Stroke
advertisement

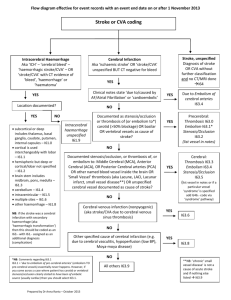
Stroke Chih-Ping Chung, MD PHD Department of Neurology, Taipei Veterans General Hospital National Yang Ming University 腦中風 : 定義 • 腦中風 : 快速發展之腦部功能局部或全面障礙, 症狀持 續 24 小時以上,或造成死亡. 除了血管病變外, 無其他明顯原因. • 種類: – 阻塞性 (ischemic stroke) – 出血性 (hemorrhagic stroke) CI: cerebral infarction ICH: intracerebral hemorrhage Ischemic Stroke • • • • • Cerebral vessel anatomy and collaterals Ischemic stroke classification (etiology-based) Cerebral microvessel Brain tissue ischemia Management: increased cerebral blood flow (CBF) Major Arteries supplying Brain: Anterior Circulation vs. Posterior Circulation Anterior Circulation Collateral circulation Circle of Willis Extracranial arterial collateral circulation • facial (a), maxillary (b), and middle meningeal (c) arteries to the ophthalmic artery • dural arteriolar anastomoses from the middle meningeal artery (d) and occipital artery through the mastoid foramen (e) and parietal foramen (f) Intracranial arterial collateral circulation • leptomeningeal anastomoses between anterior and middle cerebral arteries (b) and between posterior and middle cerebral arteries (c) Ischemic Stroke • • • • • Cerebral vessel anatomy and collaterals Ischemic stroke classification (etiology-based) Cerebral microvessel Brain tissue ischemia Management: increased cerebral blood flow (CBF) Etiologies of ischemic stroke • • • • Large artery atherothromboembolism Cardioembolism Small vessel occlusion (Lacunar infarction) Others Atherosclerosis Etiologies of ischemic stroke • • • • Large artery atherothromboembolism Cardioembolism Small vessel occlusion (Lacunar infarction) Others High risk source of cardiogenic emboli History Cardiovascular evaluation • Mechanical prosthetic heart valve • Af • Sick sinus syndrome • MI within 4 weeks • Dilated cardiomyopathy • Atrial myxoma • Infective endocarditis • Akinetic left ventricular segment • Left ventricular thrombus • Echo: dilated cardiomyopathy, atrial myxoma, infective endocarditis, akinetic left ventricular segment, left atrial thrombus, left ventricular thrombus • ECG: Af demonstrated at any time during hospitalization, AMI • Holter monitor: Af demonstrated at any time during hospitalization, sick sinus syndrome Etiologies of ischemic stroke • • • • Large artery atherothromboembolism Cardioembolism Small vessel occlusion (Lacunar infarction) Others Small vessel disease • 1965, CM Fisher – clinicopathological studies of lacune (Fisher 1969, 1977, 1978, 1979, Fisher and Caplan 1971, Fisher and Tapia 1987) • He coined the term “lacune”: specific pathological and radiological presentations Small vessel disease • Subcortical small infarction • Long penetrating arterioles: from the pial network located on the surface of the brain Perforating arteries Perforating arteries Small vessel disease: lacune Fisher’s theory: from the observations of parenchyma and vessel pathology Lipohyalinosis & microatheroma Microemboli Ischemic Stroke • • • • • Cerebral vessel anatomy and collaterals Ischemic stroke classification (etiology-based) Cerebral microvessel Brain tissue ischemia Management: increased cerebral blood flow (CBF) Microvessels Blood-brain barrier • Arteriole: An arteriole is a small diameter blood vessel that extends and branches out from an artery and leads to capillary. Thin muscular walls (usually only one to two layers of smooth muscle) and are the primary site of vascular resistance. • Capillary: 5 – 10 um; composed of only a single layer of cell, the endothelium. • Venule: A little vein. Venules go from capillaries to veins. Thin muscular walls Capillary • Enable the interchange of water, oxygen, carbon dioxide, and many other nutrient and waste chemical substances between blood and surrounding tissues. • Perfusion pressure: the net pressure gradient causing blood flow to the brain. It must be maintained within narrow limits because too little pressure could cause brain tissue to become ischemic (having inadequate blood flow), and too much could raise intracranial pressure (ICP) or/and BBB damage and vasogenic edema. • CPP = MAP − ICP (if ICP is higher than JVP) Or CPP = MAP − JVP (if JVP is higher than ICP). • Cerebral blood flow (CBF) is driven by cerebral perfusion pressure (CPP) Microangiopathy • Ischemia (perfusion pressure) • Increased vascular permeability: BBB damage – vasogenic edema – IICP/hemorrhage Arteriole: Cerebral autoregulation • CBF is regulated by a complex system influenced by multiple factors: CPP, brain metabolic activity, autonomic innervation, vasodilators (CO2, NO), and drugs (acetazolamide) • CA: The CBF is kept relatively constant within a wide range of the CPP. • Endothelium and smooth muscle CPP = ABP – ICP (JVP) Cerebral autoregulation is maintained by different hypothesized control pathways • Vasogenic • Metabolic Vasogenic mechanism Intrinsic ability of cerebral vessels to responses to changes in transmural pressure. Stroke 2003;34:1645-1649 Stroke 1994;25:793-797 Stroke 1995;26:1014-1019 Vasogenic mechanism Animal study • Intraluminal pressure: controlled by smooth muscle, modulated by endothelium (intracellular signals – Ca2+ influx) • Flow: controlled by endothelium, mediated by NO These counteracting mechanisms assure optimal adjustment of the vessel diameter to CPP at any time. Circ Res 1995;77:832-840 1990;66:1445-1448 Nuclear Medicine Review 2007;10:29-42 Circ Res Stroke 1998;29:1194-1200 Metabolic regulation • Arteriolar resistance is modified by waste products of energy metabolism (CO2), partial pressure of O2, and release of specific vasoactive substances such as adenosine and potassium ions from neurons in response to insufficient blood supply. Stroke 1977;8:358-360 2002;33:844-849 Stroke Cerebral microvascular pathology HTN Aging • Hyaline arteriosclerosis • Lipohyalinosis • Atherosclerosis Obstruction Impaired autoregulation function BBB damage Cerebral hypoperfusion (acute ischemia and chronic ischemia) in aging/HTN subjects Vasogenic edema, microbleeding Cerebral small vessel disease 1. Lacunar infarction Cerebral small vessel disease 2. Leukoaraiosis (age-related white matter changes) Leukoaraiosis • Risk factors: aging and HTN • Chronic cerebral hypoperfusion (decreased CBF globally) • BBB Vessel pathology in LA: fibrosis • Hyaline arteriosclerosis: Degeneration of the media associated with depositions of collagens type I, III, IV, V, as well as other components of extracellular matrix in media and adventitia; increased amounts of basal lamina components • Pericapillary sclerosis: the proliferation of collagen fibrils in the media and adventitia of the blood vessels is not specific to small arteries and arterioles but also occurred in the pericapillary spaces • Capillary and arteriolar loss • Venous collagenosis Ischemic Stroke • • • • • Cerebral vessel anatomy and collaterals Ischemic stroke classification (etiology-based) Cerebral microvessel Brain tissue ischemia Management: increased cerebral blood flow (CBF) Brain tissue ischemia Ischemic Stroke • • • • • Cerebral vessel anatomy and collaterals Ischemic stroke classification (etiology-based) Cerebral microvessel Brain tissue ischemia Management: increased cerebral blood flow (CBF) Management Cerebral arterial stenosis/occlusion LAA/CE/SVD/others • Improved CBF • Neuroprotection Decreased CBF Cerebral autoregulation (endothelial function etc) Brain tissue ischemia Neuroprotection Management: improved CBF Cerebral arterial stenosis/occlusion LAA/CE/SVD/others Decreased CBF Cerebral autoregulation (endothelial function etc) Brain tissue ischemia • Prevention: endarterectomy, stenting • Acute management: thrombolytics – medical and mechanical • Targeting endothelial cell functions (ACEI, calcium blocker, statins, etc.) Take home messages • Ischemic stroke is a heterogeneous disease • Cerebral microvessel: specific structures and functions • How to improve CBF