P3_Spencer Liu
advertisement

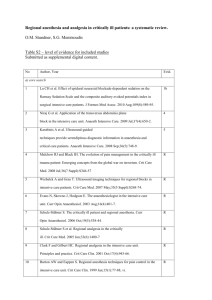
Postoperative pain control What to do after PCA? Spencer S. Liu, MD Clinical Professor of Anesthesiology Director Acute and Recuperative Pain Services Disclosure HSS educational activities are carried out in a manner that serves the educational component of our Mission. As faculty we are committed to providing transparency in any/all external relationships prior to giving an academic presentation. Spencer S. Liu, MD Hospital for Special Surgery Disclosure: I do not have a financial relationship with any commercial interest. Background • Postoperative pain is a key issue for patients • Large surveys indicate patients are more concerned about pain (59%) than surgical outcome (51%) • Unfortunately, this concern remains justified Anesth Analg 2003:97:534 Background • Multiple surveys report continued poor postoperative pain control • Most recently in 2003 – 250 adults – Mix of in-patient and ambulatory – 75% reported experiencing pain during or after surgery – 73% reported moderate to severe pain Is postoperative pain that bad? • Inherently, who wants pain – Guidelines from: • WHO • APS • ASA • Regulatory requirement: JCAHO • Key patient satisfaction surveys: Press Ganey • Pain can create bad outcomes – Morbidity – HRQOL – Development of chronic pain Anesth Analg 2007:104:689 Anesth Analg 2007:105:789 What can one do? • Acute Pain Services are popular and effective • Typically expensive • Typically manage PCA modalities Anesth Analg 2002:95:1361 Anesthesiology. 104(5):1033-1039,2006 13 How well is pain controlled after the APS signs off? • What happens after the APS signs off? • Typically, the surgeons alone manage postoperative pain with po analgesia and write the home prescriptions • Not so good per patient surveys • Same here at HSS • In March 2007 – Negative patient letters Recuperative Pain Medicine • RPM rolled out in August 2007 – Recurrent negative themes in patient letters, comments, and New York Times editorials • Post-PCA patients experienced inadequate pain management with oral analgesics • Post-PCA patients did not have easy access to a pain management expert Based on these reports, a plan was formed • Multidisciplinary team – Surgeon in Chief – Anesthesiologist in Chief – Executive Leadership – Director of Risk Management – Director of APS – Director of CPS – CAMS – Director of Patient education Patient Education and Pain Management Preoperative “Pre-emptive” medications Education Postoperative PCA APS Postoperative PO Pain management Patient education Staff education How to measure impact? • No currently standardized, validated tools • We chose 3 outcome measure for before and after implementation measurement – Press Ganey Survey • Administered to all postoperative patients to assess satisfaction • Has specific questions on pain management • Benchmarked against similar institutions – Staff satisfaction survey – Number of calls to Helpline • Less is better • Do all the work upfront Preoperative educational role of RPM • Worked with Patient education to update and expand sections on perioperative analgesia for pre-operative patient education classes for total joint replacement and spine surgery Clinical role of RPM • Designed to fill identified gaps • Provide a seamless transition from the IV/Epidural PCA to oral medications • Continued pain management monitoring thru to discharge. • The RPM service collaborates with both the Acute Pain Service and Chronic Pain Service. Administrative and Educational Role of RPM for postoperative care • Created discharge medication policy – Correct meds – Enough pain meds until first FU visit • Created discharge booklet – Written resource for patients on basic pain management information. • Expectations for pain control • Common pain medications • Common expected side effects – All inpatients receive at discharge. Patient Education and Pain Management Preoperative “Pre-emptive” medications Education Postoperative PCA APS Postoperative PO Pain management Patient education Staff education RPM Patient Volume 2007 • Since August 2007, the volume of inpatient consults has steadily increased yearly • Confirming need for further medical pain management after discontinuation of PCA therapy. 2008 2009 2010 Jan 0 74 107 102 Feb 0 60 92 81 Mar 0 48 76 101 Apr 0 76 100 116 May 0 49 96 107 Jun 0 68 103 90 Jul 0 53 117 83 Aug 0 86 90 108 Sep 16 142 86 128 Oct 56 62 104 154 Nov 56 103 81 106 Dec 24 60 74 156 152 881 1126 Total 1332 Results of RPM Implementation • Our primary outcome measure was the Press Ganey satisfaction survey. 100 • Philips, B., Liu, S., et al. “Creation of a Novel Recuperative Pain Medicine Service to Optimize Postoperative Analgesia and Enhance Patient Satisfaction”,HSS Journal (February 2010). Percentile Ranking 95 90 85 80 75 2008 2008 2008 2008 2009 2009 2009 2009 2010 2010 2010 1st 2nd 3rd 4th 1st 2nd 3rd 4th 1st 2nd 3rd Quart Quart Quart Quart Quart Quart Quart Quart Quart Quart Quart 91 97 99 97 98 99 99 99 99 99 99 Magnet PG 84 97 99 98 97 99 99 98 99 98 97 92 92 99 90 99 99 99 99 99 99 99 Large PG HSS PG RPM HelpLine Start of RPM/ARJR Pilot Program (October 2010) 50 45 40 35 30 25 Number of Phonecalls 20 15 10 5 Jan-11 Nov-10 Sep-10 Jul-10 May-10 Mar-10 Jan-10 Nov-09 Sep-09 Jul-09 May-09 Mar-09 Jan-09 0 Staff satisfaction survey • Returned by – 81 RNs – 7 surgical PAs • 92% rated RPM as extremely helpful Cost of RPM • Cost for an NP ~ 150,000 USD • 12.5-15 USD/pt visit • Could also use a Physician’s Assistant Number of PCAs 14000 12000 10000 8000 6000 4000 2000 0 2009 2010 Systemic multimodal analgesia NSAIDs, COX2, Acetaminophen Impact of Reuben retractions • NSAIDs – No effect as no RCT retracted • COX2 – Only 1 RCT with 60 patients retracted – One additional RCT demonstrating analgesic benefit with celecoxib in TKR • BMC Musculoskelet Disord 2008;9:77. • Acetaminophen – No effect as no RCT retracted Gabapentin Figure 1. Flow diagram of the review Tiippana, E. M. et al. Anesth Analg 2007;104:1545-1556 Copyright restrictions apply. Figure 2. Pain intensity difference between the control and gabapentin groups (PIDc-g) at rest (panel A) and on movement (panel B) on VAS 0-100 during 24 h observation after a single 1200 mg dose 1-2 h before surgery Tiippana, E. M. et al. Anesth Analg 2007;104:1545-1556 Copyright restrictions apply. Figure 3. Effect of preoperative gabapentin on postoperative opioid consumption Tiippana, E. M. et al. Anesth Analg 2007;104:1545-1556 Copyright restrictions apply. Side effects • Reduction in opioid related side effects – Nausea: NNT=25 – Vomiting: NNT=6 – Urinary retention: NNT=7 • Adverse effects – Sedation: NNH=35 – Dizziness: NNH=12 Pregabalin • Laparoscopic hysterectomy – Opioid sparing – Increased dizziness • Laparoscopy – Better analgesia – Trend toward increased dizziness • Laparoscopic cholecystectomy – Better analgesia – Opioid sparing BJA 2008:101:700 Conclusions • Discussed agents are efficacious • Modest benefit • NSAIDs and gabapentanoids have most to offer – Reduced opioid consumption – Reduced side effects – NSAIDs have more risk Non-traditional techniques • • • • Acupuncture Music Static magnet Massage Acupuncture Anesth Analg 2008:106:611 Acupuncture • May also depend on belief system • 47/47 studies from China, Japan, and Taiwan found efficacy • 53/96 studies from US, UK, and Sweden found efficacy Music Music • Several RCTs • Soft, relaxing music vs none during general anesthesia – Open inguinal hernia repair – Varicose vein stripping – Hysterectomy • Very modest and short lived benefit from music Acta Anaesthesiol Scand 2003:47, 278 Acta Anaesthesiol Scand 2001:45, 812 Eur J Anaesthesiol 2005:22, 96 Ambulatory procedures Intraop music 4.2 Pain in PACU (0-10) Patient 4 satisfaction Morphine 14.4 (mg) Control 3.9 3.9 16.9 Anesth Analg 2010:110:208 Magnet therapy • Multi-billion dollar industry • Mecanisms? – Increased blood flow – Altered neuron firing thresholds Massage Summary • RPM service is efficacious – Probably cost effective – Can use different staffing models • Optimize systemic analgesics • Role of CAMS? – Acupuncture has best evidence