The Alternative Quality Contract (AQC) model
advertisement

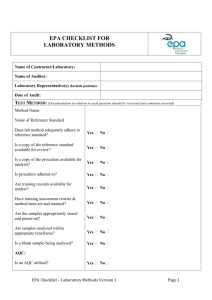
The Alternative Quality Contract (AQC) Model: A Progress Report Jeffrey L. Simmons, M.D. Medical Director for Behavioral Health Blue Cross Blue Shield of Massachusetts April 3, 2014 The Alternative Quality Contract (AQC): Key Components Global Budget • Covers all medical services • Health status adjusted Quality Incentives • Based on historical claims • Ambulatory and hospital • Shared risk • Declining trend • Significant earning potential Long-Term Contract • Nationally accepted measures • Sustained partnership • 5-year agreement • Supports ongoing investment Blue Cross Blue Shield of Massachusetts 2 Linking Quality and Efficiency As quality improves, provider share of surplus increases or share of deficit decreases Blue Cross Blue Shield of Massachusetts 3 Nationally Accepted and Validated Measure Set for Performance Incentives The 60+ measures include: Ambulatory Process Outcome • Preventive screenings • Acute care management • Chronic care management – Depression – Diabetes – Cardiovascular disease • Control of chronic conditions – Diabetes – Cardiovascular disease – Hypertension Hospital Evidence-based care elements for: • Heart attack (AMI) • Heart failure (CHF) • Pneumonia • Surgical infection prevention • Post-operative complications • Hospital-acquired infections • Obstetrical injury • Mortality (condition –specific) ***Triple weighted*** Patient Experience Blue Cross Blue Shield of Massachusetts • Access, Integration • Communication, Whole-person care • Discharge quality, Staff responsiveness • Communication (MDs, RNs) 4 Incentive Risk • BCBSMA employs several strategies Incentive Risk • Variation in costs and outcomes due to factors within providers’ control— care processes, unnecessary utilization, etc. • Examples: HbA1c control among diabetics, ED use for ambulatorycare sensitive visits Blue Cross Blue Shield of Massachusetts to insulate providers from insurance risk in the AQC: – Health status adjustment – Use of network-wide trend as benchmark for budget-setting – Prescription drug benefit adjustment – Reinsurance requirements/ contract terms – Caps on provider liability for budget deficits – Upside risk-only in payment for quality performance 5 AQC Groups (Current as of March, 2014) Blue Cross Blue Shield of Massachusetts 6 AQC Participation (Current as of March 2014) Most PCPs and specialists are in AQC Contracts today Most of our HMO Blue members are patients of AQC groups* 100% 100% 15% 11% 14% 75% 75% 50% 50% 85% 89% 86% 25% 25% 0% 0% PCPs HMO Blue Members Specialists * In-State HMO members of an AQC PCP, membership may fluctuate Blue Cross Blue Shield of Massachusetts 7 AQC Improving Adult and Pediatric Care Quality and Outcomes: Improvement of the 2009 Cohort of AQC Groups from 2007-2012 Adult Chronic Care Pediatric Care Optimal Care 100 83.1 84.0 79.6 80.4 81.1 86.0 86.7 80.8 81.0 88.2 89.9 Adult Health Outcomes 91.3 91.6 92.2 92.1 69.7 70.7 71.6 71.7 79.2 80.3 77.7 68.1 69.5 72.2 74.0 68.3 65.6 61.5 59.8 62.1 61.2 61.4 61.9 62.2 61.9 50 2012 2007 BCBSMA HEDIS National Average 2012 2007 BCBSMA HEDIS National Average 2012 2007 BCBSMA HEDIS National Average These graphs show that the AQC has accelerated progress toward optimal care since it began in 2009. The first two scores are based on the delivery of evidence-based care to adults with chronic illness and to children, including appropriate tests, services, and preventive care. The third score reflects the extent to which providers helped adults with serious chronic illness achieve optimal clinical outcomes. Linking provider payment to outcome measures has been one of the AQC’s pioneering achievements. Blue Cross Blue Shield of Massachusetts 8 What impact has the AQC had on BH care? • Primary impact so far has been on awareness and staffing – Perception of BH as a key component requiring active management Increasing interest in Collaborative Care Model Emerging measures – 11/17 AQCs chose a serial PHQ-9 Patient Reported Outcomes Measure – Addition of behavioral health clinicians to staffing patterns – Partnerships with organized behavioral health clinical groups • Academic review of the use of mental health and substance abuse services has just begun in partnership with the Harvard and Johns Hopkins Schools of Public Health – Impact on mental health and substance abuse quality gates (HEDIS Antidepressant Measure and Total Readmissions) – Impact on inpatient and outpatient service utilization – Impact on provision of medical services to those with BH needs Blue Cross Blue Shield of Massachusetts 9 AQC Impact on Medical Care for Behavioral Health Members Diabetic HgbA1c>9 25 15 Non-BH 10 BH 5 0 2009 2010 2011 Diabetic LDL-C<100 % Preliminary analysis shows that AQC-based care results in comparable improvement in key medical measures for behavioral health members. % 20 66 64 62 60 58 56 54 52 50 Non-BH BH 2009 2010 2011 Hypertension<140/90 80 % 75 Non-BH 70 BH 65 60 2009 Blue Cross Blue Shield of Massachusetts 2010 2011 10 What do AQC Providers want from BH Providers? • High impact interventions for those most in need – Full integrated continuum of care – Inpatient admission and ER avoidance where appropriate • Urgent access to adult and child psychiatric consultation • Appropriate and timely services in the PCP’s or pediatrician’s office – Collaborative Care – a new professional model – Appropriate use of video technology • Effective communications to and from BH providers – Shared EMR or standardized info/data exchange • Reliable and valid measurement of outcomes – Standardized measure sets – PROMS • Partnership on cost and quality – Innovative payment arrangements Blue Cross Blue Shield of Massachusetts 11 How will behavioral health practices be organized to meet these needs and what form will reimbursement take? • Payment Fee-for-service Quality incentives (process measures and outcomes) Case rates Episode rates Full risk-sharing • Structures Salaried Staff Multidisciplinary Groups Bricks and Mortar Virtual CMHCs Small Groups Solo Practice Blue Cross Blue Shield of Massachusetts 12