Orientation Infection Control
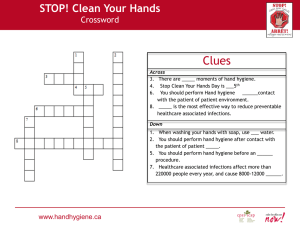
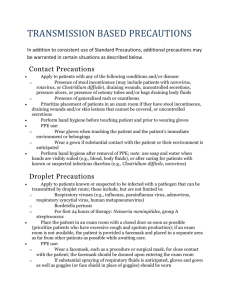
advertisement

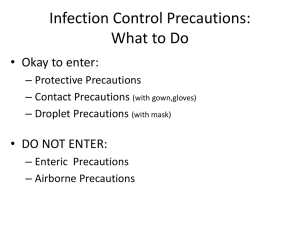
New Employee Orientation Infection Prevention and Control Topics Hand Hygiene Standard Precautions Transmission-Based Precautions Personal Protective Equipment (PPE) Multiple Drug Resistant Organisms (MDRO) Bloodborne Pathogens Aerosol Transmissible Diseases (ATD) Exposure Control Plan Infection Prevention and Control Team Physician Champion Dr. Marc J. La Riviere, Infectious Disease Infection Preventionists Theresa Caughlin, RN, BS, CIC, Director Leslie Budrick, RN, CIC Hala Nashed, M.B.B.Ch, MPH, CIC Reddy Munagala, Ph. D., CIC Leonard De la Cruz, RN, BSN, MPH, CIC, CPHQ Sharron Martinez, Project Manager Office: (323) 783-8398 24 hr Pager (323) 279-0610 Coverage Los Angeles Medical Center Medical Office Buildings (MOBs) East Los Angeles Glendale Glendale Orange Pasadena Mental Health Center PURPOSE OF THE INFECTION PREVENTION AND CONTROL PROGRAM • Improve patient safety via PREVENTION, IDENTIFICATION, and CONTROL of infections & communicable diseases • Prevent hospital acquired infections • Minimize occupational health risk to healthcare workers Starting with the basics…… HAND HYGIENE: Key to Preventing Infection WHAT? A general term that applies to either handwashing, antiseptic handwash/handrub, or surgical hand antisepsis WHEN? Before and after ALL patient interactions; before using and after removing gloves HOW? Rub hands vigorously for 15 seconds WHICH? Soap and water or alcohol-based hand gel if hands are not visibly soiled WHO? All healthcare providers, patients, family EVERY PATIENT - EVERY TIME STOP the bugs! Clean hands = patient safety Culture of a hand before disinfection Culture of a hand after disinfection Photos by John M. Boyce, M.D. WHAT CAN YOU DO? Remember the 5 moments of hand hygiene Commitment to 15 second hand wash or routine use of alcohol-based hand rub Gloves: Not a substitute for Hand Hygiene STANDARD PRECAUTIONS Previously called Universal Precautions Assumes blood and body fluid of ANY patient could be infectious Includes Respiratory Hygiene/Cough Etiquette Hand hygiene Every patient – every time Respiratory Hygiene/Cough Etiquette • Component of Standard Precautions • Prevent transmission of all respiratory infections • Targeted for all individuals with signs of respiratory illness including cough, congestion, rhinorrhea, or increased production of respiratory secretions when entering a healthcare facility Elements of Respiratory Hygiene/Cough Etiquette Education of staff, patients, and visitors Visual alerts/posted signs Source control measures Hand hygiene after contact with respiratory secretions Spatial separation STANDARD PRECAUTIONS FOR EVERY PATIENT CONTACT EVERY TIME IF IT’S WET AND NOT YOURS…DO NOT TOUCH IT DO NOT LET IT TOUCH YOU WITHOUT PPE Personal Protective Equipment (PPE) WHAT? A variety of barriers and respirators used to protect from contact with infectious agents WHY? To protect susceptible patients from inadvertent colonization and subsequent development of health care associated infections (HAI) WHEN? As part of standard precautions and transmission-based precautions depending on anticipated exposure WHO? All healthcare providers PPE GLOVES MASK GOWNS GOGGLES Transmission-based Precautions Contact Precautions • For infections spread by direct or indirect contact with patients or patient-care environment (e.g. MRSA, VRE, ESBL) • PPE • Hand hygiene • Educate patient and family and document in Health Connect Contact Plus Precautions • Use Contact Plus Precautions for confirmed or suspected cases of C. difficile, Norovirus, unexplained/infectious diarrhea • Use soap and water to wash hands for 15 seconds after all patient care • Use bleach wipes for routine cleaning of patient equipment and high touch surfaces Droplet Precautions • For infections spread by large droplets generated by coughs, sneezes (e.g. Neisseria meningitis, pertussis, seasonal influenza, MRSA pneumonia) • Use surgical mask (not N-95) • Patient should wear a surgical mask outside of the patient room • Negative pressure room is not needed • Educate patient and family and document in Health Connect Airborne Precautions • • • • • For infections spread by particles that remain suspended in the air (TB, measles, varicella, disseminated herpes zoster) Negative pressure room N-95 mask for personnel inside negative pressure room Patient should wear surgical mask outside of the room Educate patient and family and document in Health Connect It is your responsibility… • To know where to locate PPE in your department • To don PPE when appropriate • To do hand hygiene as the final step after removing and disposing PPE Multi-drug resistant organisms (MDROs) • Organisms that have developed resistance to antimicrobial drugs • Growing threat to public health Examples of MDRO • Methicillin Resistant Staphylococcus Aureus (MRSA) • Vancomycin Resistant Enterococcus (VRE) • Extended spectrum beta lactamase (ESBL) i.e. Klebsiella, E. Coli • Multi-drug resistant Acinetobacter Modes of transmission of MDROs • • • • Unwashed hands Gloves worn from patient to patient Contaminated environmental surfaces Inadequately cleaned and disinfected equipment • Inadequate, inappropriate or prolonged use of antibiotic agents Preventing Transmission of MDRO’s • Hand hygiene is the BEST way to prevent transmission • Use of Contact precautions: gloves and gowns; dedicated equipment and supplies • Proper cleaning and disinfection of the room • Education of staff and patients • Prompt identification, treatment and notification • Antimicrobial stewardship Bloodborne Pathogens (BBP) Hepatitis B virus (HBV) Hepatitis C virus (HCV) Human immunodeficiency virus (HIV) Bloodborne Pathogen 3 Modes of BBP transmission 1. Needle sticks and punctures 2. Splashes to the eyes or mucous membranes 3. Cuts or non-intact skin BBP Exposure Control Plan • • • • • Standard Precautions Hep B vaccine at no cost Hand Hygiene Safer Sharp devices Biohazardous labeling In case of exposure… • • • • Wash area Notify supervisor immediately Fill out appropriate forms See a health care professional within 1-2 hours of exposure BBP BBP Awareness Training in KP Learn http://learn.kp.org/ No Food or Drinks at the Nursing Station The OSHA Bloodborne Pathogen Standard prohibits food and drink in areas where contamination is likely. “This regulation prohibits the consumption of food and drink in areas in which work involving exposure or potential exposure to blood or other potentially infectious material exists, or where the potential for contamination of work surfaces exists. The prohibition against eating and drinking in such work area is consistent with other OSHA standards and is good industrial hygiene practice” Aerosol Transmissible Diseases (ATD) • ATD Exposure Control Plan • Exposure Prevention and Hierarchy of Controls • TB Surveillance/Screening • Fit testing ATD Exposure Control Plan • Cal OSHA ATD Standard • Preventing the transmission of various ATD including Tuberculosis • Collaboration with Employee Health Services (EHS) and Environmental Health and Safety (EH&S) in the implementation and management of program ATD Exposure Prevention • Prompt identification of suspect and confirmed ATD cases • Respiratory etiquette practices • Patients wearing surgical mask during transport or in waiting rooms • PPE during provision of care • Use of airborne infection isolation rooms (AIIR) for suspect or confirmed cases TB Surveillance and Screening • TB screening: new hire and annually • Fit testing • Exposure Control and Follow-up Tuberculosis (TB) • Is infectious and potentially life-threatening • Can involve any body organ or tissue, not just lungs • Contagious. Spread through coughing, sneezing, singing, talking loudly • Reportable to Department of Health and Human Services • Must have care plan approved by Department of Health prior to discharge from the hospital. Contact your Case Manager/Discharge Planner Infection Prevention It’s everyone’s business Thank you