Oncotype - Tangence
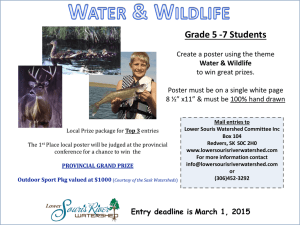
advertisement

Genomic Health Post-ASCO Clinical Data Review June 2011 Steve Shak, MD 2 Outline • The Biology Century – Principles for Evaluating Genomic Assays • Breast Cancer – Tumor Biology Matters: Supporting Data for the Recurrence Score ® in Predicting Neoadjuvant Therapy Response – Can You Consistently Predict the Recurrence Score with One or a Combination of Traditional Measures? – Practice and Health Economic Analyses • Colon Cancer – Confirmation Study (CALGB 9581) • Prostate Cancer – Identification of Prostate Cancer Genes Associated with Clinical Recurrence • Final Thoughts 3 Cancer – The Biology Century • Understanding and treating the underlying biology – Continual advances in technology – Basic research on cancer stem cells (CSC) – Circulating tumor cells – Integration of genomic analysis in the clinical context and the continuum of care 4 Evaluating Biomarkers for Clinical Use: Key Principles • Does the test deliver what patients, physicians, regulators, and payors need? – Most importantly, tests must be “Fit for Purpose” with evidence relevant to that specific purpose – Consistent results across multiple well-designed studies are required to provide evidence for analytic performance, clinical validity, and clinical utility (see Roadmap to Establish Clinical Utility) – Test must be shown to have value beyond traditional measures • Has the test been brought to a standardized implementation? And has the evidence which supports its use been obtained in that standardized implementation? Hayes DF. Am Soc Clin Oncol Ed Book. 30-34, 2008; Simon R. J Clin Oncol. 2005;23:7332-7341. 5 Roadmap to Establish Clinical Utility Define the purpose Technical feasibility Development studies Clinical validation studies, including comparative effectiveness Analytical methods validation Analytical methods finalization Treatment decision studies Health economic analysis 6 Key Questions When Evaluating Genomic Classifiers Strongly prognostic? Accurate and reliable? Predictive of chemotherapy benefit? Fit for purpose Incorporated in treatment guidelines? What is the level of evidence? 7 Selected Oncotype DX® Breast Abstracts at ASCO • Tumor Biology Matters: Supportive Data for the Recurrence Score® in Predicting Neoadjuvant Therapy Response – Masuda – RS as Predictor of Clinical Response to Neoadjuvant Exemestane in ER+ BC – Peacock – Exploratory Oncotype DX Assessment in HER2-Negative BC Receiving Ixabepilone-Cyclophosphamide Neoadjuvant Therapy • You Cannot Consistently Predict the Recurrence Score – Liebermann – Evaluation of RS and Traditional Clinical-Pathologic Assessments in a Large ER+, Node-Negative Cohort (Israel) • Practice & Health Economic Analyses – Chen – Evaluating Utilization Characteristics for Oncotype DX in ESBC (USO Network) – Hassan – Cost Benefit Analysis of 21-gene assay in Canadian healthcare system RS, Recurrence Score Tumor Biology Matters: Supportive Data for the Recurrence Score® Result in Predicting Neoadjuvant Therapy Response A Study of the Recurrence Score® by the 21-Gene Signature Assay as a Predictor of Clinical Response to Neoadjuvant Exemestane for 24 Weeks in Estrogen Receptor-Positive Breast Cancer N. Masuda, M. Toi, T. Ueno, T. Yamanaka, S. Saji, K. Kuroi, N. Sato, H. Takei, Y. Yamamoto, S. Ohno, H. Yamashita, K. Hisamatsu, K. Aogi, H. Iwata, S. Saji, H. Sasano National Hospital Organization Osaka National Hospital, Osaka, Japan; Breast Surgery, Kyoto University, Kyoto, Japan; Kyoto University Hospital, Kyoto, Japan; National Kyushu Cancer Center, Fukuoka, Japan; Saitama Medical University, International Medical Center, Saitama, Japan; Tokyo Metropolitan Cancer and Infectious Diseases Center, Komagome Hospital, Tokyo, Japan; Niigata Cancer Center Hospital, Niigata, Japan; Saitama Cancer Center, Saitama, Japan; Department of Breast and Endocrine Surgery, Kumamoto University, Kumamoto, Japan; Nagoya City University Graduate School of Medical Sciences, Nagoya, Japan; Hiroshima City Asa Hospital, Hiroshima, Japan; National Hospital Organization Shikoku Cancer Center, Eihme, Japan; Aichi Cancer Center Hospital, Nagoya, Japan; Japanese Foundation for Multidisciplinary Treatment of Cancer, Tokyo, Japan; Tohoku University Hospital, Sendai, Japan Masuda N, et al. ASCO 2011. Abstract 558 (poster presentation). 10 Objectives • This exploratory study was conducted to investigate the clinical usefulness of the 21-gene signature assay (Oncotype DX®) for prediction of the response to neoadjuvant Exemestane therapy in postmenopausal patients with hormone receptor-positive locally advanced stage II or IIIA breast cancer • Primary objective – Association between the Recurrence Score® (RS) determined on core biopsy specimens obtained at baseline and clinical response (defined as ≥50% reduction in area on imaging after 24 weeks) • Secondary objectives – Association of baseline quantitative ER by RT-PCR and Ki-67 by Central IHC with clinical response – Association of changes from baseline to post-treatment values of RS, quantitative ER by RT-PCR and Ki-67 by Central IHC with clinical response – Association of baseline RS, quantitative ER by RT-PCR and Ki-67 by Central IHC with breast-conserving surgery (BCS) vs. mastectomy Masuda N, et al. ASCO 2011. Abstract 558 (poster presentation). 11 Primary Analysis: Core Biopsy Recurrence Score® Result and Clinical Response RS Group Clinical Response Low (< 18) 19/32 = 59.4% Intermediate (18 - 30) 10/17 = 58.8% High (≥ 31) 3/15 = 20.0% p=0.015 for Comparison Between Low and High RS Groups (2-sided Fisher’s exact test) RS, Recurrence Score Masuda N, et al. ASCO 2011. Abstract 558 (poster presentation). 12 Logistic Regression Analyses of Baseline Core Biopsy RS in Predicting Clinical Response Model Odds Ratio (95% CI) p-value Int. vs. Low 0.977 (0.296, 3.233) 0.970 High vs. Low 0.171 (0.040, 0.728) 0.017 2 Continuous RS/50 0.205 (0.044, 0.946) 0.042 3 Age (years) 1.012 (0.926, 1.106) 0.795 Tumor Size (mm) 1.033 (0.960, 1.112) 0.387 Continuous RS/50 0.172 (0.034, 0.858) 0.032 1 • • Effect RS Group When analyzed by RS groups, the low and intermediate RS groups had similar odds of clinical response, whereas the high RS group had significantly lower odds of clinical response When analyzed as a continuous score, a lower RS was significantly associated with a higher odds of clinical response in both unadjusted and covariate-adjusted (for age and tumor size) analyses. RS, Recurrence Score® Masuda N, et al. ASCO 2011. Abstract 558 (poster presentation). 13 Logistic Regression Analysis of Baseline Core Biopsy ER by RT-PCR and Ki-67 by IHC in Predicting Clinical Response Model Effect • • Odds Ratio (95% CI) p-value 4a Continuous ER by RT-PCR 1.436 (0.963, 2.141) 0.076 4b Age (years) 0.980 (0.897, 1.072) 0.665 Tumor Size (mm) 1.017 (0.950, 1.090) 0.624 Continuous ER by RT-PCR 1.480 (0.975, 2.246) 0.066 5a Continuous Ki-67 by IHC 0.981 (0.948, 1.015) 0.273 5b Age (years) 1.023 (0.934, 1.121) 0.627 Tumor Size (mm) 1.025 (0.955, 1.100) 0.502 Continuous Ki-67 by IHC 0.976 (0.940, 1.013) 0.197 The association between quantitative ER by RT-PCR and clinical response was of borderline statistical significance Baseline Ki-67 by IHC was not associated with clinical response Masuda N, et al. ASCO 2011. Abstract 558 (poster presentation). 14 Logistic Regression Analyses of Changes in Markers From Core Biopsy to Resection in Predicting Clinical Response Model Variable Odds Ratio (95% CI) p-value 6 Change from Baseline to Post-Treatment RS/50 0.198 (0.013, 2.952) 0.240 7 Change from Baseline to Post-Treatment ER by RT-PCR (CT) 0.753 (0.419, 1.354) 0.343 8 Change from Baseline to Post-Treatment Ki-67 by IHC (%) 1.011 (0.967, 1.057) 0.629 Changes from pre-treatment to post-treatment values in Recurrence Score®, ER by RTPCR or Ki-67 by central IHC were not associated with clinical response RS, Recurrence Score Masuda N, et al. ASCO 2011. Abstract 558 (poster presentation). 15 Logistic Regression of Baseline Core Biopsy Markers in Predicting Breast Conserving Surgery (BCS) Unadjusted Adjusted for Tumor Size and PgR Allred Score Marker Odds Ratio (95% CI) pvalue Odds Ratio (95% CI) pvalue RS/50 0.055 (0.009, 0.323) 0.001 0.016 (<0.001, 0.259) 0.004 ER by RT-PCR 1.786 (1.150, 2.774) 0.001 1.881 (1.090, 3.245) 0.023 Ki-67 by IHC 0.957 (0.921, 0.994) 0.024 0.953 (0.907, 1.002) 0.060 • Lower Recurrence Score® result, higher ER by RT-PCR, and lower Ki-67 by central IHC were all significantly associated with greater odds of breast-conserving surgery • When adjusted for the effects of tumor size and PgR Allred Score, RS and ER by RT-PCR maintained their significance, and Ki-67 was of borderline significance RS, Recurrence Score Masuda N, et al. ASCO 2011. Abstract 558 (poster presentation). 16 Recurrence Score® Result, Ki-67 and Prediction of BCS Relationship Between Core Biopsy RS and Core Biopsy Ki-67 by IHC Core Biopsy RS and Breast Conserving Surgery RS Group BCS Low (< 18) 29/32 = 90.6% Intermediate (18 - 30) 13/17 = 76.5% High (≥ 31) 7/15 = 46.7% p=0.002 for Comparison Between Low and High RS Groups (2-sided Fisher’s exact test) Multivariable Analysis of Core Biopsy RS and Ki-67 and Breast Conserving Surgery Effect Odds Ratio (95% CI) p-value RS/50 0.048 (0.004, 0.514) 0.012 Ki-67 by IHC 1.005 (0.949, 1.064) 0.868 RS, Recurrence Score Masuda N, et al. ASCO 2011. Abstract 558 (poster presentation). • Recurrence Score and Ki-67 by central IHC are moderately correlated (Spearman correlation coefficient = 0.672, 95% CI 0.506-0.785) • When Recurrence Score and Ki-67 by central IHC were included in the same logistic regression model, Recurrence Score was the only statistically significant predictor of breast-conserving surgery. 17 Summary and Conclusions • Pre-treatment Recurrence Score® result from the core biopsy predicts clinical response to 24 weeks of neoadjuvant exemestane – Approximately 60% of the patients in the low and intermediate RS groups experienced a clinical response as compared with 20% in the high RS group – The significance of the associations persisted when adjusting for traditional baseline factors • A low RS in the core biopsy is significantly associated with a greater likelihood of undergoing BCS which carries an overall better outcome for patients (lower morbidity and better cosmesis than mastectomy) • Pre-treatment Ki-67 by central IHC was significantly associated with BCS, but not when adjusted for the RS – Changes from core biopsy to resection in RS, ER by RT-PCR and Ki-67 by central IHC were not associated with clinical response • Neoadjuvant endocrine treatment may be an effective option in patients with low or intermediate RS disease RS, Recurrence Score Masuda N, et al. ASCO 2011. Abstract 558 (poster presentation). Ixabepilone and Cyclophosphamide as Neoadjuvant Therapy in HER2-Negative Breast Cancer with Exploratory Oncotype DX® Assessments: A Sarah Cannon Research Institute Phase II Trial Nancy W. Peacock MD1,2, Denise A. Yardley MD1,2, Carolyn Hendricks MD3, Sang Yoon Huh MD4, Sarah Ketchum MD5, Calvin Chao MD6, Carl Yoshizawa PhD6, Mythili Shastry PhD1, Brian Strike MS1, Howard A. Burris MD1,2, John D. Hainsworth MD1,2 1Sarah Cannon Research Institute, Nashville, TN; 2Tennessee Oncology, PLLC, Nashville, TN; 3Center for Cancer and Blood Disorders, Bethesda, MD; 4Providence Medical Group, Terre Haute, IN; 5Mercy Hospital, Portland, ME; 6Genomic Health, Redwood City, CA Peacock NW, et al. ASCO 2011. Abstract 1066 (poster presentation). 19 Exploratory Oncotype DX® Assessments • The Oncotype DX Breast Cancer Assay uses reverse transcriptase-polymerase chain reaction (RT-PCR) to assess a panel of 21 genes in tumor tissue to calculate a score predictive of the probability of recurrence (Paik et al 2004) • In this study, Oncotype DX Recurrence Score® results were calculated from tumor tissue obtained at baseline and after neoadjuvant therapy in this ER+/ER- patient population • Recurrence Score results were then correlated with pCR rate. These correlations may provide preliminary information regarding the use of the Oncotype DX assay to predict response to neoadjuvant chemotherapy Peacock NW, et al. ASCO 2011. Abstract 1066 (poster presentation). 20 Oncotype DX® Assessments (N=38) Paired Oncotype DX assessments (baseline biopsy and surgical specimen) were available for 38 patients at the time of the interim analysis. p=0.025 from logistic regression Correlation of Recurrence Score® result and pCR (38 patients; 7 pCR events) High Int. Low No Yes Pathologic Complete Response Peacock NW, et al. ASCO 2011. Abstract 1066 (poster presentation). 21 Correlation Between Recurrence Score® and pCR Rate • The interim assessment of Oncotype DX® Recurrence Score values indicated that high Recurrence Scores from the core biopsy may predict a higher likelihood of pCR with neoadjuvant ixabepilone/cyclophosphamide. • Recurrence Score values from the pre-treatment core biopsy and the post-treatment surgical specimen were similar in most patients (Spearman r = 0.81, 95% CI: 0.56-0.92) Peacock NW, et al. ASCO 2011. Abstract 1066 (poster presentation). 22 Patients with a Low Recurrence Score® Result Are Less Likely to Respond to Neoadjuvant Chemotherapy Neoadjuvant Anthracyline-Taxane Treatment (N=89) Neoadjuvant Docetaxel Treatment (N=72) P=0.005 P=0.0079 Gianni L, et al. J Clin Oncol. 2005;23(29):7265-7277. Chang JC, et al. Breast Cancer Res Treat. 2008;108 (2):233-240. 23 The Precision of the Recurrence Score® Result Defines Individual Biology for ER+ Breast Cancer Distant recurrence at 10 years CONTINUOUS BIOLOGY 40% 35% 30% 25% 20% 15% 10% 5% 0% 0 5 10 15 20 25 30 35 40 45 50 Recurrence Score value LOW RECURRENCE SCORE DISEASE Indolent Hormone therapy-sensitive Minimal, if any, chemotherapy benefit HIGH RECURRENCE SCORE DISEASE Aggressive Less sensitive to hormone therapy Large chemotherapy benefit Paik S, et al. N Engl J Med. 2004;351:2817; Paik S, et al. J Clin Oncol. 2006;24:3726; Habel LA, et al. Breast Cancer Res. 2006;8:R25-R39. Can You Consistently Predict the Recurrence Score® Result with One or a Combination of Traditional Measures? Evaluation of Recurrence Score® and Traditional Clinicopathologic Assessments in a Large Estrogen Receptor-Positive, Lymph NodeNegative Patient Cohort Liebermann N,1 Baehner FL,2,3 Soussan-Gutman L, Klang S, Yoshizawa C,3 Shak S,3 Siegelmann-Danieli N 1Clalit Health Services, Tel Aviv, Israel; 2University of California, San Francisco, San Francisco, CA; 3Genomic Health, Inc., Redwood City, CA; 4Teva Pharmaceutical Industries, Netanya, Israel; 5Maccabi Health Organization, Tel-Aviv, Israel Liebermann N, et al. ASCO 2011. Abstract 632 (poster presentation). 26 Objectives • To examine, in a large cohort of ER-positive (ER+), HER2-negative (HER2-), lymph node-negative (LN-) patients selected for the Oncotype DX® breast cancer assay, the distribution of the Recurrence Score® (RS) result and RS groups, within individual and joint categories of age, tumor size, and grade. Liebermann N, et al. ASCO 2011. Abstract 632 (poster presentation). 27 Spearman Correlation Coefficients for Continuous Recurrence Score® Result with Individual Prognostic Factors n Spearman Correlation With Continuous RS 95% CI Age (years) 1864 -0.09 (-0.13, -0.04) Tumor Size (cm) 1849 0.07 (0.02, 0.12) Tumor Grade 1530 0.33 (0.28, 0.37) Characteristic RS is poorly correlated with age and tumor size, and modestly correlated with tumor grade. RS, Recurrence Score Liebermann N, et al. ASCO 2011. Abstract 632 (poster presentation). 28 Recurrence Score® (RS) Groups by Age / Tumor Size / Tumor Grade RS Groups by Patient Age <50 yrs (n=367) RS Groups by Tumor Grade Grade 1 (n=277) ≥50 yrs (n=1497) Grade 2 (n=964) RS Groups by Tumor Size Grade 3 (n=289) ≤2 cm (n=1447) >2 cm (n=402) • Not all grade 1 tumors have low RS values. • Only 31% of grade 3 tumors have high RS values. • Small tumors have proportionately fewer high RS values. • However, there is a range of RS values across both categories of tumor size. Liebermann N, et al. ASCO 2011. Abstract 632 (poster presentation). 29 Recurrence Score® (RS) Groups by Age / Tumor Size / Tumor Grade RS Groups by Age and Tumor Size Age <50 yrs, Size ≤2 cm (n=302) Age <50 yrs, Size >2 cm (n=64) • The likelihood of a high RS value in tumors >2 cm is approximately twice that for tumors ≤2 cm. • However, there is a range of RS values for each category of age and size. Age ≥50 yrs, Size ≤2 cm (n=1145) Age ≥50 yrs, Size >2 cm (n=338) RS Groups by Age and Tumor Grade Age <50 yrs, Grade 1 (n=56) Age <50 yrs, Grade 2 (n=197) Age <50 yrs, Grade 3 (n=66) Age ≥50 yrs, Grade 1 (n=221) Age ≥50 yrs, Grade 2 (n=767) RS Groups by Tumor Size & Tumor Grade Age ≥50 yrs, Grade 3 (n=223) Size ≤2 cm, Grade 1 (n=247) Size ≤2 cm, Grade 2 (n=775) • There are relatively few high RS values among patients with low grade, but not all low grade tumors have low Recurrence Scores. • There is otherwise a wide range of Recurrence Scores among joint categories of grade and tumor size. Size ≤2 cm, Grade 3 (n=194) Size >2 cm, Grade 1 (n=29) Size >2 cm, Grade 2 (n=183) Size >2 cm, Grade 3 (n=37) Liebermann N, et al. ASCO 2011. Abstract 632 (poster presentation). 30 Summary and Discussion • There is a range of Recurrence Score® biology across patient age, tumor size, and tumor grade in lymph node-negative, ER-positive early stage breast carcinoma • The correlations between the Recurrence Score and these clinicopathologic factors are small for age and tumor size, and modest for tumor grade • The Recurrence Score cannot be predicted by traditional clinicopathologic variables Liebermann N, et al. ASCO 2011. Abstract 632 (poster presentation). Practice and Health Economic Analyses Evaluating Utilization Characteristics for the Oncotype DX® Recurrence Score® Chen C, Patt DA, Kazzaz D, Shankleton J, Forsyth M, Ganesh R Department of Healthcare Informatics, US Oncology Network, The Woodlands, Texas Chen C, et al. ASCO 2011. Abstract 625 (poster presentation). 33 Objective • Primary Objective – To determine whether practice or patient characteristics drive Oncotype DX® testing and whether there is an association between the results of the Oncotype DX test and the patient’s likelihood of receiving chemotherapy • Secondary Objectives – To determine, of breast cancer patients in the US Oncology Network who are eligible for Oncotype DX testing, how many received the test – To determine whether there are patient or practice characteristics that influence whether patients receive Oncotype DX testing Chen C, et al. ASCO 2011. Abstract 625 (poster presentation). 34 Summary and Discussion • Clinical factors influenced whether patients received the Oncotype DX® assay in the USO Network – Oldest patients (>76) had decreased utilization of Oncotype DX – Utilization is greatest in patients with tumors on the border of chemotherapy choice as dictated by pre-Oncotype DX guidelines (T1b, T1c, T2 tumors) – Utilization diminished in the very small (T1a) and very large (T3 & T4) tumors where decisions were likely based on size, given favorable pathology • Oncotype DX testing influences decision-making about whether to incorporate chemotherapy into the care of patients with early-stage breast cancer Chen C, et al. ASCO 2011. Abstract 625 (poster presentation). A Cost-Benefit Analysis of the 21-Gene Breast Cancer Assay within a Canadian Health Care System S Hassan1, N Mittmann1,2 1 Health Outcomes & PharmacoEconomics (HOPE) Research Centre, Division of Clinical Pharmacology, Department of Medicine, Sunnybrook Health Sciences Centre, Toronto 2 Department of Pharmacology, University of Toronto, Toronto Hassan S and Mittmann N. ASCO 2011. Abstract 6111 (poster presentation). 36 Cost Benefit Analysis of the 21-Gene Breast Cancer Assay within a Canadian Health Care System • Objective – To quantify budget impact relative to the addition of the 21BCA to a Canadian provincial framework • Conclusion – In this analysis model, all patients with low Recurrence Score® (RS) results and 50% of intermediate RSs avoided chemotherapy – The budget impact of the cost of the 21BCA would be offset by a reduction in costs associated with treatment. The use of the 21BCA in BC patients using this model would have resulted in more than $11M (CDN) per year in savings to the health care system – This conservative analysis may show even greater costs savings if adverse event costs were considered Hassan S and Mittmann N. ASCO 2011. Abstract 6111 (poster presentation). Validation of a 12-Gene Colon Cancer Recurrence Score® in Stage II Colon Cancer Patients from CALGB 9581 A.P. Venook1, D. Niedzwiecki2, M. Lopatin3, M. Lee3, P. N. Friedman4, W. Frankel5, K. Clark-Langone3, C. Yoshizawa3, C. Millward3, S. Shak3, R. M. Goldberg6, N. N. Mahmoud7, R. L. Schilsky4, M. M. Bertagnolli8 1. University of California, San Francisco, San Francisco, CA; 2. Duke University, Durham, NC; 3. Genomic Health, Redwood City, CA; 4. The University of Chicago, Chicago, IL; 5. The Ohio State University, Columbus, OH; 6. University of North Carolina at Chapel Hill, Chapel Hill, NC; 7. University of Pennsylvania, Philadelphia, PA; 8. Brigham and Women's Hospital, Boston, MA Venook AP, et al. ASCO 2011. Abstract 3518 (poster presentation). 38 CALGB 9581: A Unique Opportunity to Test the Oncotype DX® Assay in Low/Standard Risk Stage II Colon Cancer • Sampling design with 690 evaluable patients, including 162 recurrence events, representative of 1,672 stage II colon cancer patients from CALGB 9581 • A population where risk discrimination is challenging with conventional clinical and pathologic factors Venook AP, et al. ASCO 2011. Abstract 3518 (poster presentation). Patient Characteristics of the Validation Studies Characteristic | CALGB | QUASAR 39 CALGB 9581: Second Successful Prospectively-Designed Confirmation Study Relationship Between RS and Risk of Recurrence at 5 Years RS, Recurrence Score® Venook AP, et al. ASCO 2011. Abstract 3518 (poster presentation). 40 CALGB 9581: Improving the Ability to Discriminate High vs. Low Risk of Recurrence in Standard Risk Stage II Colon Cancer Ability to Discriminate High vs Low Risk of Recurrence: RS Group % of Patients RS, Recurrence Score® Venook AP, et al. ASCO 2011. Abstract 3518 (poster presentation). Average 5-Year Recurrence Risk for T3 MMR-P Patients (95% Cl) Quantitative Gene Expression in Primary and Highest Gleason Patterns Identifies Genes Associated with Clinical Recurrence in Prostate Cancer After Radical Prostatectomy Eric A Klein1, Sara M Falzarano2, Tara Maddala3, Carl Millward3, William F Novotny3, Robert J Pelham3, Diana Cherbavaz 3, Cristina Magi-Galluzzi2 Cleveland Clinic 1Glickman Urological and Kidney Institute and 2Pathology and Laboratory Medicine Institute, Cleveland Clinic 3 Genomic Health, Inc., Redwood City, CA Klein EA, et al. ASCO 2011. Abstract 4663 (poster presentation). 42 Prostate Cancer Is Widely Over-treated to Benefit Very Few Need Is Clear • >750,000 biopsies1; 200,000 cancers diagnosed2 (U.S. 2009) • Vast majority get aggressive surgery/radiation therapy; <10% patients choose active surveillance 1 Marks et al, Urology 2007; 69:532. 2 Jemel et al, CA Cancer J Clin 2009;59: 225-249. 43 Which Men Have Clinically Significant Prostate Cancer Requiring Treatment? • Surgery and radiation therapy are common treatments for prostate cancer • However – Between 19 and 48 men have to be treated to prevent one death from prostate cancer – Over 50% of men suffer incontinence and/or impotence after surgery Schröder FH et al, N Engl J Med. 2009; 360:1320-1328. 44 Unique Challenges in Prostate Cancer • Small tumors common and biopsy tissue very small; required modification of our RT-PCR platform for lower input RNA • Multi-focal disease common; sampling with standard biopsy procedures may confound accurate prediction of risk 45 Study Objectives • Overall Objective – Development of a biopsy-based genomic assay to discriminate indolent from aggressive prostate cancer • Objective of Current Study: – Quantitative assay of gene expression in radical prostatectomy (RP) tissue • Identify genes whose expression predicts clinical recurrence after RP • Assess the ability of gene expression to predict clinical recurrence (cR) in the context of Gleason grade heterogeneity • Assess the ability of gene expression to provide recurrence risk information beyond that provided by Gleason grade Klein EA, et al. ASCO 2011. Abstract 4663 (poster presentation). 46 Patients, Samples, Methods, and Genes 2,600 Patients with RP 1987-2004 501 Patients Selected 127 Clinical Recurrence 374 Disease Free Quantitative RT-PCR using Oncotype DX® RT-PCR technology for 738 Genes 6 Reference Genes 732 Cancer-Related Genes 51 Excluded for insufficient tumor 7 Did not meet inclusion criteria 2 Outlier gene profile 441 Patients Evaluable for Clinical /Pathology/Gene Expression Klein EA, et al. ASCO 2011. Abstract 4663 (poster presentation). 5 Cancer genes excluded 727 Evaluable Cancer Genes 47 Methods Specimens re-reviewed centrally for assignment of stage & grade (2005 Consensus) Manual microdissection Two tumor foci separately analyzed Primary Gleason pattern Highest Gleason pattern RNA extraction Gleason Pattern 3 Gleason Pattern 4 RT- PCR for each gene Data analysis Identify specific gene expression levels associated with outcome (cR, bR, PCSS) Cox regression controlling the false discovery rate at 10% Klein EA, et al. ASCO 2011. Abstract 4663 (poster presentation). 48 Genes are Associated with Clinical Recurrence in Both Sample No. of Genes Associated with Clinical Recurrence Primary Gleason Pattern 295 Highest Gleason Pattern 297 Both Primary and Highest Gleason Pattern 235 HR for association of gene expression with cRFI in HGP the Primary and Highest Gleason Pattern Samples 2.4 1.6 1.0 0.7 0.4 0.4 0.7 1.0 1.6 2.4 HR for association of gene expression with cRFI in PGP Genes significantly associated with cRFI in both PGP and HGP Genes significantly associated with cRFI in PGP only Genes significantly associated with cRFI in HGP only Genes not significantly associated with cRFI in PGP or HGP \\Lims\medical\Prostate\CCFProstateGI(09-002)\Analysis\USCAP_2011\Programs\g_ScatterStdHRcRFI_PGPvHGP.sas Klein EA, et al. ASCO 2011. Abstract 4663 (poster presentation). 12JAN2011:1459 SCL:00.05.96 tmaddala 49 Genes Associated With Clinical Outcome Cluster Into Co-Expression Groups with Related Biological Functions Klein EA, et al. ASCO 2011. Abstract 4663 (poster presentation). 50 Hazard Ratios for Genes Associated with Clinical Recurrence in Both Primary and Highest Gleason Pattern Samples Univariate Std. HRs for cRFI Cox PH Regression Worse Outcome Better Outcome Stress DUSP1 FOS Migration GSTM2 PPAP2B Proliferation BIRC5 TOP2A ECM COL3A1 FAP 0.3 0.6 1.0 1.8 Std. Hazard Ratio for Clinical Recurrence Stnd Hazard Ratio for ClinicalPrimary Recurrence Highest \\L i m s \m e d i c a l \Pro s ta te \CCFPro s ta te GI(0 9 -0 0 2 )\An a l y s i s \AAGUS\Pro g ra m s \g _ Fo re s tc RFIStd HR4 Ge n e Grp _ x GP.s a s Klein EA, et al. ASCO 2011. Abstract 4663 (poster presentation). 3 0 M AR2 0 1 1 :1 2 2 6 SCL :0 0 .0 6 .0 5 j y u e 3.2 51 Each Gene Group Add Prognostic Value Beyond Clinical and Pathological Covariates Worse Outcome Better Outcome DUSP1 Stress FOS Unadjusted GSTM2 Adj. for path Tstage PPAP2B Adj. for surgical GS BIRC5 Adj. for Gleason pattern TOP2A Adj. for CAPRA risk group COL3A1 Adj. for AUA risk group Migration Proliferation ECM FAP 0.3 0.6 1.0 1.8 Std. Hazard Ratio (95% CI) Std. HR (95% CI) AUA Klein EA, et al. ASCO 2011. Abstract 4663 (poster presentation). GP CAPRA GS 3.2 52 Gene Expression Predicts for All Clinically Important Endpoints Better Outcome Worse Outcome DUSP1 Stress FOS cRFI GSTM2 Migration bRFI PPAP2B Upgrade/ Upstage BIRC5 Proliferation PCSS TOP2A ECM COL3A1 FAP 0.3 0.6 1.0 1.8 Std. Relative Risk Estimate (95% CI) (log scale) PCSS Klein EA, et al. ASCO 2011. Abstract 4663 (poster presentation). UpRsk 3.2 Final Thoughts 54 Genomic Health’s Research is Focused on Optimizing Cancer Treatment Breast Renal Colon Prostate 55 Closing Thoughts • Importance of understanding and treating the underlying individual tumor biology • Importance of standardizing emerging “next generation” technologies • Genomic assays for clinical decision-making must be “Fit for purpose” – Clinically validated in prospectively-designed studies of sufficient size and statistical power – Supported by evidence in target patient population, with demonstrated value beyond existing measures – Standardized and reproducible – Practical and clinically impactful