Document
advertisement

Today’s Webinar will begin at 11 PST
7/19/12
Welcome from Barb DeBaun, RN, MSN, CIC
Introduction
• Please do not put your phone on hold; use the
mute function or *6
• Please type questions or comments into text
box
• If time permits, we will open up the phone
lines at the conclusion of the presentation
Katy Loos, RN, MSN
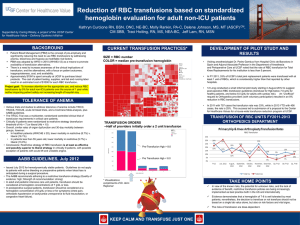
PATIENT BLOOD MANAGEMENT
Katy Loos RN, MSN
GOOD SAMARITAN HOSPITAL
CINCINNATI, OH
OBJECTIVES
Identify areas of practice ready for change
Implement strategies to decrease or
eliminate allogenic transfusions
Identify strategies to manage anemia
6
BLOOD MANAGEMENT AT GSH
Started Early 2010
Identified 3 largest users of Blood Products
Focused on Orthopedics, ICU, and Oncology
Other areas were rising to the top in usage
by remaining static giving us our next area
to tackle
7
BASIC TENETS
Anemia is a treatable medical condition
Red cells should not be used to treat
anemias that can be corrected with
medications
(AABB, American Blood Centers, American Red Cross)
Always document reason for transfusion
Use one unit whenever possible
Recheck labs before ordering more blood
products
IDENTIFY AREAS NEEDING CHANGE
Know your data!
Target key problem areas first
Celebrate and congratulate all gains
Know your practices !
Data Dives…
Blood utilization by MSDRG
Physician practice
Premier benchmarking
…drive the focus
10
Top 10 MSDRGs by Blood Case Count for Discharges January 2009
to December 2009 - Inpatient
Blood Products
MS
DRG DRG Description
470
Major joint replacement or
reattachment of lower extremity w/o
MCC
765
Cases
No Blood Products
Avg
Chrgs
ALOS
Avg
ALOS Chrgs
Cases
Var Yes vs. No
Avg
Chrgs
ALOS
206
3
59,188
735
2 55,120
1
4,067
Cesarean section w CC/MCC
79
8
39,301
960
6
23,264
2
16,037
377
G.I. hemorrhage w MCC
77
5
34,336
23
4
21,902
1
12,434
378
G.I. hemorrhage w CC
Extreme immaturity or respiratory distress
syndrome, neonate
62
3
23,686
27
3
19,555
0
4,131
60
67
399,723
100
59
3
95,448
232
2
70,354
1
25,094
871
Spinal fusion except cervical w/o MCC
Septicemia or severe sepsis w/o MV 96+
hours w MCC
53
8
50,043
306
6
33,643
2
16,400
812
Red blood cell disorders w/o MCC
47
3
16,936
11
1 12,491
2
4,446
811
Red blood cell disorders w MCC
Major joint replacement or
reattachment of lower extremity w MCC
34
4
31,336
7
2 16,391
2
14,946
34
7
91,471
29
5 64,869
2
26,602
790
460
469
Hospital Average
23%
77%
28 152,825
39 246,898
37,106
11
Transfusion Practice at GSH by DRG
PEER Data
HOSPITAL (OH)) And (({Community Status} = Urban) And ({Council of Teaching Hospitals} = COTH) And ({Bed-Size} = Facilities w/ 501 Beds or More)) And ({Perspective
Clinical Summary} = BLOOD PRODUCTS)
Patient
Patient
Pat Pop Util
MGSH-Top 15 MSDRGS by Blood Product
Patient
Pop
Population
Rate
Cases
Populatio
Patient
Utilization
Utilization
Variance
MS-DRG
Blood Cases for Blood Cases
n for
Populatio
Rate for
Rate for
(FacilityFacility
for Peer
Facility
n for Peer
Facility
Peer
Peer)
Total
826
16,916
4,720
103,823
17.50%
16.29%
1.21%
MJR JNT RPLCMNT/RTTHMNT
470
197
3,052
908
22,973
21.70%
13.29%
8.41%
OF LWR ET W/OMCC
377
GI HEMORRHAGE WITH MCC
75
1,279
100
3,130
75.00%
40.86%
34.14%
765
812
460
790
378
871
469
811
945
774
481
329
742
CESAREAN SECTION WITH CC/MCC
RED BLOOD CELL DISORDERS
WITHOUT MCC
SPINAL FUSION EXCEPT CERVICAL
W/O MCC
EXT IMMATUR OR RESP DISTRESS
SYN NEONATE
G.I. HEMORRHAGE W CC
SEPTICEMIA/SEVR SEPSIS W/OMV
96+HRS WMCC
MAJ JOINT REPLACE/REATTACH
LOW EXT W MCC
RED BLOOD CELL DISORDERS
WITH MCC
REHABILITATION W CC/MCC
VAGINAL DELIVERY W
COMPLICATING DX
HIP & FEMUR PROC EXC MAJOR
JOINT W CC
MAJOR SMALL & LARGE BOWEL PX
W MCC
UTERINE&ADNEXA PX
NONMALIGNANCY WCC/MCC
68
596
1,005
13,618
6.77%
4.38%
2.39%
66
2,640
83
6,681
79.52%
39.52%
40.00%
62
518
286
6,041
21.68%
8.57%
13.10%
60
947
163
3,047
36.81%
31.08%
5.73%
54
1,977
80
5,538
67.50%
35.70%
31.80%
46
1,719
321
11,477
14.33%
14.98%
-0.65%
31
429
53
1,329
58.49%
32.28%
26.21%
31
964
41
2,095
75.61%
46.01%
29.60%
30
350
536
9,891
5.60%
3.54%
2.06%
29
158
867
8,908
3.34%
1.77%
1.57%
28
1,022
48
3,241
58.33%
31.53%
26.80%
25
900
57
2,976
43.86%
30.24%
13.62%
24
365
172
2,878
13.95%
12.68%
1.27%
Transfusion Practice by Top 10 MDs
Blood Products
Attend MD
Cases
ALOS
No Blood Products
Avg Chrgs
Cases
ALOS
Var Yes vs. No
Avg Chrgs
ALOS
Avg Chrgs
1
159
4
37,131
983
0
8,031
4
29,100
2
93
53
336,243
606
17
88,146
36
248,096
3
70
6
45,824
768
3
22,702
3
23,122
4
61
6
40,356
778
2
20,504
4
19,852
5
55
6
31,756
4769
1
5,970
5
25,787
6
53
7
121,419
435
1
24,366
6
97,052
7
43
3
25,601
680
0
8,116
3
17,485
8
43
8
64,414
278
3
26,218
5
38,196
9
40
4
91,258
211
0
17,306
4
73,953
10
40
3
60,370
481
2
45,024
1
15,346
ORTHOPEDICS
Hip Cases With Transfusions
120.00%
100.00%
80.00%
% Hip Cases
With
Transfusions
By Doctor
60.00%
40.00%
20.00%
0.00%
A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
Example of physician blinding for elective total hip arthroplasties
Orthopedics
Blinded physician-specific transfusion data
Presented at Section meeting
Extensive literature review for evidence based best
practice
New practice initiatives for pre, intra, and postoperative conservation
Amended order sets to reflect changes
Established Anemia Clinic
Orthopedic Center of Excellence (OCE)
Quality measure: Preoperative anemia
Established metrics
Posted on OCE dashboard
Orthopedic Recommendations
Document Reason for Transfusion:
HGB ≤7, HCT ≤ 21, Hypoxia, Weakness, or other signs of decreased
oxygen carrying capacity.
Reasons and Triggers for Autologous transfusion
same as allogenic.
While autologous transfusion is safer, it is not without risk
Limit autologous donations for indications such as
known antibodies on T&S, complex surgery, or
patient refusal of blood products.
Check HGB or HCT before automatically transfusing,
thereby documenting lab value, and reason for
transfusion
Do not give PRBCs in PACU without lab results.
Transfuse ONE unit at a time. Then recheck labs, reevaluate patient. Give second unit only if needed.
INTENSIVE CARE
Physician and Resident education
Newsletter
E- LEARN
Mandatory transfusion order set usage
Audited for compliance
Established ICU transfusion dashboards
Intensivist scorecards delivered quarterly
Transfusion order sets revised
Decreased H/H trigger to 7/21
Decreased number of PRBCs to 1
Increased INR trigger on FFP to 1.8 (from 1.5)
Oncology subset with decreased triggers
ONCOLOGY
General Oncology Meeting
OPCC, 14CD, CNS, and Physicians
Show them their practice and opportunity to improve
Task force to review best practice
Always give literature to support changes
Oncology Order sets revised
Decreased RBC trigger to HGB 7 or HCT 21
Decreased daily automatic transfusion to 1 unit RBC if
indicated by trigger (was 2 units)
Decreased Platelet trigger to 10,000 (from 20,000)
Strategies to Decrease or Eliminate
Transfusions
Pre-admission testing 14 – 45 days prior to
surgery – allowing time to treat anemia
Oral agents of Iron, Folic Acid and Vitamin C for
all patients
Avoid drugs that promote bleeding
Use Procrit - an erythropoesis stimulating
agent (ESA), and IV Iron for more severe anemia
Anemia is treated as a laboratory value, not a
diagnosis
Overlooked in the presurgical History and
Physical
Total Joint Replacement surgeries (TJA) on the
rise – especially in the elderly
TJAs have some of the highest rates of
transfusion
Preoperative anemia is the greatest predictor of
peri-operative transfusion !!!
Regional anesthesia
Hypotensive anesthesia for those requiring
general anesthesia
Pre-op Tranexamic acid
Decreased tourniquet time
Reinfusion system
Bipolar cautery
Avoidance of drains
Avoidance of strong VTE chemoprophylaxis in
low risk Total Knee Arthroplasy (TKA) patients.
Lovenox 40 mg daily in TKA.
INR targets near 1.5 for patients on Coumadin.
Prolonged knee flexion >70 degrees the day of
surgery
Transfusion triggers HGB 7 / HCT 21 unless
cardiac symptoms or unstable
IV fluid correction of hypotension and postural
changes
OUTCOMES IN ORTHOPEDICS
Since May 2011, overall transfusions of red blood cells have
decreased by over 50% to a rate of 2-6% in elective total
joint procedures
Transfusion rates during total hip replacements decreased
No adverse patient outcomes resulted
Decreased length of stay of 1 day on average
2011 PRBC Orthopedic purchase cost savings of $5,700 per
month average compared to 2010 average
Anemia Prevention
Anemia Clinic with automatic treatment of
patients by hematologist
Education of residents, and individual
services
Go to each section meeting and deliver the
message that is pertinent to their practice
Let other services know about the
successes gained by others
Empower staff nurses as your advocates
Pre-Surgical Anemia Protocol
Hospital Purchase Costs
RBC COSTS
$130,000.00
$120,000.00
$110,000.00
$100,000.00
$90,000.00
$80,000.00
$70,000.00
$60,000.00
$50,000.00
Elective Hip and Knee Arthroplasty RBC
% Transfused
20.00%
% Transfused
18.00%
16.00%
14.00%
12.00%
10.00%
8.00%
6.00%
4.00%
2.00%
0.00%
Linear (%
Transfused)
Oncology Data
Hgb > 7
Unknown
RBC Transfusion Triggers in Oncology (14CD & OPCC)
60
RBC UNITS TX
50
40
30
20
10
0
Hgb ≤ 7
Thank You
Katy Loos RN, MSN
Katy_Loos@trihealth.com
(CartCartoon source: http://bloodbankpartners.com)
References
Alexandrov, A. W., & Brewer, B. B. (2011). The Role of Outcomes in Evaluating Practice
Change. In B. M. Melnyk, & E. Fineout-Overholt, Evidence Based Practice in Nursing and
Healthcare . Philadelphia: Wolters Kluwer/ Lippencott Williams & Wilkins.
American Society of Anesthesiologists, Inc. (2006). Practice guidelines for perioperative
blood transfusion and adjuvant therapies. Anesthesiology, 198 - 208.
Farris, P., Ritter, M., & Abels, R. (1996). The Effects of Recombinant Human Erythropoietin
on Perioperative Transfusion Requirements in Patients Having a Major Orthopedic
Operation. The Journal of Bone and Joint Surgery, 62 - 72.
Goodnough, L. T., Maniatis, A., Earnshaw, P., Benon, G., P. B., Bisbe, E., et al. (2011).
Detection, evaluation, and management of preoperative anemia in the elective orthopedic
patient: NATA guidelines. British Journal of Anaesthesia, 13 - 22.
References, cont.
Kumar, A. (2009, November). Perioperative management of anemia: Limits of blood
transfusion and alternatives to it. Cleveland Clinic Journal of Medicine, pp. S112 - S118.
Liumbruno, G., Bennardello, F., Lattanzio, A., Piccoli, P., & Rossetti, G. (2011).
Recommendations for the transfusion management of patients in the peri-operative
period. III. The post-operative period. Blood Transfusion, 320 - 335.
Martinez, V., Monsaingeon-Lion, A., Cherif, K., Judet, T., Chauvin, M., & Fletcher, D. (2007).
Transfusion strategy for primary knee and hip arthroplasty: Impact of an algorithm to lower
transfusion rates and hospital costs. British Journal of Anesthesia, 794 - 800.
Spahn, D. (2010, August). Anemia and patient blood management in hip and knee surgery:
A systematic review of the literature. Anesthesiology, pp. 482 - 495.
www.cynosurehealth.org
Upcoming Webinars
• August 9th 11:00am-noon PST
• September 13th 11:00am-noon PST
Thanks for joining us today