after
advertisement

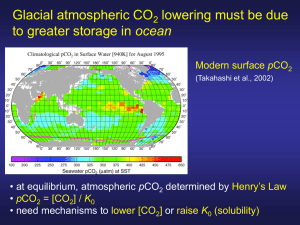
SOLUBLE FIBRIN MONKEY (E. COLI INJECTION) HUMAN (ACUTE LEUKEMIA) CAUSES OF DIC • Blood exposed to excess tissue factor Endothelial damage Tissue factor expression by monocytes Massive tissue/organ injury Cancer Obstetric catastrophe • • Activation of fibrinolysis Secondary to thrombin formation (t-PA) Cancer/leukemia (t-PA, u-PA, other) Cardiopulmonary bypass Other procoagulant or profibrinolytic substances Cancer cells Venoms TFPI TFPI AT3 APC AT3 APC TFPI F. VIII/F. IX F. VII Tissue factor AT3 APC Thrombin PL, Ca++ TFPI APC F. II F. X/F. V AT3 AT3 TFPI APC APC AT3 TFPI Thrombin F. VIII/F. IX F. VII Tissue factor Thrombin PL, Ca++ F. II F. X/F. V Thrombin TISSUE FACTOR • Ubiquitous lipoprotein • Highest concentrations in mucosa, brain, skin, • • vascular adventitia "hemostatic envelope" Not normally expressed by endothelium or circulating cells Expression induced by inflammatory cytokines Major physiologic (and pathologic) initiator of coagulation TISSUE FACTOR Am J Pathol 1989; 134:1087-97 LARGE VESSEL SMALL VESSEL MONOCYTE + MONOCYTE ENDOTOXIN CYTOKINE-INDUCED GAPS IN ENDOTHELIAL MONOLAYER J Exp Med 1989;169:1977-91 Control 5 nM TNF x 90 min 5 nM TNF x 24h KINETICS OF MONOCYTE TISSUE FACTOR mRNA EXPRESSION AND THROMBIN GENERATION AFTER ADMINISTRATION OF BACTERIAL LIPOPOLYSACCHARIDE TO HEALTHY VOLUNTEERS Tissue factor mRNA Franco et al, Blood 2000;96:554-9 Thrombin Cancer cells shed procoagulant membrane vesicles Fibrin deposits around tumor cells Intravascular fibrin Dvorak et al, 1981 SECRETED PRODUCTS OF MYELOBLASTS Urokinase Tissue factor Elastase tPA Cytokines PROMOTERS OF DIC • Inflammation (TNF, IL-1, IL-6, etc) Upregulation of procoagulant pathways Downregulation of profibrinolytic pathways Effects on endothelium • Liver disease Inhibitor deficiency (antithrombin, antiplasmin, protein C, etc) Diminished clotting factor production Delayed clearance of FDP INFLAMMATORY CYTOKINES TNF monocyte IL-1 endothelial cell Tissue factor Decreased expression Thrombomodulin IL-3/IL-6 liver megakaryocyte Increased Increased Increased PAI-1 Fibrinogen, Platelets antiplasmin Fibrin deposition in kidney in DIC induced by tissue factor (TF) or bacterial lipopolysaccharide (LPS) in rats Asakura et al, Crit Care Med 2002;30:161 RELATIONSHIP BETWEEN MORTALITY AND TNF LEVEL IN CHILDREN WITH INFECTIOUS PURPURA FULMINANS 100 Mortality (%) 80 Under 0.15 0.15-0.50 60 0.50-1.00 40 Over 1.00 20 0 TNF level (ng/ml) NEJM 1988;319:397-400 COMPLICATIONS OF DIC •Bleeding •Thrombosis •Tissue necrosis CAUSES OF BLEEDING IN DIC • Clotting factor consumption • High levels of FDP (inhibit fibrin formation) • Endothelial damage • Increased fibrinolytic activity FIBRINOLYSIS Platelets Endothelial cell PAI-1 Plasminogen Fibroblasts TPA UK Macrophage Liver Fibrin 2 PI Plasmin FDP 2 PI Fibrinogen Bleeding severity vs antiplasmin activity patients with platelets > 30,000 100 % of patients 80 0-2+ bleeding 60 3-4+ bleeding 40 20 0 < 50% 50-75% Antiplasmin activity > 75% DIC WITH HYPERFIBRINOLYSIS Examples • Acute leukemia (particularly promyelocytic) • Metastatic cancer (esp. prostate) • Cardiopulmonary bypass • Liver disease or transplantation THROMBOSIS IN DIC • Large vessel thrombosis uncommon • • Disordered clotting Increased fibrinolysis More common in "chronic DIC" e.g., Trousseau syndrome Clots may form around intravascular catheters, etc TISSUE NECROSIS AND DIC (PURPURA FULMINANS) Contributing factors • Intravascular fibrin • Endothelial damage • Downregulated fibrinolysis • Hypotension • Pressor administration • Acquired protein C deficiency PUPURA FULMINANS Pneumococcal sepsis in splenectomized patient High level bacteremia NEJM 2001;344:1593 NEJM 2004;351:2636 PURPURA FULMINANS IN MENINGOCOCCEMIA High level bacteremia Blood 2005;105:11 NEJM 2001;344:1372 TISSUE NECROSIS IN PURPURA FULMINANS ADRENAL GLAND (Waterhouse-Friderichsen syndrome) NEJM 2005;353:1245 RENAL CORTEX Hum Pathol 1972;3:327 PROTEIN C • Physiologic anticoagulant • • Vitamin K-dependent Destroys factors Va, VIIIa (Protein S is cofactor) Activated by thrombin bound to endothelium Activation downregulated by inflammatory cytokines Protective effect on endothelium? Protein C receptor on endothelial cells Activated protein C modulates endothelial response to inflammation and hypoxia Severe deficiency of protein C can cause tissue necrosis THE PROTEIN C SYSTEM Blood 2007; 109:3161 CYTOPROTECTION BY APC Blood 2007; 109:3161 PROTEIN C OR S DEFICIENCY STATES ASSOCIATED WITH THROMBOSIS OR PURPURA FULMINANS Situation Mechanism Clinical Manifestations Inherited protein C or S deficiency (homozygous) Genetic Neonatal purpura fulminans Inherited protein C or S deficiency (heterozygous) Genetic Increased risk of venous thromboembolism Genetic + decreased protein C synthesis Warfarin-induced skin necrosis ? Immune-mediated protein S consumption ? Protein C and S consumption (DIC) or downregulation ? Monoclonal Ig binds protein C or APC Post-infectious purpura fulminans Heterozygous protein C (or S?) deficiency + warfarin Rx Varicella infection Meningococcemia Acquired protein C inhibitor Meningococcal purpura Purpura fulminans HOMOZYGOUS PROTEIN C DEFICIENCY WITH NEONATAL PURPURA FULMINANS WARFARIN-INDUCED SKIN NECROSIS ACQUIRED PROTEIN C INHIBITOR PROTEIN C IN BACTERIAL SEPSIS Baboon model With normally lethal dose of E. coli: Activated protein C prevents DIC, tissue necrosis and death Another inhibitor of thrombin formation blocks DIC but not tissue necrosis and death With normally sublethal dose of E. coli: Monoclonal antibodies to either protein C or its endothelial receptor promote DIC, tissue necrosis and death F.B. Taylor et al, J Clin Invest 1987; Blood 1991; Blood 2000 TRANSGENIC MICE THAT OVEREXPRESS THE ENDOTHELIAL APC RECEPTOR HAVE IMPROVED SURVIVAL AFTER ENDOTOXIN ADMINISTRATION J Thrombos Haemost 2005;3: 1351–1359 CIRCULATING ACTIVATED PROTEIN C IN SEVERE SEPSIS Survivors had higher APC levels and lower F1.2/APC ratios than non-survivors Blood 2004;104:3958 ENDOTHELIAL PROTEIN C ACTIVATION IS REDUCED IN SEPSIS Normal Sepsis Thrombomodulin NEJM 2001;345:408 Protein C receptor ANTICOAGULANT PROTEIN LEVELS IN MENINGOCOCCEMIA Relationship to multiorgan failure Mean level (% normal) ORGAN FAILURE? Protein C Antithrombin Protein S Yes 18 ± 7 53 ± 16 75 ± 19 No 42 ± 13 81 ± 20 87 ± 14 Blood 2000;96:3719 Protein C levels predict ICU survival as well as the APACHE II or SAPS II score Anesthesiology 2007;107:15 DIC PATHOPHYSIOLOGY Summary • Excess tissue factor + flowing blood = DIC • Inflammatory cytokines set the stage for DIC and contribute to tissue damage • Excessive fibrinolysis associated with higher bleeding risk • Acquired protein C deficiency associated with high risk of tissue necrosis/purpura fulminans DIAGNOSIS OF DIC DIC is likely when there is 1. A condition known to cause DIC 2. Evidence of accelerated fibrinolysis and clotting factor consumption LABORATORY TESTS IN DIC DIAGNOSIS ASSESS SEVERITY GUIDE TREATMENT FDP or D-Dimer Antithrombin III PT/INR Fibrinogen Alpha2-antiplasmin Fibrinogen PT/INR Protein C Platelet count Platelet count Fibrin monomer Alpha2-antiplasmin Death Is Coming OUTCOME IN DIC • 346 patients • Incidence of bleeding: 77% • Mortality Overall: With bleeding: Without bleeding: 68% 72% 63% • Most deaths from underlying disease, not bleeding Thromb Haemost 1980; 43:28-33 TREATMENT OF DIC • TREAT UNDERLYING DISEASE! • Clotting factor & inhibitor replacement Fresh frozen plasma Cryoprecipitate Platelets ?Antithrombin III, protein C concentrate • Pharmacologic inhibitors Heparin Antifibrinolytics REPLACEMENT THERAPY IN DIC Product Content Indication Risk FFP All clotting factors and inhibitors INR > 1.6 Volume, virus transmission Cryoprecipitate Fibrinogen, VIII, VWF Fibrinogen < 50-100 (?) "Feed the fire"? Platelets Platelets < 30-50K Antithrombin Purified antithrombin Low antithrombin? ? Activated protein C Purified APC Purpura fulminans? Low protein C? Bleeding PHARMACOLOGIC INHIBITORS IN DIC • • • • Anticoagulant: Unfractionated Heparin Little experience with LMWHs Antifibrinolytic: Epsilon aminocaproic acid (Amicar) Tranexamic acid (?availability) No controlled trials showing benefit Convincing anecdotal evidence of benefit in individual patients HEPARIN IN DIC Rationale: Prevent thrombin/fibrin formation and secondary fibrinolysis Indications: Cancer-associated DIC Acute leukemia and DIC Chronic DIC with aneurysm, etc Overt thrombosis Purpura fulminans? Concomitant antifibrinolytic Rx Risks: Exacerbate bleeding Drug-induced thrombocytopenia Low dose (eg, 500 U/hr) usually adequate ANTIFIBRINOLYTIC DRUGS H N 2 LYSINE H N CH CH CH CH CH COOH AMICAR (EACA) H N CH CH CH CH CH COOH 2 2 2 2 2 2 2 2 CH 2 TRANEXAMIC ACID 2 2 CH 2 H N CH CH 2 2 CH 2 CH 2 CH 2 COOH FIBRINOLYSIS Antifibrinolytic drug effects EACA Plasminogen TPA EACA Fibrin UK Plasmin FDP EACA Fibrinogen ANTIFIBRINOLYTIC THERAPY IN DIC Rationale: Inhibit activation of plasminogen/clot lysis Prevent bleeding Indications: DIC in promyelocytic leukemia DIC with severe bleeding, low antiplasmin? Risk: Thrombosis Amicar, 1 gram/hour i.v. with low dose heparin SPINAL ARTERY THROMBOSIS AFTER AMICAR TREATMENT Hum Pathol 1972;3:327 ANTIFIBRINOLYTIC THERAPY IN PROMYELOCYTIC LEUKEMIA • • • • APML often associated with DIC and hyperfibrinolysis, high risk of fatal intracranial hemorrhage In seven patients with APML, bleeding occurred only in those with severe alpha2-antiplasmin deficiency (<30%) Patients with low antiplasmin levels were treated with EACA plus low-dose heparin EACA treatment was associated with prompt cessation of bleeding, reversal of laboratory evidence of hyperfibrinolysis, and decreased need for blood product support Ann Intern Med 1986;105:873-7 62 yo man with spontaneous intracranial bleed PT 20.4 sec Plts 69K Fibrinogen 163 Antiplasmin < 25% Antithrombin 116% PSA > 10,000 DIC AND PROSTATE CARCINOMA 60 yo man post XRT for spine mets with diffuse bleeding 250 250 200 200 150 150 100 100 50 50 0 0 1 2 3 4 5 DAY 6 7 8 Pla te le ts F ib rin o g e n , m g /d l 300 PROTEIN C REPLACEMENT IN PURPURA FULMINANS A prospective, open-label clinical trial • Subjects: 36 patients with meningococcemia, shock and purpura fulminans Mean age = 12 (3 months-72 yrs) Mean protein C activity 18% • Intervention: Protein C concentrate, 100 IU/kg loading dose and 10 IU/kg/hr, adjusted to keep protein C activity in 80-120% range Two patients also received antithrombin concentrate OUTCOME OBSERVED PREDICTED Death 8% 50% Amputation 12% 30% Blood 2000;96:3719 RECOMBINANT ACTIVATED PROTEIN C INFUSION IN SEVERE SEPSIS NEJM 2001;344:699 • Subjects: 1690 patients with severe sepsis • Method: randomized, double-blind, placebo-controlled multicenter trial • Intervention: rAPC infusion vs placebo • Outcomes: Mortality lower in treated pts (24.7% vs 30.8%, p=.005) Serious bleeding more common in treated pts (3.5% vs 2%, p=.06) EFFECT OF rAPC INFUSION ON SURVIVAL IN SEVERE SEPSIS NEJM 2001;344:699 EFFECT OF rAPC INFUSION ON D-DIMER LEVELS NEJM 2001;344:699