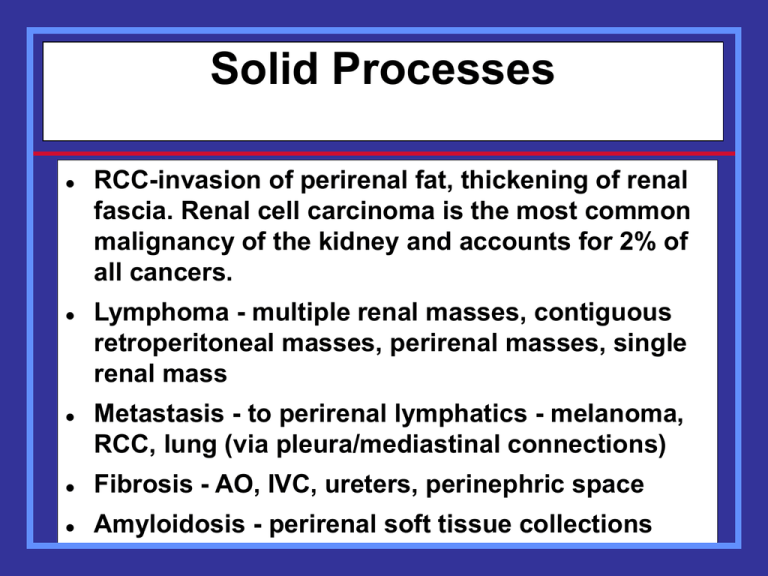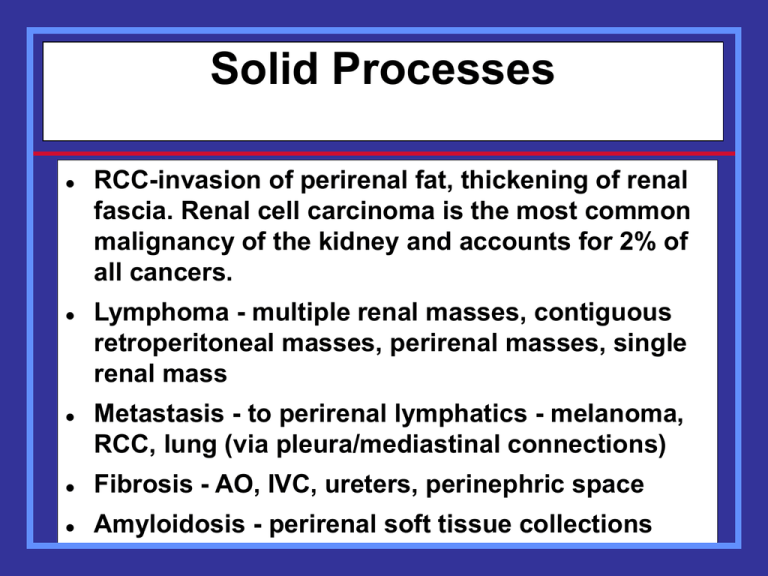
Solid Processes
RCC-invasion of perirenal fat, thickening of renal
fascia. Renal cell carcinoma is the most common
malignancy of the kidney and accounts for 2% of
all cancers.
Lymphoma - multiple renal masses, contiguous
retroperitoneal masses, perirenal masses, single
renal mass
Metastasis - to perirenal lymphatics - melanoma,
RCC, lung (via pleura/mediastinal connections)
Fibrosis - AO, IVC, ureters, perinephric space
Amyloidosis - perirenal soft tissue collections
Renal cell carcinoma (RCC)
• is the most common primary renal malignant
neoplasm in the adult. It accounts for
approximately 85% of renal tumors and 2% of
all adult malignancies.
• RCC is more common in men than in women
(ratio, 2:1), and it most often occurs in
patients aged 50-70 years.
• One fourth to one third of patients have
metastatic disease at the time of
presentation.
• In only approximately 2% of sporadic cases
are bilateral tumors seen at presentation.
RCC risk factors include
• increased age, male sex, smoking,
cadmium, benzene, trichloroethylene and
asbestos exposure, excessive weight,
chronic dialysis use, and several genetic
syndromes (familial RCC, hereditary
papillary RCC, von Hippel-Lindau
syndrome, and tuberous sclerosis)
Renal Cell Carcinoma with
Spread to Gerota’s Fascia
MRI of the Kidneys
When contraindication to IV contrast
Renal mass characterization
Staging renal cell carcinoma
Vascular involvement
Renal cell carcinoma
MRI better than CT in demonstrating
vascular invasion
– Renal vein
– IVC
Tumor
Tumor
Coronal
Axial
Renal Cell Carcinoma
with tumor invading
right renal vein and IVC
Tumor
Axial
Retroperitoneal Lymphoma
Lymphadenopathy - can directly invade
kidney or encase ureter
Perirenal involvement - transcapsular,
direct spread from lymph nodes,
isolated disease (least common)
Lymphoma - Direct invasion of kidneys
Perirenal Lymphoma
Bilateral Perirenal Lymphoma
Lymphoma involving the small bowel mesentery,
anterior pararenal space, perinephric space and
kidneys
Metastatic
Lung Cancer
Perinephric
Metastasis
Adrenal
Metastasis
Renal Infarction
Causes
–
–
–
–
Embolism (cardiac)
Aortic dissection
Trauma
Venous thrombosis (dehydration, tumor)
Renal Infarction
CT Findings (with IV contrast)
Focal
– Region of no enhancement
Diffuse
– Hypodense kidney
– Renal enlargement
May see rim of enhancement
– Patent collateral capsular vessels
Two contrast-enhanced axial CT
images demonstrate a wedgeshaped non-enhancing lesion in the
right kidney with no perinephric
inflammatory stranding
History atrial fibrillation, presents
with right flank pain
Left atrial
thrombus
Renal
infarct
Right Flank Pain
Renal
tumor
IVC
Renal infarct
Presents with
left flank pain
Pyonephrosis —
gas in infected
collecting system
Patient Presents with
Right Flank Pain
Kidney normal
Cholecystitis
Gallstone in distended GB
2 Different Patients with
Right Flank Pain
Dermoids
Ovarian cyst
CRF: Prominent bridging septae
and small amount of perinephric fluid
Kidney “sweat sign”
Fluid in perirenal space corresponding to
thickened septae and fluid on CT scan
Echogenic kidneys in patient with CRF
Acute Pancreatitis
Inflammatory process spares perinephric
spaces
Acute hemorrhage in anterior pararenal space
involves perinephric space via septae
Lymphatic Spread of Disease
from Perinephric Space
•Small perirenal lymph nodes
Nodes in renal hilum
Periaortic/pericaval nodes
Inflammatory Processes
and Fluid Collections
Infections
Urinomas
Hematomas
Pseudocysts
Infections
Most originate from kidney
May spread through all spaces and via
bare area to peritoneum and thorax
Xanthogranulomatous pyelonephritis
Subcapsular
Abscess
Chronic Perinephric Abscess
Abscess is loculated in perinephric space secondary to perinephric septae.
See also calculus and mild hydronephrosis
Pyelonephritis in Ectopic Kidneys
Adrenal Level
Renal Level
Note straight adrenal glands with liver, spleen and colon falling into expected renal fossae. At level of pancake kidney,
renal fascia is visualized and slightly thickened.
Perinephric gas extending to extraperitoneal space and to anterior abdominal wall muscles.
Patient with fever
after left
hemicolectomy
Xanthogranulomatous
Pyelonephritis
Obstructed upper pole
Extension to post pararenal
space and post abd wall
Perinephric Collection
Hematomas
Traumatic- MVA, iatrogenic
Spontaneous- tumor, vascular (AAA,
AVM, arteritis), hematologic disorders,
endstage kidney
Spread of hepatic or splenic hematomas
to perinephric space without renal
injury
Leaking aortic aneurysm
Subcapsular into anterior pararenal space extending along iliac vessels into pelvis.
Also via perinephric septae to upper aspect post pararenal space
Spontaneous
Hemorrhage in
End-stage Kidney
Subcapsular to perinephric to anterior
pararenal hematoma secondary to
renal artery stent placement
ATN with vicarious
gallbladder excretion
Renal Cell Carcinoma
with spontaneous
hemorrhage
Traumatic
Avulsion Renal
Artery
RRA
with
perinephric
hematoma
Retroperitoneal Fibrosis
Most commonly idiopathic
Other causes: aortic hemorrhage, aortitis,
methysergide toxicity, prior surgery or
XRT, collagen vascular disease (Riedel’s
thyroiditis, sclerosing mediastinitis)
Clinical: 40-60 yrs, males>females
Hydronephrosis, ureteral narrowing, slight
medial ureteral displacement
Retroperitoneal Fibrosis
Retroperitoneal Fibrosis extending
into perinephric and postpararenal spaces
MRI of the Adrenal Glands
Metastases versus non-functioning
adenoma
Suspected pheochromocytoma
Helpful to localize origin of mass
discovered on CT/US
– Upper pole kidney vs adrenal gland
Is this mass arising
from the liver,
kidney or adrenal
gland?
Coronal imaging shows mass not renal in origin
Adrenal tumor invading liver
Adrenal Masses
Adenomas are very common
– 2-8% of population
Metastases are common in adrenal
glands
Fortunately, MR can accurately
distinguish between adenomas and
metastases
Adrenal Adenomas
Key to diagnosis is demonstrating
fat/lipid in mass
Chemical shift imaging
Fat suppression imaging
MRI of adrenal adenomas
High lipid content
Chemical shift imaging helpful
– In-phase: bright
– Out-of-phase: dark
Look for “india ink” rim at fat/water interface
In-phase image
Out-of-phase image
Abdominal Aortic Aneurysm
Without rupture may present as
pulsatile abdominal mass without pain
With rupture, typically present with
back pain or mid abdominal pain
CT Diagnosis of AAA Rupture
Retroperitoneal hematoma
Contrast extravasation
High density crescent
Calcified rim of aorta is discontinuous
Discontinuous aortic wall
Contrast extravasation
A
retroperitoneal hematoma
Abdominal Aortic Dissection
Defined as hematoma in wall, typically
with intimal tear
CT is screening modality of choice
Acute aortic dissection is most common aortic
emergency Helical CT with sensitivity and
specificity near 100%
Considered acute if sx < 2 weeks, chronic if
longer
75% deaths occur within 2 weeks of initial sx
Hypertension is major cause adding mechanical
stress to aortic wall with longitudinal shearing forces
and decreased vasa vasorum flow increases stiffness
of media causing more stress and contributing to
development of dissection
Abdominal Aortic Dissection
CT Diagnosis
Contrast in 2 channels
– If one lumen thrombosed difficult to
differentiate from mural thrombus
Intervening intimal flap
1
2
1
2
Pt presented with
flank pain, had
unenhanced CT
Calcified intimal flap displaced
medially from wall of aorta
Contrast demonstrates 2 lumens
Penetrating Atherosclerotic Ulcer
Ulceration of atheromatous plaque that
erodes inner, elastic layer of aortic wall
and when it reaches medial layer, media
is exposed to arterial flow, causing
hemorrhage in wall.
Localized dissection can occur, break
into adventitia, resulting in PSA or
rupture
CT Findings
Unenhanced: extensive atherosclerosis, focal
and variable IMH, displaced intimal
calcification
Enhanced: Collection of contrast visualized
outside lumen, similar to peptic ulcer. May be
multiple or single with thickening of aortic
wall.
Atheromatous ulcers confined to intima may
be seen in asymptomatic patients, but should
be followed for progression to aortic
aneurysm. When rupture occurs, impossible
to differentiate from ruptured aneurysm.
Unenhanced CT with IMH, enhanced CT at
same level shows ulcer filled with contrast
Castaner
True lumen of celiac trunk and left renal artery narrowed by
thrombosed false lumen. Left renal infarction