Complex-Regional-Pain
advertisement
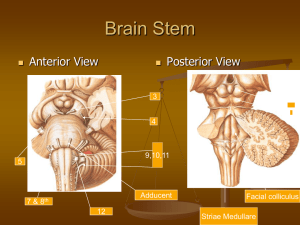
Complex Regional Pain Syndrome Dr. Dawood Nasir Definition • CRPS: Complex regional Pain Syndrome, a neuropathic pain syndrome associated with sympathetic nervous system dysfunction • CRPS1: Previously known as Reflex sympathetic dystrophy, is a syndrome occurring after minor trauma • CRPS 11: Causalgia, usually occurs after major nerve injury Complex Regional Pain Syndrome Pathophysiology • Peripheral & Central Mechanism • Proposed mech include - Sensitization of small diameter polymodal C & A delta afferent fibers - Sensitization of central wide dynamic range neurons - Altered activity of low threshold A beta fibers Question • Complex regional pain syndrome type 11 (Causalgia) is differentiated from complex regional pain synd type 1 by knowledge of A. Etiology B. Chronicity C. Affected body region D. Type of symptoms E. Rapidity of onset Answer (A) • Complex regional pain syndrome type 1 is a clinical syndrome of continuous burning pain usually occurring after an injury or surgery. Pts present with variable sensory, motor, autonomic, & trophic changes. Complex regional pain syndrome type 11 exhibits the same features as complex regional pain syndrome type 1, but the etiology is damage to a major nerve. Epidemiology • Incidence - Unknown • Prevalence - Unknown - Women predominate (60-80 percent) - Mean age: 36-42 years • Genetics - Genetic correlation debated Diagnostic criteria At least 4 of the following must be present to diagnose CRPS Examination findings: 1. Temperature / Color change. 2. Edema 3. Trophic skin, hair, nail growth abnormalities. 4. Impaired motor function. 5. Hyperpathia / Allodynia 6. Sudomotor changes Diagnostic criteria-cont• Diagnostic test results - Three phase bone scan that is abnormal in pattern characteristic. - This test is not needed if 4 or more of examination findings are present. Stages of Complex regional type 1 • CRPS 1 is divided into 3 stages 1. Acute 2. Dystrophic 3. Atrophic Acute phase • • • • Pain: Localized, Severe, Burning Extremity : Warm, swollen, nail growth Skin: Dry & red, growth of hairs X-ray: Normal Mech.: Could be due to increase blood supply Dystrophic Phase • Pain: Diffuse, throbbing • Extremity: Cold, Cyanotic, edematous, muscle wasting. • Skin: Sweaty, thinning or loss of hairs • X-ray: Reveals osteoporosis Mech.: Could be due to vasoconstriction Atrophic Phase • • • • Pain: Less severe, may involve other extremities Extremity: Severe muscle atrophy, contractures Skin: Glossy & atrophic X-ray: Reveals severe osteoporosis, & ankylosis of joints. Mech.: Could be due to disuse atrophy Physical Exam • Allodynia: Perception of non noxious stimulus as painful • Hyperesthesia: Increased response to mild stimulus • Skin discoloration/mottling • Dry glossy extremity • Sweating • Edema • Abnormal temperature • Weakness, tremor, Hyperkeratosis, Brittle nail Question • Allodynia is defined as A. Spontaneous pain in an area or region that is anesthetic B. Pain initiated or caused by a primary lesion or dysfunction in the nervous system. C. An unpleasant abnormal sensation, whether spontaneous or provoked D. An increased response to a stimulus that is normally painful E. Pain caused by a stimulus that does not normally provoke pain. Answer (E). • The IASP has defined several pain terms. Anesthesia dolorosa: refers to spontaneous pain in an area or region that is anesthetic. Neuropathic pain: is caused by dysfuction in NS. Dysthesia :is unpleasant abnormal sensation. Hyperalgesia :is increased response to painful stimulus. Allodynia: is pain caused by a stimulus that does not normally provoke pain. Tests • Imaging - Osteoporosis or fine demineralization on xray - Increased periarticular uptake in delayed bone scintigraphy Pathological findings • Reduced thermoregulatory reflexes • Changes in sudomotor neuron activity • Neurogenic inflammation Question • Which of the following choices is not consistent with a limb affected by complex regional pain syndrome? A. Osteoporosis. B. Allodynia. C. Dermatomal distribution of pain D. Atrophy of the involved extremity. E. Hyperesthesia. Answer © • CRPS are associated with trauma. The main feature is burning & continuous pain ie exacerbated by normal movement, cutaneous stimulation, or stress usually weeks after the injury. The pain is not anatomically distributed. Other associated features include cool, red, clammy skin & hair loss in the involved extremity. Chronic cases may be associated with atrophy & osteoporosis. Differential Diagnosis • • • • • • • • Infection Hypertrophic scar Bone fragments Neuroma Radiculopathy Joint contracture CNS tumor Syringomylia Medications • First line - Anticonvulsants 1. Gabapentin up to 900 mgs PO q8 hrs. 2. Pregabalin up to 300 mg PO q 12 hrs - Tricyclic antidepressants: 1. Amitriptiline up to 150 mgs PO qhs 2. Nortriptylene: upto 150 mgs PO qhs 3. Desipramine: upto 150 mgs PO qhs - NSAIDs: If no complications Second Line • • • • • • Other anticonvulsants Oxcarbazepine upto 600 mg PO q12 hrs Lamotrigine upto 150 mgs PO qhs Short & long acting opioids (Controversial) Alpha adrenergic blocking agents Corticosteroids(Short term only) Biphosphonates Topical therapies Interventional • Regional anesthetic approaches • Sympathetic blockade (local with or without steroids) • Peripheral nerve blockade • IV regional analgesia (reserpine, guanethidine, bretylium) • Chemical sympathetic neurolysis • Radiofrequency sympathetic rhizotomy • Epidural clonidine • Spinal cord stimulation Rehabilitation • • • • • • • • Avoid immobilization Desensitization Mobilization Edema control Isometric/Isotonic strengthing Stress loading/range of motion Aerobic conditioning TENS Mental Test/Behavioral • • • Psychometric testing Counseling Behavioral modification Relaxation therapy Group therapy Self-hypnosis Psychotherapy Medical management of depression Technique for Stellate ganglion Block • Pt. supine, head midline, mouth slightly open • 2 finger breadth or 2 cm. above clavicular head, trachea, sternocleidomastoid ms, & carotid sheath palpated at level of cricoid cartilage • 2 fingers press down at lat. Edge of transverse process of C6, pushing the contents of carotid sheath laterally • A 1.5-3 in. 23 or 25 gauge B bevel needle is inserted lat to trachea after skin inf. With local anesth. • Transverse of C6 encountered between 2 fingers withdraw needle 2 mm & inj 8-10 ml local Stallate Ganglion Stellate Ganglion Block Question • Stellate ganglion lies in closest proximity to A. Common carotid artery. B. Internal carotid artery. C. Vertebral artery. D. Axillary artery. E. Aorta. Answer © • The stellate ganglion usually lies in front of the neck of the 1st rib. The vertebral artery lies anterior to the ganglion as it has just originated from the subclavian artery. After passing over the ganglion, it enters the vertebral foramen & lies posterior to the anterior tubercle of C6. Signs of successful block • • • • Horner’s synd. Ipsilateral nasal congestion Flushing of conjunctiva & skin Temperature increase in the ipsilateral arm & hand Side effects & complications • • • • • • • • • Lump sensation in throat Hoarseness & dysphagia due to recurrent n block Hematoma, osteitis Brachial Plexus block Phrenic nerve block Epidural & subarachnoid block Pneumothorax Vertebral art. Inj. Causing loss of consciousness Cardioaccelarator nerve block with hypotension Follow up Prognosis • Some resolve with minimal management • Most respond to initial conservative measure • Early aggressive treatment in those with rapid temporal changes has best results if initiated within 12 weeks of onset • Prognosis poor if pain becomes chronic with marked disability, thus emphasizing multidisciplinary approach.