Coagulation Laboratory
advertisement

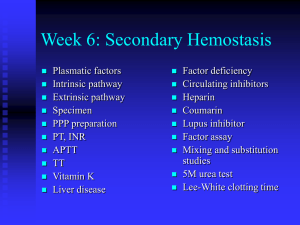
Renee Wilkins, Ph.D., MLS(ASCP)CM MLS 322 Clinical Hematology School of Health Related Professions University of Mississippi Medical Center What is hemostasis? The process in circulation where the blood is maintained within the blood vessels Depends on the balance of Vascular Plasma coagulation factors Platelets Fibrinolytic system Primary Hemostasis PLATELETS Hemostasis Primary hemostasis Blood vessel constricts (vasoconstriction) Platelets adhere and aggregate to damaged area of the vessel wall Results in the formation of the platelet plug Platelets must be adequate in number and must be functioning normally in order for the platelet plug to form ○ Thrombocytopenia ○ Aspirin therapy Platelets (thrombocytes) Cellular fragments of megakaryocytes that contain granules Circulate 9-12 days 2-4 μm Normal platelet count is 150-400,000/μL 100,000 are needed to perform platelet function testing Thrombocytopenia is the most common cause of abnormal hemostasis Platelet Alpha granules within the organelle contain platelet derived growth factor, platelet factor 4, FV, FXIII, fibrinogen, vWF Formation of platelet plug Adhesion (1-2 seconds) Platelets adhere to collagen fibers and vWF to form a bridge (glycoprotein Ib) Activation Morphological and functional changes Increases internal Ca++, swelling occurs Glycoprotein IIb/IIIa is activated Aggregation (10-20 seconds) Vasoactive substances like ADP and thrombozane A2 are released along with platelet procoagulants gp IIb/IIIa is exposed and binds to fibrinogen Other platelets are stimulated to adhere and aggregate When activation and primary adhesion have been achieved, platelets commence discharge of granule contents. Granule contents include ADP, adenosine triphosphate (ATP), serotonin, calcium, vWF, Factor V, and fibrinogen Once the plug is formed (1-3 minutes), the platelet mass consolidates to a dense thrombus (3-5 minutes), then retracts and stabilizes (5-10 min) fibrinogen Platelet glycoprotein Ib von Willebrand factor blood vessel wall/subendothelium collagen Primary platelet plug platelets fibrinogen Platelets in coagulation Platelet factor 3 (PF3) is a phospholipid that resides on or within the platelet PF3 is required in the activation of certain coagulation factors (to help form thrombin) Diseases of Primary Hemostasis Bleeds from skin or mucous membranes Factor abnormalities are usually internal Disorders of the vascular system Abnormalities or damage of lining of blood vessels or subendothelial structures Superficial bleeding (bruises, petechiae) Platelet count and factors are normal Platelet disorders Thrombocytopenia (<50x109/L) ○ Asymptomatic to severe Thrombocytosis (>450x109/L) Diseases of Primary Hemostasis Inherited (functional disorders) von Willebrand Disease (vWD) [adhesion] Bernard-Soulier syndrome (adhesion) Glanzmann Thrombasthenia (aggregation) May Hegglin anomaly (quantitative) Disorders of pregnancy (quantitative) Aquired Idiopathic thrombocytopenic purpura (ITP) Drug-induced platelet dysfunction ○ Aspirin induced platelet dysfunction ○ Aspirin resistance von Willebrand Disease Inherited, up to 3% of U.S. population Qualitative or quantitative abnormality of von Willebrand Factor (vWF) – fails to bridge gap (NOT a platelet disorder) vWF is a cofactor to Factor VIII (VIII:vWF complex) Excessively heavy or prolonged menstrual bleeding occurs in 20% of women ○ vWD may be the cause of menorrhagia in as many as 20% of these women Other symptoms include easy bruising and gingival bleeding 3 types with Type 2 containing 4 subtypes Nature of vWF The vWF molecule (protein) is a chain of identical subunits called multimers vWF is synthesized in alpha granules of megakaryocytes Primary hemostasis: vWF bridges GPIb/IX on platelets and collagen to form the plug Secondary hemostasis: vWF binds to FVIII which ultimately leads to fibrin formation vWF in plasma varies in size, but most binds with VIII in plasma (1:1) FVIII is formed in liver before release vWD glycoprotein Ib Normal Platelet No von Willebrand factor means no adhesion… von Willebrand disease blood vessel wall On the flip side…. Giant Platelet No glycoprotein Ib means no adhesion…. Bernard-Soulier von Willebrand factor blood vessel wall Bernard-Soulier syndrome A.k.a. giant platelet syndrome Rare autosomal recessive disorder <1 in 1,000,000 Moderate to severe thrombocytopenia Abnormal platelet function due to lack of GPIb/IX complex on platelet Homozygous individuals have lifelong bleeding tendency; heterozygous have not significant bleeding Glanzmann Thrombasthenia Rare deficiency of glycoprotein IIb/IIIa on platelet gp IIb/IIIa binds fibrinogen and is essential to platelet aggregation Platelet count normal, but bleeding prolonged Fails to aggregate with agonists ADP Epinephrine Collagen May-Hegglin anomaly Moderate macrothrombocytopenia (large platelets, low #) Dohle-like inclusions in WBCs Associated with abnormalities of MYH9 gene Disorders of Pregnancy Incidental thrombocytopenia of pregnancy Occurs in 5-7% of pregnancies Poses no risk for neonatal thrombocytopenia Thrombocytopenia from pre-eclampsia Pre-eclampsia is a hypertensive disorder of pregnancy (7-10%) 10-20% of pre-eclamptic women will develop thrombocytopenia Prolonged bleeding Pathogenesis unknown Idiopathic Thrombocytopenic Purpura (ITP)--autoimmune Children No gender preference Platelet count <20x109 Abrupt onset of bleeding Infection 1-3 wks prior Lasts 2-6 weeks ACUTE Adults Females 3:1 Platelet count 30-80x109 Insidious onset of bleeding No history of infection Lasts months to years CHRONIC Drug induced platelet dysfunction Aspirin inhibits prostaglandin production and Thromboxane A2 (TXA2) Aspirin irreversibly acetylates the cyclooxygenase enzymes which prevents formation and release of thromboxane A2 Platelets affected by aspirin continue to circulate but are no longer capable of functioning COX-1 Thromboxane Aspirin resistance Evidence suggests that significant insensitivity (5% - 60%) to aspirin occurs among patients with defined coronary disease and stroke Some individuals may have to take alternative drugs (i.e. Plavix®) Plavix (clopidigrel) affects the ADP receptor (P2Y12) which inhibits gp IIb/IIIa receptor that binds fibrinogen Aspirin & Clopidogrel Effects QUESTION Cells involved in hemostasis are: Erythrocytes Granulocytes Lymphocytes Thrombocytes QUESTION Normal platelets have a circulating lifespan of approximately: 5 days 10 days 20 days 30 days QUESTION Aspirin affects platelet function by interfering with platelets’ metabolism of: Prostaglandins Lipids Carbohydrates Nucleic acids QUESTION Platelet activity is affected by: Calcium Aspirin Hyperglycemia Hypoglycemia QUESTION Thrombocytopenia is a characteristic of: Classic von Willebrand disease Hemophilia A Glanzmann thrombasthenia May-Hegglin anomaly QUESTION Which of the following is the most common cause of an abnormality in hemostasis? Decreased plasma fibrinogen level Decreased Factor VIII level Decreased Factor IX level Quantitative abnormality of platelets QUESTION Which of the following is a true statement about acute idiopathic thrombocytopenic purpura (ITP)? It is found primarily in adults Spontaneous remission usually occurs within several weeks Women are more commonly affected Peripheral destruction of platelets is decreased QUESTION Which of the following is characteristic of platelet disorders? Deep muscle hemorrhage Retroperitoneal hemorrhage Mucous membrane hemorrhage Severely prolonged clotting times QUESTION Thrombocytosis would be indicated by a platelet count of: 100 x 103/μL (100 x 109/L) 200 x 103/μL (200 x 109/L) 300 x 103/μL (300 x 109/L) 600 x 103/μL (600 x 109/L) QUESTION vWF antigen can be found in which of the following? Myeloblast Monoblast Lymphoblast Megakaryoblast QUESTION Alpha granules are found on the platelet in: Peripheral zone Sol gel zone Organelle zone Membranes Secondary Hemostasis COAGULATION FACTOR INVOLVEMENT Secondary Hemostasis Results in the formation of a blood clot because of coagulation factors Forms fibrin network and thrombus that stabilize the plug/clot Stops bleeding completely Lysis (fibrinolysis) of the clot begins and final repair of injury takes place Thrombin acts on fibrinogen to form fibrin strands (clot) Secondary Hemostasis Coagulation factors are proteins (with exception to thromboplastin and calcium) All are involved in generating insoluble fibrin (cascade) They can be divided into 3 families based on properties: Fibrinogen group (thrombin sensitive) – fibrinogen, FV, FVIII, FXIII Prothrombin group (vitamin K dependent) – Factors II, VII, IX, X, Protein C and Protein S Contact family – Factor XII, Factor XI, prekallikrein and HMWK Vitamin K Vitamin K is inhibited by warfarin (Coumadin®) All factors in the prothrombin group are affected Individuals on warfarin need to monitor vitamin K intake (hypercoag) Factors in RED are affected by vitamin K QUESTION Coagulation factors affected by coumarin (warfarin) drugs are: VIII, IX and X I, II, V and VII II, VII, IX and X II, V and VII ANSWER Coagulation factors affected by coumarin drugs are: VIII, IX and X I, II, V and VII II, VII, IX and X (vitamin K dependent) II, V and VII Mechanism of Coagulation 1. 2. 3. Generation of Thromboplastic activity Generation of thrombin Conversion of fibrinogen to fibrin Pathways for the Coagulation Cascade Intrinsic pathway Extrinsic pathway Common pathway Intrinsic vs. Extrinsic Intrinsic All factors are contained in the blood Extrinsic Activated by tissue thromboplastin (FIII) Thromboplastin is released from damaged cells and tissues outside the circulating blood Intrinsic Pathway Circulating blood contains all components that lead to activation of Factor X HMWK (Fitzgerald) and prekallekrein (Fletcher) activate FXII to FXIIa Factor XII activates FXI, which in turn, activates FXI (now FXIa) in the presence of Ca++ ions Factor IX forms a complex with FVIII (with Ca and phospholipid on platelets) which activates FX Factor XI and XII are “contact factors” b/c their activation is initiated by contact with subendothelial basement membrane that is exposed at the time of a tissue or blood vessel injury Intrinsic Pathway Also these complex reactions take place slowly, they account for the most coag activities in the body The APTT test can monitor the intrinsic pathway The APTT measures: Factors XII, XI, X, IX, VIII, V, II, and fibrinogen Common Pathway Factors Extrinsic Pathway Occurs when tissue thromboplastin (not in blood) enters vasculature Factor VII is activated to VIIa by Ca++ and tissue thromboplastin (FIII) Factor VIIa can now activate FX (common) Extrinsic pathway vascular injury X tissue thromboplastin + VIIa Ca++ VII X V Xa (VVa) II (prothrombin) IIa (thrombin) I (fibrinogen) fibrin Extrinsic Pathway The extrinsic pathway can also quickly provide small amounts of thrombin (leads to fibrin formation) Thrombin can also enhance the activity of Factor V and VIII (intrinsic pathway) The PT test (prothrombin time) monitors the extrinsic pathway The PT measures Factors VII, X, V, II, and I Common QUESTION Which of the following factors is used only in the extrinsic coagulation pathway? II V VII VIII ANSWER Which of the following factors is used only in the extrinsic coagulation pathway? II V VII VIII Common Pathway Begins with FX Activation of FX is the point where both the intrinsic and extrinsic pathway converge Once Xa is formed, it’s cofactor (FV), in the presence of Ca++ and PF3 convert prothrombin to thrombin Thrombin acts to convert fibrinogen to fibrin Factor XII stabilizes the clot Interpreting abnormal tests Disorders of the coag cascade Hemophilia A Factor VIII deficiency (VIII:C subunit) Have normal VIII:vWF molecule vWD is deficient of VIII:vWF Hemophilia B factor IX deficiency Mild, moderate, or severe (need to test) Hemophilia C Factor XI deficiency 4th most common inherited bleeding disorder Factor XII deficiency Causes prolonged APTT Normal PT, PFA 100 and TT No signs of a bleeding disorder FXII may be more involved with inflammation since FXII deficient individuals have higher rates of infection. Disorders of the coag cascade Vitamin K deficiency diet, malabsorption disorders, liver disease pregnancy Can prolong factor assays that include II, VII, IX, and X…as well as the PT and APTT Found in leafy green vegetables ○ Green tea (712 μg) ○ Avocado (634) ○ Turnip greens (408) ○ Brussels sprouts (317) ○ Broccoli (200) Anti-coags that can affect the cascade aPPT Direct thrombin inhibitors: -Hirudin (leaches) -Argatroban Vitamin K antagonists: -Coumadin® (warfarin) Heparins: -Heparin -Lovenox® (enoxaparin), LMWH Factor Xa inhibitors: -Arixtra® PT Heparin Heparin and its low molecular weight derivatives are effective at preventing deep vein thromboses and pulmonary emboli in patients at risk Heparin binds to the enzyme inhibitor ATIII causing a conformational change that results in its activation through an increase in the flexibility of its reactive site loop The activated ATIII then inactivates thrombin and other proteases involved in blood clotting, most notably FXa Fibrinolysis….almost done Fibrinolysis is the last stage of coagulation that causes the dissolution of the fibrin clot Fibrinolysis is mediated by the conversion of plasminogen to plasmin Activation of plasminogen can be due to: Intrinsic activation- initiated by FXIIa & kallikrien Extrinsic activation- stimuli like vascular injury, ischemia, exercise and stress Exogenous (therapeutic) activation- drugs like streptokinase, urokinase, tissue plasminogen activator (tPA)…for strokes FIBRINOGEN FIBRIN Fibrin monomer thrombin D E Fibrin polymer D Factor XIII plasminogen plasmin Crosslinked fibrin polymer plasmin X fraction: Y fraction “Stabilized Clot” Degradation products D fragments D-dimer (crosslinked D-domains) D fragments E fragments Fibrinolysis testing Most commercial FDP kits detect D & E fragments which are both products of fibrin and fibrinogen degradation (latex kits) The D-Dimer test is a specific marker for plasmin degradation of fibrin (latex kit or ELFA) Latex particles are coated with anti-human fibrinogen SPR – Solid Phase Reaction Sample goes here Fibrinolysis Disease states can either increase or decrease fibrinolytic activity Disseminated Intravascular Coagulation Trauma from surgical procedures or accidents Deficiencies in or consumption of the various inhibitors and activators of the fibrinolytic system DIC Uncontrolled formation of thrombi/fibrin Fibrinolysis is activated but rapidly consumed thus leading to depletion of coag factors and platelets Bleeding, shock, microscopic thrombi Petechiae, hematomas, deep tissue bleeding Associated with obstetric emergencies, septicemia, burns, crush injuries, cardiac and vascular disorders DIC lab findings PT and PTT usually prolonged, not always Fibrinogen – 2-3X normal (150-400) Platelets – thrombocytopenia (<50,000) FDPs – usually elevated D-Dimer – elevated DVT Occurs when a blood clot forms in one of the large veins, usually in the lower limbs The blood clot can break loose and move into the: Lungs (Pulmonary Embolism) Brain (Stroke) DVT facts DVT occurs in about 2 million Americans every year. Up to 600,000 people are hospitalized in the U.S. each year for DVT. Fatal PE may be the most common preventable cause of hospital death in the United States. In the elderly, DVT is associated with a 21% mortality rate, and PE is associated with a 39% mortality rate. PE is the leading cause of maternal death associated with childbirth. A woman's risk of developing emboli is six times greater when she is pregnant Lab tests D-Dimer is most useful b/c it tests for the breakdown of the fibrin mesh >10,000 critical (>500 pos) FDPs are sometimes useful in post-op deep vein thrombosis Natural anticoagulants In vivo anticoagulants help to prevent thrombosis Antithrombin III (ATIII) ○ Inhibits thrombin and factor Xa, but can also affect Factors IXa, XIa, and XIIa ○ Deficiencies can be inherited or acquired ○ ATIII can be given as treatment for thrombotic disorders Heparin Cofactor ○ ATIII heparin cofactor and HC-II are thrombin inhibitors that are present in human plasma ○ They are produced by mast cells ○ Unfractioned heparin binds to ATIII to target factors IX, X, V, and II (prothrombin)..detected by APTT or both (if dose is high Natural Anticoagulants (cont’d) Protein C and Protein S Protein C is made in the liver and circulates as zymogen It is converted to activated protein C (APC) by thrombin and thrombomodulin APC with its cofactor, protein S, can inactivate FV and VIII Protein C/S Disorders APC Resistance Also factor V Leiden Factor V Leiden is a genetic mutation that alters Factor V so that APC cannot bind and inactivate it This can lead to thrombophilia (hypercoagulability…..thrombosis) 20-50% of inherited thrombophilias Discovered at the Univ. of Leiden (Netherlands) QUESTION A deficiency of protein C is associated with which of the following? Prolonged APTT Decreased fibrinogen (<100) Increased risk of thrombosis Spontaneous hemorrhage ANSWER A deficiency of protein C is associated with which of the following? Prolonged APTT Decreased fibrinogen (<100) Increased risk of thrombosis Spontaneous hemorrhage QUESTION Which of the following is a characteristic of Factor XII deficiency? Negative bleeding history Normal clotting times Decreased risk of thrombosis Epistaxis A coagulation lab performs: Routine Testing PT(INR) aPTT Fibrinogen D-Dimer FDP Thrombin Time PFA-100 Bleeding Time Special Coag Factor Assays Lupus Panels Mixing Studies ATIII Plasminogen von Willebrand LMWH Euglobulin clot lysis Factor XIII Factor Inhibitor Fletcher Factor APC Resistance Antiphospholipid testing (ELISA) HIT (ELISA) PAI-1 (ELISA) Coagulation Basics 3.2% sodium citrate tubes Anticoag to blood ratio is crucial a short draw could prolong results Ratio is 9 parts whole blood to 1 part anticoagulant (sodium citrate) Discard first tube b/c it may be contaminated with tissue fluid (tissue thromboplastin may activate extrinsic system..prolonged PT) Anticoagulants to remember Anticoagulants (EDTA, citrate) remove calcium to prevent clotting (in vitro) Heparin (FIX, X, V, II) and warfarin (vitamin K dependent factors II, VII, IX, X) prevent the conversion of prothrombin (factor II) to thrombin (in vivo) Centrifugation Samples are spun in a refrigerated centrifuge fro 10-15 minutes at 3500 rpms to obtain platelet poor plasma Refrigeration maintains labile factors VIII and V Samples for assays that are performed at a later date are: Immediately separated Checked for platelet count (<10x109) Phospholipids from lysed platelets can falsely effect phospholipid based tests (Lupus testing) frozen rapidly at -72°C Thawed rapidly to avoid cryoprecipitation (VIII) Automated Testing Automated (photooptical) or semi-automated End point of reaction is a clot (measured in seconds) Clot formation is timed automatically and is detected by a photocell that reads the optical density change when the clot is formed Contains a heat block to bring reagents and plasma to 37°C Reagents not in use are kept at 4-6°C to maintain integrity (on instrument, in fridge, or cooling block) Analyzers automatically pipette (or require manual pipetting) PT, APTT, factor assays, fibrinogen, etc STart 4 Analyzer Electromechanical method PT testing Prothrombin time (extrinsic & common pathways) Method of choice for monitoring Coumadin (Vit K antagonist) Reagents include Calcium Chloride Contained together in a Thromboplastin single vial Both of these are needed to initiate the extrinsic pathway and test for any deficiencies PT Testing Normal PT = 10-14 seconds In the past, many labs performed a PT test with (thromboplastin) and a separate PT(INR) test for those on oral anticoagulant therapy to determine an INR Now, some labs run the PT(INR) on all patients and have discontinued the routine PT PT INR INR – International PT standardization for oral anticoagulant therapy monitoring The WHO and the International Committee on Thrombosis and Hemostasis recommend that PT tests run on patients on oral therapy use an INR value INR values are independent of the reagents and methods used, and are specifically intended for assessing patients stabilized on long term oral anticoagulant therapy PT(INR) To standardize the PT, a calculation is used to obtain the International Normalized Ratio (INR) for people on warfarin (normal INR = up to about 4) Patient PT INR = X ISI Mean PT (of normal population) International Sensitivity Index Current normal PT in lab = 9.4-12.5 PT INR Note: When coumadin is initiated, with a loading dose, there is a rapid depletion of Factor VII during the first 48 hrs, with other factors not being fully affected until about 5 days after Prolonged PT times before 5 days have no correlation with any therapeutic benefits Measurements are not suggested until the 5th day of therapy QUESTION The prothrombin time (PT) test requires that the patient’s citrated plasma be combined with: Platelet lipids Thromboplastin Ca++ and platelet lipids Ca++ and thromboplastin ANSWER The prothrombin time (PT) test requires that the patient’s citrated plasma be combined with: Platelet lipids Thromboplastin Ca++ and platelet lipids Ca++ and thromboplastin APTT Testing Activated Partial Thromboplastin Time Screens for deficiencies involving factors of the intrinsic pathway Most sensitive to Factors VIII, IX, X, XI & XII Can be prolonged in severe Factor V deficiency Fresh citrated plasma provides all factors necessary for the intrinsic clotting mechanism except ionic Ca (removed by citrate) platelet factor (removed by centrifugation APTT testing An activator and phospholipid is incubated with patient plasma to activate contact factors (creates negatively charged surface) Activators: kaolin, celite, ellagic acid, silica Phospholipids: rabbit brain, cephalin, soy bean Calcium is added after incubation and the time it takes for a clot to form observed Normal aPTT = varies from about 24-34 seconds Actin® is a reagent that contains ellagic acid and rabbit brain APTT Note: Heparin can be given continuously (IV) or in subcutaneous mini-doses Care should be taken not to obtain samples above heparin line Patients should be monitored prior to next dose if APTT is to be meaningful Heparin contamination can sometimes severely prolong APTT (>60 seconds) Another APTT reagent: PSL Panthromtin SL is more sensitive than the routine APTT reagent It is used in some labs to detect inhibitors affecting the APTT The “SL” refers to Lupus and is used to detect risk of disease If prolonged and heparin is ruled out, further Lupus testing is performed Fibrinogen Testing Thrombin converts fibrinogen to fibrin Thrombin is added to plasma and the time it takes to clot (determined in seconds) is proportional to the fibrinogen concentration in plasma Calibration curves are needed for each new lot of thrombin Normal range = 150 – 400 mg/dL Anything >500 is run manually on a semiautomated instrument (i.e. Start 4) Factor Assays Allows testing for specific factors by making a series of dilutions on a control, reference (deficient) plasma, and patient 3 (automated) dilutions made: 1:10, 1:20, 1:40 Run a PT or APTT, depending on what factor is being tested The factor deficient plasma has every factor except the desired factor Factor assays PT: 2, 7, 5, 10 PTT: 9, 8, 11, 12 The 3 points of the reference (calibration curve) is plotted and a best fit line is drawn (automated) The 3 points of the patient or control are plotted and compared to reference If patient is below reference, then the factor activity is low (normal 50-150%) If patient is above, then factor is high (no worry) If patient crosses the reference line (not parallel), then an inhibitor is suspected Factor graph (basic example) 1:40 Inhibitor present, possibly FVIII inhibitor or Lupus anticoagulant 1:20 1:10 reference Curvilinear paper is used to obtain straight line Low factor Factor XIII Stabilizes clot Uses 2 tubes containing plasma are clotted with Calcium chloride 5M urea added to one tube Acetic acid added to the other Checked (in water bath) at 30 min intervals to monitor clot If clot dissolves in 10-30 min, FXIII deficiency Normal clots remain over an hour Umbilical stump hemorrhage is the hallmark of FXIII deficiency Lupus Anticoagulant Panel LA (or inhibitor) is thought to be a nonspecific phospholipid antibody Prolonged PTT is a routine screening test If after testing, a lupus inhibitor is detected, mixing studies are performed to rule out factor deficiency LA testing Lupus panel consists of: APTT: Actin FSL and Pathromtin SL Dilute Russell’s Viper Venom Test (DRVVT) – modified APTT that uses viper venom as an activator. Very sens. DRVV Confirm – higher concentrations of phospholipids. This higher concentration of phospholipids allows the reagent to “correct” the prolonged DRVVT. Anti-cardiolipin, anti-phosphatidylserine, anti-prothrombin and beta-2-glycoprotein Sta-Clot kit detects lupus inhibitor ○ Tube A is an APTT ○ Tube B is an APTT with phospholipid ○ If clotting changes more than 8 seconds, it is positive Triturus tests (ELISA) Antiphospholipid tests (for APS syndrome, SLE, etc) HIT Testing PAI-1 Inhibitor HIT Heparin Induced Thrombocytopenia Tests for anti-platelet antibodies to the PF4 receptor on platelets In patients on heparin or who have had previous exposure to heparin Platelet count dramatically drops by 50% after second exposure Must be removed from heparin and given alternative treatment (i.e. argatroban, LMWH) Euglobulin Lysis Overall screen of the fibrinolytic system Fibrinogen, plasmin and fibrinolytic agents are precipitated (left in tube) Inhibitors of fibrinolysis are discarded The precipitate is re-dissolved in buffer and thrombin is added to form a clot It is put in a water bath and monitored every 10 min for 1 hour then at 2 and 24 hours Normal patient >2 <24 hours Abnormal <2 hrs increased fibrinolytic activity >24 hours decreased fibrinolytic activity ATIII testing Naturally occurring inhibitor that neutralizes the serine protease thrombin, FIXa, Xa, Xia and XIIa The inhibition of thrombin by antithrombin is greatly accelerated by heparin Chromogenic assays that inhibit thrombin or Fxa, microlatex assays, nephalometry are frequent assays. Bleeding Time Tests for platelet function Normal 3-9 minutes Patient MUST have a Plt count >50,000 Blood pressure cuff is applied (40) Small incision made with lancet and the bleeding is “wicked” with paper disc every 30 seconds until plug forms Test is terminated if bleeding does not stop after 15 minutes Abnormal bleeding disorders include: Thrombasthenia vonWillebrand disease Bernard Soulier Aspirin sensitivity PFA 100® Platelet Function Analyzer Simulates in vivo conditions Uses 2 cartridges: Col/EPI Col/ADP Could replace the bleeding time Francis J., Francis, D., Larson, L., Helms, E. & Garcia, M. (1999). Can the Platelet Function Analyzer (PFA)-100 test substitute for the template bleeding time in routine clinical practice? Platlets, 10(2-3), 132-6. Assesses platelet dysfunction due to: ASA-like platelet defects congenital platelet defects (vWD) PFA 100 Platelet aggregation/plug 800 µL blood Filter with Epinephrine or ADP Once started, a timer begins. When platelets have plugged aperature, the final time is reported as “closure time” Interpretation Col/EPI True platelet defect (vWD, etc) Aspirin-like defect (ASA) Col/ADP +++ +++ (ex. >300) +++ normal Platelet Aggregation A photo optical instrument or instruments using electrical currents are used to detect aggregation of platelets in platelet rich plasma or whole blood, respectively PRP or whole blood is mixed with an aggregating agent and results are transmitted to a chart recorder Collagen, ADP, epinephrine, thrombin, serotonin, ristocetin Platelet aggregation curves http://www.practicalhaemostasis.com/Data%20Interpretation/Data%20Questions/data_interpret ation_platelet_function.html click here for practice cases Aggregation Disorders Glanzmann’s Thrombasthenia Bernard-Soulier Syndrome ADP Abnormal Normal Thrombin Abnormal Abnormal Collagen Abnormal Normal Epinephrine Abnormal Normal Ristocetin Normal Abnormal vWF Normal Abnormal Lab Findings Platelet Aggregation QUESTION Heparin Induced Thrombocytopenia (HIT) is an immune mediated complication associated with heparin therapy. Antibodies are produced against: ACLA PF4 AT B2GP1 QUESTION A bleeding time is used to evaluate the activity of: Platelets Prothrombin Labile factor Factor XIII QUESTION A patient has been taking aspirin regularly for arthritic pain. Which one of the following tests is most likely to be abnormal in this patient? Platelet count Template bleeding time Prothrombin time Activated partial thromboplastin time QUESTION Biological assays for antithrombin III (ATIII) are based on the inhibition of: Factor VIII Heparin Serine proteases Anti-ATIII globulin