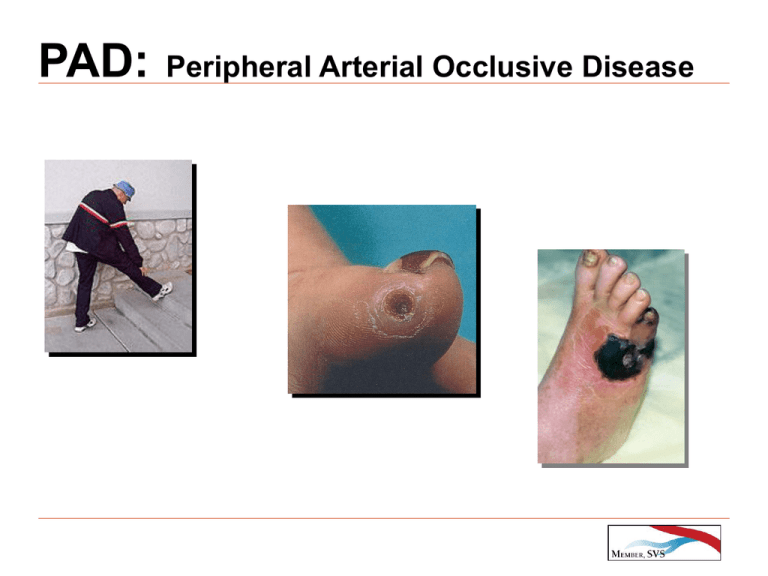
PAD: Peripheral Arterial Occlusive Disease
advertisement
PAD: Peripheral Arterial Occlusive Disease PAD in the United States Common Manifestation of Atherosclerosis Prevalence: 12% - 14% of the General Population - Up to 20% of Population > 75 Years Old Increased risk from Cerebrovascular & Coronary Disease PAD: PREVALENCE vs AGE Criqui MH, et al, Circulation, 1985 EPIDEMIOLOGY OF ATHEROSCLEROSIS STROKE MI PAD Incidence Prevalence Mortality (millions) (millions) (%) .7 4 1.1 7 - 22 31 33 4 PAD: LONG-TERM MORTALITY Criqui MH, et al, Vasc Med, 2001 PATIENTS WITH INTERMITTENT CLAUDICATION Cause of Death Coronary Artery Disease 63% Cerebrovascular Disease 9% All Cardiovascular Diseases 80% Smith DG, et al, Circulation, 1990 INTERMITTENT CLAUDICATION Exercise-Induced Limb Pain / Weakness Symptoms Relieved with Rest Marker for Underlying Systemic Atherosclerosis Prognosis Worse with Multiple Risk Factors CLAUDICANTS: LONG-TERM OUTCOME Ouriel K, Lancet, 2001 PAD: NONINVASIVE LAB EVALUATION (PVR) PAD: ABI PREDICTS SURVIVAL PAD: Rx of INTERMITTENT CLAUDICATION Symptomatic Rx Systemic Rx Exercise Risk Factor Control Smoking Cessation Pharmacologic Endovascular / Open Surgery - Smoking Hyperlipidemia Hypertension Diabetes Pharmacologic - Antiplatelet - Statins - Beta Blockers AORTO-ILIAC OCCLUSIVE DISEASE PATIENTS Younger than Femoral-Popliteal Disease More Often Hyperlipidemic Less Often Diabetic Claudicants AORTO-ILIAC OCCLUSIVE DISEASE DIAGNOSIS HISTORY: - Proximal Claudication +/- PHYSICAL EXAM: - Femoral Pulses +/- NONINVASIVE LABORATORY *** - Thigh Pressure +/- Waveform *** AORTO-ILIAC OCCLUSIVE DISEASE SURGICAL OPTIONS BILATERAL DISEASE UNILATERAL DISEASE Aorto-Iliac Endarterectomy Ilio-Femoral Bypass Aorto-Bifemoral Bypass Femoral-Femoral Bypass Axillo-Bifemoral Bypass Axillo-Femoral Bypass Thoracic Aorta-Fem-Fem Bypass (PTA & Femoral-Femoral Bypass) AORTO-ILIAC OCCLUSIVE DISEASE SURGICAL OPTIONS ANATOMIC EXTRA-ANATOMIC Aorto-Iliac Endarterectomy Femoral-Femoral Bypass Aorto-Femoral Bypass Axillo-Bifemoral Bypass Ilio-Femoral Bypass AORTO-ILIAC ENDARTERECTOMY INDICATIONS: Focal Disease CONTRAINDICATIONS: Aneurysm Disease Extending to Renal Arteries Disease Extending to External Iliac Arteries Largely Replaced Today with Angioplasty AORTO-ILIAC ENDARTERECTOMY AORTO-FEMORAL BYPASS AORTO-FEMORAL BYPASS OPERATIVE MORTALITY 1960s 12% 1970s 6% 1980s < 5% 1990s 2% AORTO-FEMORAL BYPASS PATENCY Source (Yr) # Pts. Brewster (1978) Martinez (1980) Crawford (1981) Szilagyi (1986) Rutherford (1986) Vantinnen (1991) Nevelsteen (1991) 464 376 949 1749 157 177 912 PATENCY (%) 5-Yr 10-Yr 15-Yr 88 88 87 85 86 91 93 75 78 84 83 74 77 AORTO-FEMORAL BYPASS COMPLICATIONS Graft Limb Occlusion Graft Infection Graft-Enteric Fistula Anastomotic Aneurysms Ureteral Obstruction Male Sexual Dysfunction AORTO-FEMORAL GRAFT LIMB OCCLUSION ETIOLOGY EARLY Distal Intimal Flap Kinking / Twisting Incomplete Clot Evacuation Unsuspected Hypercoagulability SEVERE OUTFLOW DISEASE *** AORTO-FEMORAL GRAFT LIMB OCCLUSION: LATE LATE (< 2 Yr) Anastomotic Hyperplasia ANGIOGRAPHY: Anastomoses Contralateral Limb Run-Off: LYSIS LATE (> 2 Yr) Progressive Atherosclerosis*** Anastomotic Pseudoaneurysm AXILLO-FEMORAL BYPASS CANDIDATES: Severe Comorbidity & Limb-threatened Infection AXILLO-FEMORAL BYPASS PATENCY 1- YEAR …………………… 22% - 100% 3-YEAR …………………… 36% - 97% 5-YEAR …………………… 34% - 87% AXILLO-FEMORAL BYPASS (Oregon HSU) PATENCY % P A T E N C Y 100 90 80 70 60 50 40 30 20 10 0 Ax-Fem Aorto-Fem 1 2 3 YEARS 4 5 AXILLO-BIFEMORAL BYPASS UNILATERAL ILIAC ARTERY OCCLUSION FEMORAL-FEMORAL BYPASS ILIO-FEMORAL BYPASS - Extra-Anatomic - Anatomic - Superficial - Retroperitoneal Dissection vs - Less Morbidity - More Morbid - Lower Patency - Better Patency FEMORAL-FEMORAL BYPASS PATENCY (13 Series / 919 Patients) 1- YEAR …………………… 74% - 98% (mean, 88%) 3-YEAR …………………… 62% - 85% (mean, 77%) 5-YEAR …………………… 45% - 80% (mean, 67%) BILATERAL ILIAC ARTERY DISEASE - PTA & FEMORAL-FEMORAL BYPASS Johns Hopkins 100 % 90 80 70 P 60 A 50 T 40 E 30 N 20 C 10 Y 0 J Vasc Surg. 1996 66% 59% PTA & FEM-FEM FEM-FEM 1 2 3 4 YEARS 5 6 7 ILIO-FEMORAL BYPASS PATENCY INSTITUTION # PTS PATENCY F/U (YRS) Brigham 56 75% 4 U. Toronto 50 92% 3 U. Wisconsin 20 100% 2 Johns Hospkins 22 92% 6 THORACIC AORTA-FEMORAL BYPASS PATENCY (U North Carolina) J Vasc Surg, 1999 ILIAC ANGIOPLASTY: UCLA (1993 – 2004) J Vasc Surg, 2005 ILIAC ANGIOPLASTY: UCLA (1993 – 2004) J Vasc Surg, 2005 AORTOILIAC RECONSTRUCTION SUMMARY Increasing Endovascular Interventions Decreasing Open Surgical Procedures Multiple Surgical Options - Anatomy - Comorbidity Patient Selection Key INFRAINGUINAL ARTERIAL OCCLUSIVE DISEASE EPIDEMIOLOGY Lower Extremity Atherosclerosis: 10% > 70 yo Limb-Threatening Ischemia: 50,000 Individuals / Year 80,000 Infrainguinal Bypass Grafts / Year Elderly: Fastest Growing Population Segment FEMORAL-POPLITEAL-TIBIAL BYPASS - Indications - **** ** LIMB THREATENING ISCHEMIA - Rest Pain - Nonhealing Ulcers - Gangrene CLAUDICATION - 50%-67% Improve Medically - 2% -7% Limb Loss / Year FEMORAL-POPLITEAL-TIBIAL BYPASS - Operative Mortality SOURCE Cleveland Clinic Med Coll WI Albany Med Coll UCLA Brigham Oregon U Johns Hopkins VA Multicenter Brigham (Yr) (1987) (1987) (1988) (1988) (1988) (1990) (1995) (2000) (2000) No. Pts. 932 192 1038 120 266 564 100 752 172 % Mortality 4.4% 3.0% 6.7% 1.2% 1.4% 1.3% 2.0% 0.8% 2.4% FEMORAL-POPLITEAL-TIBIAL BYPASS - Wound Morbidity - INCIDENCE: 5% - 30% RISK FACTORS: - Vein Harvesting Ischemic Limb Diabetes Re-Do Procedures Infected Lesions FEMORAL-POPLITEAL-TIBIAL BYPASS - Wound Morbidity – Oregon Health Science U PATIENTS: 112 Diabetes ……………. 53% Renal Failure ……… 22% Limb Salvage ……… 96% PROCEDURES: Fem-Pop …………… Fem-Tib …………… Pop-Tib …………… Vein ………………… 52% 38% 10% 91% WOUND COMPLICATIONS: 24% TIME TO HEALING: 0.4 – 10.1 (mean, 1.9) Months J Vasc Surg, 1998 FEMORAL-POPLITEAL-TIBIAL BYPASS REDUCED WOUND MORBIDITY Duplex Vein Mapping Endoscopic Vein Harvest FEMORAL-POPLITEAL-TIBIAL BYPASS Kent & Queen Anne Hosp METHOD OF VEIN HARVEST ENDOSCOPIC (n=16) CONVENTIONAL (n=16) Wound Complications 0% 31% Mean LOS (days) 3.8 6.2 JACS, 1998 FEMORAL-POPLITEAL-TIBIAL BYPASS PATENCY: KEY VARIABLES *** GRAFT MATERIAL Vein vs Prosthetic ** SITE OF DISTAL ANASTOMOSIS Fem-Pop vs Fem-Tib * CLINICAL INDICATION Claudication vs Limb salvage FEMORAL-POPLITEAL-TIBIAL BYPASS CLINICAL INDICATION CLAUDICATION vs LIMB SALVAGE 100 % Claudication 80 P A T E N C Y 60 Limb Salvage 40 20 2,572 PATIENTS 15 YEARS 0 1 2 3 YEARS 4 5 FEMORAL-POPLITEAL-TIBIAL BYPASS DISTAL ANATOMOSIS FEM-POP vs FEM-TIB (SAPH. VEIN) 100 % Fem-Pop 80 P A T E N C Y 60 40 Fem-Tib 20 2,572 PATIENTS 15 YEARS 0 1 2 3 YEARS 4 5 FEMORAL-POPLITEAL-TIBIAL BYPASS GRAFT MATERIAL FEM-POP % % 100 P A T E N C Y FEM-TIB 100 p < .025 80 Vein 60 PTFE 40 20 2,572 PATIENTS 15 YEARS 0 P A T E N C Y P< .001 80 Vein 60 40 PTFE 20 2,572 PATIENTS 15 YEARS 0 1 2 3 YEARS 4 5 1 2 3 YEARS 4 FEMORAL-POPLITEAL BYPASS - LONG-TERM 1 0 PATENCY - Randomized Prospective Trial: FEM-POP % P A T E N C Y J Vasc Surg, 1986 68% 38% MONTHS FEMORAL-TIBAL BYPASS - LONG-TERM 1 0 PATENCY - Randomized Prospective Trial: FEM-TIB % P A T E N C Y J Vasc Surg, 1986 49% 12% MONTHS FEMORAL-POPLITEAL BYPASS LONG-TERM PATENCY: GRAFT MATERIAL SERIES: YEARS: PROCEDURES: % P A T E N C Y 69 15 11,600 100 72% 80 58% 45% 60 40 20 0 1 2 3 YEARS 5 VEIN HUV PTFE FEMORAL-TIBIAL BYPASS LONG-TERM PATENCY: GRAFT MATERIAL SERIES: YEARS: PROCEDURES: 69 15 11,600 % P A T E N C Y 100 80 56% 42% 60 33% 40 20 0 1 3 YEARS VEIN HUV PTFE FEMORAL-POP BYPASS (Above Knee) - LONG-TERM PATENCY RANDOMIZED TRIAL: VA MULTICENTER PATIENTS: 752 ASSISTED 10 PATENCY % P A T E N C Y J Vasc Surg, 2000 73% 53% MONTHS P < .01 MONTHS 39% FEMORAL-POPLITEAL-TIBIAL BYPASS - SECONDARY PROCEDURES Oregon HSU GRAFTS: YEARS: REVISIONS: % 1,498 1990 – 2000 330 / 259 GRAFTS (17%) 100 90 80 70 60 50 40 30 20 10 0 Assisted 10 Patency Limb Salvage 1 J Vasc Surg, 2002 3 5 7 YEARS 9 10 FAILING VEIN GRAFT - DIAGNOSIS - SYMPTOMS ANKLE-BRACHIAL INDEX: 15% DUPLEX SURVEILLANCE FAILING VEIN GRAFT DUPLEX SURVEILLANCE Sys Vel Ratio 2:1 ….. > 50% Sys Vel Ratio 3:1 ….. > 75% Sys Vel Ratio 4:1 ….. > 90% Sys Velocity < 45 cm/sec INFRAINGUINAL VEIN GRAFT STENOSES PTA vs SURG - Solitary Stenosis - Multiple Stenoses - Focal Stenosis - Longer Stenoses - First Presentation - Recurrent Stenoses - Reversed Graft - In-Situ Graft vs FEMORAL–POPLITEAL–TIBIAL BYPASS PATENCY META-ANALYSIS (RCTs): Antiplatelet Rx vs Placebo J Vasc Surg, 1999 FEMORAL–POPLITEAL–TIBIAL BYPASS PATENCY META-ANALYSIS (RCTs): Antithrombotic Rx vs Placebo Am J Med, 2004 FEMORAL–POPLITEAL–TIBIAL BYPASS STATIN Rx Brigham & Women’s Hosp Patients: Limb Salvage: Infrapopliteal: PRIMARY PATENCY 189 92% 65% SECONDARY PATENCY Statins Statins No Statins No Statins p= .25 J Vasc Surg, 2004 p< .02 TREATMENT OF CARDIOVASCULAR DISEASE CONTEMPORARY PRACTICE : > 70% OF OPEN OPERATIONS WILL BE REPLACED BY PERCUTANEOUS OR ENDOVASCULAR PROCEDURES PAOD REVASCULARIZATION Surgery vs Endovascular: 2002 - 2009 2002 42% 2009 70% Health Care Advisory Board Innovations Center Futures Database SURGERY ENDO PAOD REVASCULARIZATION Volume Projections: 2004 - 2009 400,000 +25% 350,000 300,000 # + 37% 250,000 200,000 150,000 + 4% 100,000 50,000 0 2004 Health Care Advisory Board Innovations Center Futures Database 2009 YEARS SURGERY ENDO TOTAL SFA OCCLUSIVE DISEASE Advantages of Endovascular Therapy Less Risk Less Morbidity Shorter LOS Acceptable Clinical Outcomes Cost Efficacy INFRAINGUINAL OCCLUSIVE DISEASE ENDOVASCULAR THERAPEUTIC OPTIONS PTA Stents Subintimal Angioplasty Drug Eluting Stents Covered Stents Bioabsorbable Stents Cutting Balloon PTA Cryoplasty Brachytherapy Excimer Laser Atherectomy Percutaneous Bypass x = Fem-Pop (Saph V.) J Vasc Surg, 2005 ACUTE ARTERIAL ISCHEMIA ACUTE LIMB ISCHEMIA TREATMENT GOALS PRIMARY: Restore Perfusion SECONDARY: Identify & Correct Underlying Lesions vs ACUTE LIMB ISCHEMIA: SEVERITY SVS CLINICAL CLASSIFICATION I. Viable Doppler Arterial. Venous SENSORY MOTOR - - + + +/- toes - - + - + - - II. Threatened: Marginally Immediately > toes III. Irreversible profound mild - mod paralysis ACUTE LIMB ISCHEMIA: ETIOLOGY THROMBOTIC (60%) EMBOLIC (40%) Bypass Graft Atherosclerotic Aneurysm Iatrogenic Nonatherosclerotic Cardiac Atherosclerosis Aneurysm Paradoxical Tumor “Cryptogenic” LOCATION Lower vs Upper Extremity Proximal vs Distal ACUTE LIMB ISCHEMIA BENEFITS OF THROMBOLYTIC THERAPY Restores Perfusion Controlled Reperfusion Maximizes Reperfusion Accurate Diagnosis Endovascular Intervention Avoids Emergency Surgery ACUTE LIMB ISCHEMIA: THROMBOLYSIS - RANDOMIZED CLINICAL TRIALS - U ROCHESTER: < 7 Days Ischemia UK SURG n=57 n=57 p 30-Day Amputation 30-Day Mortality 9% 12% 14% 18% ns ns 30-Day Cardiopulmonary Morbidity 30-Day M.I.: 16% 5% 49% 16% .001 .02 1-Yr Mortality Rate: 1-Yr Limb Salvage: 16% 82% 42% 82% .001 ns THROMBOSED POPLITEAL ANEURYSMS: - Thrombolysis vs Immediate Surgery - 30-DAY LIMB SALVAGE Institution (Year) U Penn (1993) U Rochester (1998) U Florence (2002) U Lausanne (2002) U Hosp Birmingham (2003) Lysis & Surgery Immediate Surgery 100% 100% 86% 83% 100% 57% 70% 77% LIMITATIONS OF THROMBOEMBOLECTOMY Leaves Residual Thrombus Mural Thrombus: Infra-Popliteal Vessels: (35% – 85%) Refined Catheters Angio-Directed Embolectomy Cannot Clear Branch Vessel Occlusion THROMBOLYTIC AGENTS: EVOLUTION AGENT t½ FIBRIN SPECIFICITY Streptokinase 23 min + Urokinase 16 min ++ Alteplase Retaplase Tenecteplase 4-5 min 14 min 20-24 min +++ ++ ++++ Prourokinase Staphylokinase Desmoteplase Plasmin Alfimeprase 7 min 6 min 40-50 x t-PA 0.1 sec N.A. ++ ++++ ++++ +++++ +++++ Percutaneous Mechanical Thrombectomy Devices Aspiration Devices AngioJet* Possis Medical, Minneapolis, MN Trellis* Bacchus Vascular, Santa Clara, CA Fino Bacchus Vascular, Santa Clara, CA Solera Bacchus Vascular, Santa Clara, CA Rescue Boston Scientific, Watertown, MA Oasis Boston Scientific, Watertown, MA Hydrolyser Cordis Endovascular, Miami, FL Gelbfish EndoVac NeoVascular Technologies, Brooklyn, NY Thrombex PMT System Edwards Life Sciences, Irvine, CA The Cleaner Rex Medical/Boston Scientific, Watertown, MA Xtrak Thrombectomy Device Xtrak Medical, Salem, NH Rotarex Straub Medical, Wangs, Switzerland X-Sizer EndiCOR Medical, San Clemente, CA Microfragmentation Devices Arrow-Trerotola Arrow International, Reading, PA Amplatz Clot Buster Microvena, White Bear Lake, MN Cragg brush Micro Therapeutics, Aliso Viego, CA Castaneda brush Micro Therapeutics, Aliso Viego, CA Ultrasound Devices Acolysis Angiosonics, Morrisville, NC Resolution 360 therapeutic wire Omnisonics, Wilmington, MA ACUTE LIMB ISCHEMIA: ANGIOJET Author Muller-Hulsbeck # Success 112 71% Lyis 18% Complications (%) Embolism (10%) Amputation (1.8%) Mortality (7%) Silva 22 95% 0% Embolism (9%) Amputation (5%) Mortality (14%) Wagner 50 52% 30% Embolism (6%) Amputation (8%) Mortality (0%) Kasirajan 86 84% 50% Embolism (2.3%) Amputation (11.6%) Mortality (9.3%) ACUTE LIMB ISCHEMIA - Contemporary Management VIABLE / MARG. THREATENED IMMEDIATELY THREATENED IRREVERSIBLE Arteriogram Embolus Thrombotic Thrombolysis Thrombolysis - UE - Distal LE Surgery Intra-Op Arteriogram +/- Intervention Surgery Intraoperative Thrombolysis Amputation