Depo-ProveraClinicalUpdateforDSHS610
advertisement
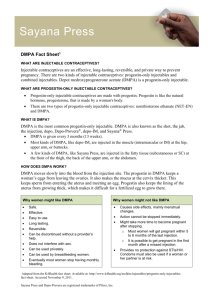
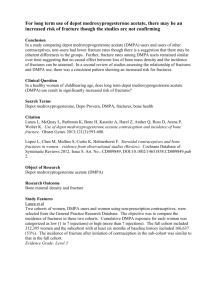
Depo-Medroxyprogesterone Acetate Clinical Update Scott J Spear, MD Medical Director Planned Parenthood of the Texas Capital Region & Planned Parenthood of Central Texas Clinical Assistant Professor of Obstetrics & Gynecology UT Southwestern Medical Center Learning Objectives • Provide background and description of DMPA • List mechanism of action, efficacy, advantages, and disadvantages of DMPA • Describe examples of good candidates for DMPA use • Discuss DPMA Black Box Warning • Discuss research on DMPA and it’s impact on BMD and skeletal health more… Learning Objectives (continued) • Critically examine recommendation for “addback” estrogen or DEXA scans for minors • Present ACOG’s and WHO’s Guidance on DMPA DMPA: Background • Since introduction in 1963, used safely in >30 million women worldwide • >2 million US women currently use DMPA • Temporary bone loss ACOG Committee Opinion No. 415. Obstet Gynecol. 2008. Description of DMPA • Depot Medroxyprogesterone Acetate (DMPA) • Brand names: DepoProvera® and Depo-subQ provera 104™ • Intramuscular or subcutaneous injection every 3 months Goldberg AB. Contraceptive Technology. 2007; Mechanism of Action: DMPA Prevents Ovulation Goldberg AB. Contraceptive Technology. 2007. Reduces production of estradiol Candidates for DMPA • Women who want reversible, non-daily contraception ▪ The percentage of teens who use DMPA increased from 10% in 1995 to 21% in 2002 • Women in whom estrogen is contraindicated • Women who experience menorrhagia, dysmenorrhea, and iron deficiency anemia • Women who don’t wish to conceive immediately after discontinuing this method Cromer BA. Am J Obstet Gynecol. 2005.; Westhoff C. Contraception. 2003.; Trussell J. Contraceptive Technology. 2007. DMPA: Failure Rate Perfect Use Typical Use 0.3% 3% Westhoff C. Contraception. 2003.; Cromer BA. Am J Obstet Gynecol. 2005. Risks and Side Effects of DMPA Weight Gain Menstrual cycle changes Nelson AL. J Reprod Med. 1996.; Kaunitz AM, Contraception. 2008. BMD Loss Advantages of DMPA Convenient, discrete, very effective, reversible May improve menorrhagia, dysmenorrhea, iron deficiency anemia, and endometriosis Women with contraindications to estrogen can use it Reduces the risk of endometrial cancer Reduces risk of PID and uterine leiomyomata Can decrease the number and severity of crises in patients who have sickle cell anemia Can decrease frequency of seizures Thomas DB. Contraception. 1995.; Gray PH. Br J Obstet Gynecol. 1996.; Lumbiganon P J Reprod Med. 1996; Culling VE. J Reprod Med. 1996.; Mattson RH Neurology. 1984. Disadvantages of DMPA Requires visit to clinician Initial irregular bleeding Weight gain Short-term, reversible BMD loss Delayed return to fertility Lack of protection against STIs Westhoff C. Contraception. 2003.; Risser WL. Adolesc Health. 2003. Le YL. Obstet Gynecol. 2009.; Kaunitz AM, Contraception. 2008. Contraindications • History of or current breast cancer • Anorexia nervosa • Chronic steroid use WHO. 2004 DPMA Black Box Warning “It is unknown if use of DMPA Contraceptive Injections during adolescence or early adulthood, a critical period of bone accretion, will reduce peak bone mass and increase the risk for osteoporotic fracture in later life. FDA Safety Alert. 2009.; Liang BA J Clin Anesth. 2002. DPMA Black Box Warning Prolonged use may result in significant loss of bone density Degree of loss is proportional to the amount of time on DMPA Loss may not be completely reversible more… FDA Safety Alert. 2009 DPMA Black Box Warning (continued) Woman should use DepoProvera for more than two years only if other contraceptive methods are inadequate FDA Safety Alert. 2009 What the Best Science Indicates • BMD loss associated with DMPA is similar to that associated with pregnancy and breastfeeding • BMD loss is substantially reversed after stopping use of DMPA • Environmental factors, such as nutrition and exercise, have a more substantial impact on bone mass than DMPA Kaunitz AM. Contraception. 2008. What we know about DMPA and it’s impact on BMD and skeletal health DMPA users are likely to have a reduced BMD Suppressed estradiol production is associated with an increased rate of bone resorption Short-term diminishment of BMD recovers within three years once DMPA is discontinued DMPA use not linked to the development of menopausal osteoporotic fractures Cundy T. BMJ. 1991.; Kaunitz AM. Obstet Gynecol Clin North Am. 2000.; Kaunitz AM. Contraception. 2008.; Banks E. BJOG. 2001.; Westhoff CL. Contraception. 2003.; et al. More Research on DMPA and It’s Impact on BMD • Former users of DMPA had BMD similar to nonusers • Adolescents demonstrated a full recovery of BMD within one year after discontinuation of DMPA Pettiti DB. Obstet Gynecol. 2000.; Scholes D. Arch Pediatr Adolesc Med. 2005. “Add-back” Estrogen or DEXA scans for Minors Research indicates • Estradiol levels mediate BMD changes in adult and adolescent DMPA users • “Add-back” estrogen prevents the transient decline in the BMD of current DMPA users • BMD recovers after DMPA is discontinued • Unlikely that women would benefit from estrogen supplementation or serial surveillance by DEXA scans more… Cundy T. J Clin Endocrinol Metab. 2003.; Kaunitz AM. Contraception. 1999. “Add-back” Estrogen or DEXA scans for Minors (continued) • In adolescents, daily intake of 1500 mg of calcium and 400 mg of vitamin D is recommended Guidance on DMPA Usage and Skeletal Health Position statements have been issued by several professional organizations—ACOG & WHO These organizations recommend no restrictions on initiation or continuation of DMPA to address skeletal health concerns These organizations recommend no routine BMD testing for DMPA users Kaunitz AM. Contraception. 2008. DMPA: ACOG Guidelines “Concerns regarding the effect of DMPA on BMD should neither prevent practitioners from prescribing DMPA nor limit its use to 2 consecutive years.” No need to perform BMD monitoring solely in response to DMPA use. more… ACOG Committee Opinion No. 415. Obstet Gynecol. 2008; AAP Policy Statement. Pediatrics. 2007. DMPA: ACOG Guidelines (continued) ACOG recommends: • Counsel thoroughly about benefits and risks of DMPA • Encourage daily exercise and ageappropriate calcium and vitamin D intake • Estrogen supplementation during DMPA use is not currently recommended ACOG Committee Opinion No. 415. Obstet Gynecol. 2008; AAP Policy Statement. Pediatrics. 2007. DMPA: WHO Guidelines • No restriction on DMPA in eligible women 18-45 yrs of age • Among adolescents and women >45 yrs of age, advantages of DMPA generally outweigh theoretical safety concerns re: fracture risk • No restrictions on progestin-only or combined hormonal contraception in eligible women D’Arcangues C. Contraception. 2006. Counseling Messages for DMPA • Women for whom estrogen products are contraindicated can use DMPA • Bleeding profile improves over time • Non-hormonal backup contraception is needed for first 7 days What Providers Need to Know • No mandate for serial BMD testing or “addback” estrogen supplementation • No need to discontinue DPMA after two years of use • Supplemental use of menopausal doses of estrogen can be considered for women with additional risk factors for low BMD • Women should consume appropriate amounts of calcium and vitamin D. more… FDA Safety Alert. 2009 What Providers Need to Know (continued) • Concerns about temporary bone loss should be weighed against DMPA’s convenience and efficacy • Patients should engage in weight-bearing exercise to promote bone health • Risks associated with DMPA along with genetic and lifestyle factors should be examined DiVasta AD. Adolesc Med. 2006. The DMPA picture is generally rosy: