Practical Peds Cardi..
advertisement

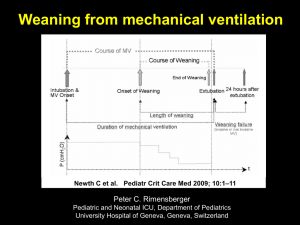
Practical Pediatric Cardiac Anesthesia Michael S. Mazurek, MD Overview Preoperative Workup Pathophysiology Induction Pre-pump considerations On-pump considerations Post-pump considerations ?Extubation Preoperative Workup Heart Center 4th floor Medicines Previous surgeries Heart failure, arrythmias Sternotomy, BT shunt Recent echocardiogram Pathophysiology, ventricular function Preoperative Workup Labs CXR Cardiomegaly, pulmonary congestion Physical exam Electrolytes, CBC, Coags Failing to thrive, tachypneic, pulses, perfusion, rales, hepatomegaly Consent Caudal morphine Intubated, sedated in ICU Preoperative Workup Orders NPO same as usual Preop versed same as usual Inotrope drip sheet order Dopamine, dobutamine, epinephrine, nitroglycerine usually (discuss with staff) Send to pharmacy night before Give to nurses in heart center Fax it to the pharmacy yourself Pathophysiology Understand the patient’s lesion (recent echo most helpful) Cyanotic or acyanotic lesion (RA sats) Ventricular function good or poor Obstructive lesion? Are there oxygenation and ventilation issues? Are there line placement issues? Postop pulmonary hypertension? Room Setup Normal setup plus: Phenyephrine 100mics/cc Epinephrine 10mics/cc Have inotrope drips in the room 2 or 3 IVs and A-line Add several stopcocks to D5LR line Hot line Need blood available Bair hugger (for post-pump use) Cerebral oximeter Induction IV induction or inhalation induction Again, know the pathophysiology If ventricular function poor or LVOT obstructive lesion (critical AS), lean towards gentle IV induction (ketamine, narcotic, etomidate) If ventricular function good, inhalation induction most likely well tolerated Induction Again consider oxygenation/ventilation issues Again consider line placement issues Caudal morphine 70-100mics/kg if plan on early extubation Cefuroxime 25mg/kg if not allergic Anesthesia Maintenance Narcotic based Remifentanil infusion Fentanyl bolus < 10mic/kg if plan on extubation 50 – 100mic/kg as sole anesthetic for many neonatal pumps Volatile anesthetic titration Ketamine Muscle relaxant (usually cisatra infusion) Intermittent midazolam Pre-Pump Considerations Aprotinin? (Surgeon’s decision) Dr. Brown Dr. Turrentine 2.5 + 2.5 + 2.5cc/kg Heparin 400Units/kg given in RA 3.5cc/kg IV shortly before cannulation (wait until pursestring sutures in) 3.5cc/kg in pump per perfusionist ACT 2mins after Midazolam dose pre-cannulation Pre-Pump Considerations Cannulation Aortic line first (trendelenburg position) Look for bubbles IVC and SVC cannulation Valsalva 10-20 cm/H20 until pursestrings cinched Potential for blood loss – watch field and ABP and have perfusionist give volume through aortic line if necessary On-Pump Considerations IVFs to keep open Turn off humidifier Monitor mean ABP Monitor urine output Get inotropes ready for post-pump Dopamine, nitroglycerine On-Pump Considerations Nitroglycerine 0.25mcg/kg/min Dr. Turrentine for whole case Helps with rewarming Dopamine 5mcg/kg/min ready to go Call for echo and blood products 20 minutes before coming off pump Repeat midazolam with rewarming Set up RA, LA, PA lines On-Pump Considerations Start ventilating when patient starts ejecting One of venous canulas out Decompression line out Re-expand lungs with large breath and hold Off-Pump Considerations Weaning off pump Full ventilation 100% O2 Bair hugger full warm Hypotension? What does echo show – volume and function Hct, calcium Consider small dose epi or phenylephrine Consider inotropes Modified Ultrafiltration (MUF) Off-Pump Considerations Protamine after MUF Half dose at a time Hypotension and pulmonary hypertension side effects ACT and ABG 5 minutes after protamine Start blood products if coagulopathy Platelets first, then cryo Rarely need FFP Off-Pump Considerations Coagulopathy Risk < 8 kg Cyanotic lesions Long pump run Redo sternotomy Residual hypothermia Keep calcium > 1.0 (20mg/kg/dose CaGluc) NaHCO3 for metabolic acidosis: mEq dose= base deficit x wt. x 0.3 Extubation Extubation criteria (case by case basis) Non-neonate Stable hemodynamics Stable coagulopathy Caudal helpful, not mandatory Reasonable PaO2 on 40-50% O2 Transport to ICU Emergency supplies (laryngoscope, ETT, drugs, etc.) Oxygen (Jackson-Rees circuit or Ambu) Discuss case with ICU resident and nurses Return monitor and oxygen to workroom Case Example 5 year old boy who is otherwise healthy for repair of a secundum ASD. 5 year old ASD Preoperative workup What’s important Pathophysiology Induction Anesthesia maintenance Aprotinin? Coagulopathy? Extubation? Case Example 3 day old with hypoplastic left heart syndrome for Norwood procedure. 3 day old Norwood Preoperative workup Pathophysiology Induction Anesthesia maintenance Aprotinin? Coagulopathy? Extubation?