction, MI) 等
Ultrasonography
Echocardiography
Cerebral angiography
Diagnosis and differentiation
诊断:急骤起病,有定位体征,有栓子
来源
鉴别诊断:
与脑出血、脑血栓鉴别
有局限性癫痫者应与其它引起癫痫的
疾病鉴别.
Treatment and prognosis
Treatment:
Antiedema and increased ICP
Recurrence prevention treatment:
emboli originated disease treatment.
Vasodilation agents
Treatment and prevention
Treatment:
others
prognosis:
mortality
- 5%~15%. Die from severe
cerebral edema, herniation, respiratory
system infection, and heart failure.
Majority of Survivors will have severe
disability
本课重点
TIA的临床特点,颈内动脉和椎-基底动
脉TIA的最常见的表现及特有症状
脑血栓形成的常见病因,好发部位,临
床特点及治疗重点
腔隙性脑梗死的常见临床类型几表现
脑栓塞的常见病因、临床特点及鉴别诊
断