Bleeding disorders
advertisement

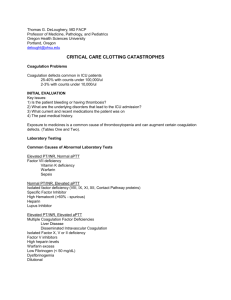
Bleeding disorders Doc. MUDr. L. Boudová, Ph.D. Bleeding disorders I. Vessels - increased fragility II. Platelets - deficiency or dysfunction III.Coagulation disorders IV.Combination I-III • I. Vessels • infections, drugs (hypersensitivity) • poor vascular wall: Ehlers-Danlos, scurvy; Cushing syndrome, old people • hereditary hemorrhagic teleangiectasia • amyloid Thrombocytes 150-300 000/mm3 normal 100 000/mm3 50 000/mm3 20 000/mm3 thrombocytopenia posttraumatic bleeding spontaneous bleeding Thrombocytopenia • • • • decreased production increased destruction sequestration dilution Splenomegaly a sign of an underlying disease a problem per se bigger spleen~ bigger function = destruction of blood cells Hypersplenism 1. splenomegaly 2. (pan) cytopenia 3. correction of blood cytopenia by splenectomy Immune thrombocytopenic purpura Idiopathic TP – but autoimmune! Antibodies against platelets Primary or secondary ITP • Acute – children • Abrupt onset, both sexes, 2 weeks after virosis, resolves within 6 mo, 20% chronic • Chronic – adults (F:M 3:1) • Petechial hemorrhages and ecchymoses • Easy bruising, skin, mucosa, nose, gums, soft tis., melena, hematuria, menstruation • Clin.: nonspecific – reflective of thrombocytopenia ITP - organs • Spleen - normal size • PB: megathrombocytes • BM:+ /- more megs • Therapy: splenectomy Thrombotic microangiopathies related clinical syndromes thrombotic thrombocytopenic purpura (TTP) hemolytic-uremic syndrome (HUS) ENDOTHELIAL INJURY WIDESPREAD HYALINE MICROTHROMBI OVERLAP - common features (TTP, HUS): • thrombocytopenia • microangiopathic hemolytic anemia • fever Thrombotic microangiopathies thrombotic thrombocytopenic purpura (TTP) hemolytic-uremic syndrome (HUS) Versus Disseminated intravascular coagulation Common: hyaline thrombi !!Differences: DIC: primary importance: activation of clotting system Thrombotic microangiopathies related clinical syndromes thrombotic thrombocytopenic purpura (TTP) hemolytic-uremic syndrome (HUS) ENDOTHELIAL INJURY WIDESPREAD HYALINE MICROTHROMBI OVERLAP - common features (TTP, HUS): • thrombocytopenia • microangiopathic hemolytic anemia • fever Thrombotic microangiopathies TTP HUS Common: thrombocytopenia, microangiopathic hemolytic anemia, fever neurological deficits (transient) renal failure adult women mostly no neurol. sympt. acute renal failure DOMINANT! children; E. coli O157:H7, verotoxin Microangiopathic hemolytic anemia hemolytic-uremic syndrome several fragmented red cells Thrombotic microangiopathies thrombotic thrombocytopenic purpura (TTP) hemolytic-uremic syndrome (HUS) Versus Disseminated intravascular coagulation Common: hyaline thrombi !!Differences: DIC: primary importance: activation of clotting system Disseminated intravascular coagulation (DIC) secondary complication of some serious condition consumption coagulopathy thrombohemorrhagic diathesis acute, subacute, chronic DIC: thrombotic and hemorrhagic diathesis activation of coagulation sequence Microthrombi hypoxia, infarctions Consumption →depletion of platelets and clotting factors + secondary activation of fibrinolysis hemorrhages Mechanisms of DIC trigger 1. Release of tissue factor or thromboplastic substances 2. Widespread endothelial injury DIC 1. obstetrics – 50%; abruptio placentae, retained dead fetus, septic abortion, amniotic fluid embolism, toxemia 2. neoplasms – 30%; adenocarcinomas, AML 3. infections – gram-negative sepsis 4. trauma, burns, extensive surgery 5. Other – snakebite, heat stroke, giant hemangioma, aortic aneurysm etc. DIC • Morphology microthrombi • Kidneys hemorrhages Microinfarcts, bilat. renal necrosis • lungs • Brain - microinfarcts, hemorrhage • Placenta • Spleen , liver • Endocrine organs: pituitary, adrenals DIC - clinical • microangiopathic hemolytic anemia, RDS – dyspnea, cyanosis • neurologic symptoms, oliguria, acute renal and circulatory failure, • Convulsions, coma • SHOCK Disseminated intravascular coagulation hyaline thrombi Sy Waterhouse - Friedrichsen