Epilepsy Programme Cost
advertisement
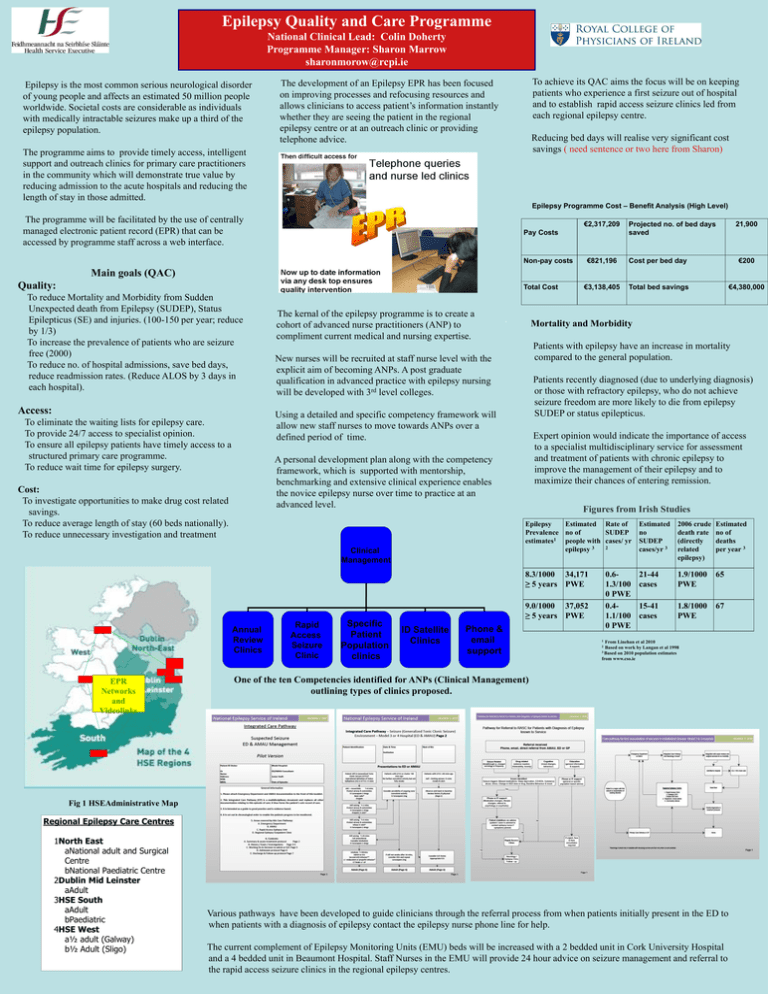
Epilepsy Quality and Care Programme National Clinical Lead: Colin Doherty Programme Manager: Sharon Marrow sharonmorow@rcpi.ie .Epilepsy is the most common serious neurological disorder of young people and affects an estimated 50 million people worldwide. Societal costs are considerable as individuals with medically intractable seizures make up a third of the epilepsy population. The development of an Epilepsy EPR has been focused on improving processes and refocusing resources and allows clinicians to access patient’s information instantly whether they are seeing the patient in the regional epilepsy centre or at an outreach clinic or providing telephone advice. To achieve its QAC aims the focus will be on keeping patients who experience a first seizure out of hospital and to establish rapid access seizure clinics led from each regional epilepsy centre. Reducing bed days will realise very significant cost savings ( need sentence or two here from Sharon) The programme aims to provide timely access, intelligent support and outreach clinics for primary care practitioners in the community which will demonstrate true value by reducing admission to the acute hospitals and reducing the length of stay in those admitted. Epilepsy Programme Cost – Benefit Analysis (High Level) The programme will be facilitated by the use of centrally managed electronic patient record (EPR) that can be accessed by programme staff across a web interface. €2,317,209 Pay Costs Non-pay costs 21,900 Projected no. of bed days saved €821,196 Cost per bed day €200 €3,138,405 Total bed savings €4,380,000 Main goals (QAC) Quality: Total Cost To reduce Mortality and Morbidity from Sudden Unexpected death from Epilepsy (SUDEP), Status Epilepticus (SE) and injuries. (100-150 per year; reduce by 1/3) To increase the prevalence of patients who are seizure free (2000) To reduce no. of hospital admissions, save bed days, reduce readmission rates. (Reduce ALOS by 3 days in each hospital). Access: The kernal of the epilepsy programme is to create a cohort of advanced nurse practitioners (ANP) to compliment current medical and nursing expertise. Mortality and Morbidity Patients with epilepsy have an increase in mortality compared to the general population. New nurses will be recruited at staff nurse level with the explicit aim of becoming ANPs. A post graduate qualification in advanced practice with epilepsy nursing will be developed with 3rd level colleges. Patients recently diagnosed (due to underlying diagnosis) or those with refractory epilepsy, who do not achieve seizure freedom are more likely to die from epilepsy SUDEP or status epilepticus. Using a detailed and specific competency framework will allow new staff nurses to move towards ANPs over a defined period of time. To eliminate the waiting lists for epilepsy care. To provide 24/7 access to specialist opinion. To ensure all epilepsy patients have timely access to a structured primary care programme. To reduce wait time for epilepsy surgery. Expert opinion would indicate the importance of access to a specialist multidisciplinary service for assessment and treatment of patients with chronic epilepsy to improve the management of their epilepsy and to maximize their chances of entering remission. A personal development plan along with the competency framework, which is supported with mentorship, benchmarking and extensive clinical experience enables the novice epilepsy nurse over time to practice at an advanced level. Cost: To investigate opportunities to make drug cost related savings. To reduce average length of stay (60 beds nationally). To reduce unnecessary investigation and treatment Clinical Management Annual Review Clinics EPR Networks and Videolinks . Rapid Access Seizure Clinic Specific Patient Population clinics Figures from Irish Studies Epilepsy Estimated Rate of Prevalence no of SUDEP estimates1 people with cases/ yr 2 epilepsy 3 Estimated no SUDEP cases/yr 3 2006 crude death rate (directly related epilepsy) Estimated no of deaths per year 3 8.3/1000 34,171 ≥ 5 years PWE 21-44 cases 1.9/1000 PWE 65 15-41 cases 1.8/1000 PWE 67 0.61.3/100 0 PWE 0.41.1/100 0 PWE 9.0/1000 37,052 ≥ 5 years PWE ID Satellite Clinics Phone & email support 1 From Linehan et al 2010 2 Based on work by Langan et al 1998 3 Based on 2010 population estimates from www.cso.ie One of the ten Competencies identified for ANPs (Clinical Management) outlining types of clinics proposed. Fig 1 HSEAdministrative Map Regional Epilepsy Care Centres 1North East aNational adult and Surgical Centre bNational Paediatric Centre 2Dublin Mid Leinster aAdult 3HSE South aAdult bPaediatric 4HSE West a½ adult (Galway) b½ Adult (Sligo) Various pathways have been developed to guide clinicians through the referral process from when patients initially present in the ED to when patients with a diagnosis of epilepsy contact the epilepsy nurse phone line for help. The current complement of Epilepsy Monitoring Units (EMU) beds will be increased with a 2 bedded unit in Cork University Hospital and a 4 bedded unit in Beaumont Hospital. Staff Nurses in the EMU will provide 24 hour advice on seizure management and referral to the rapid access seizure clinics in the regional epilepsy centres.