DISEASES OF LOWER GI
1
•
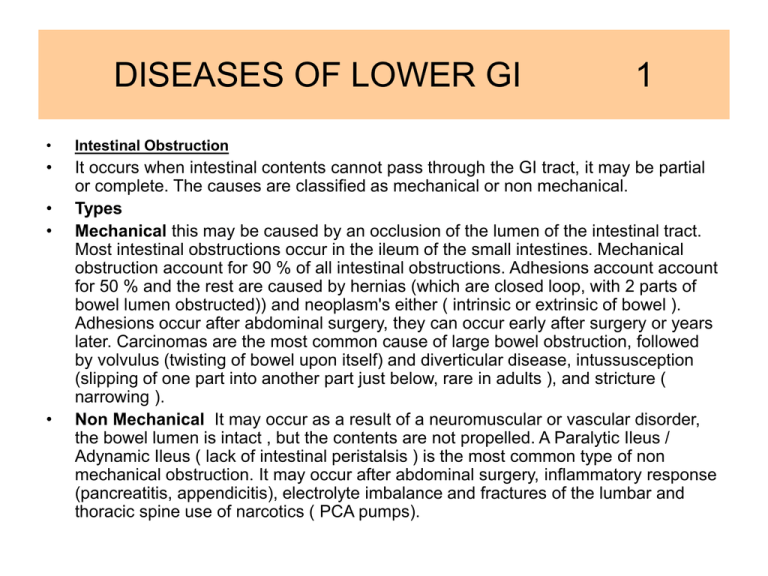
Intestinal Obstruction
•
It occurs when intestinal contents cannot pass through the GI tract, it may be partial
or complete. The causes are classified as mechanical or non mechanical.
Types
Mechanical this may be caused by an occlusion of the lumen of the intestinal tract.
Most intestinal obstructions occur in the ileum of the small intestines. Mechanical
obstruction account for 90 % of all intestinal obstructions. Adhesions account account
for 50 % and the rest are caused by hernias (which are closed loop, with 2 parts of
bowel lumen obstructed)) and neoplasm's either ( intrinsic or extrinsic of bowel ).
Adhesions occur after abdominal surgery, they can occur early after surgery or years
later. Carcinomas are the most common cause of large bowel obstruction, followed
by volvulus (twisting of bowel upon itself) and diverticular disease, intussusception
(slipping of one part into another part just below, rare in adults ), and stricture (
narrowing ).
Non Mechanical It may occur as a result of a neuromuscular or vascular disorder,
the bowel lumen is intact , but the contents are not propelled. A Paralytic Ileus /
Adynamic Ileus ( lack of intestinal peristalsis ) is the most common type of non
mechanical obstruction. It may occur after abdominal surgery, inflammatory response
(pancreatitis, appendicitis), electrolyte imbalance and fractures of the lumbar and
thoracic spine use of narcotics ( PCA pumps).
•
•
•
DISEASES OF LOWER GI
•
•
•
•
2
A incarcerated hernia (constricted) and volvolus can cause a strangulated
obstruction, causing the bowel to be obstructed and the blood supply to be affected
portion is compromised.
Pathophysiology
Normally 6-8Lof fluid enter small intestine daily, most of it is reabsorbed by the time it
reaches the colon. 75 % of intestinal gas is swallowed. Fluids, gas and intestinal
contents accumulate proximal to the obstruction, this causes distention, causing
distal bowel to collapse. This distention reduces absorption of fluids and stimulate
intestinal secretions. As pressure increases so does the pressure in the lumen of the
bowel. This increased pressure leads to increased capillary permeability and
extravasation of fluids and electrolytes into the peritoneal cavity ( causing perforation
). Edema, congestion and necrosis from impaired blood flow with possible rupture of
the bowel may occur. The retention of fluids in the intestines and peritoneal cavity can
lead to a reduction in circulating blood volume resulting in hypotension and
hypovolemic shock.
The location of the obstruction determines the extent of fluid, electrolyte, and acid
base balances. If the obstruction is high in pylorus, metabolic alkalosis may occur
from loss of HCL from stomach through vomiting and NG suction. When the
obstruction is in the small bowel, dehydration occurs quickly. Dehydration and
electrolyte imbalances do not occur early in large bowel obstruction.
DISEASES OF LOWER GI
•
•
•
•
•
•
•
•
•
•
•
•
3
Reverse peristalsis occurs in late bowel obstruction, causing the person to vomit fecal
material. Gangrene can develop following strangulation.
Manifestations vary depending on location. N/V, abd. Pain, distention,inability to pass
flatus, constipation. In mechanical obs. Pain comes and goes in waves, have
hyperactive bowels early. . Visible peristaltic waves may be seen in distended loops.
Later on bowel sounds are absent. They will also present signs from other conditions
that occur as a result of this obs. Large bowel obs. They have high pitched, tinkling
bowel sounds with gurgles, abd. is distended
MANIFESTATIONS
SMALL INTESTINE LARGE INTESTINE
ONSET
RAPID
GRADUAL
Vomiting
Frequent / Copious amts.
Rare late vomit fecal
Projectile With bile
material.
Pain
Colicky, cramplike,
Low grade cramping
intermittent
abdominal pain
Bowel move
Feces for a short
Constipation
time
Abdominal
Minimally increased
Greatly increased
distention
DISEASES OF LOWER GI
•
•
•
•
•
•
•
4
Complications
Hypovolemia, hypovolemic shock with multiple organs dysfunction. Renal
insufficiency from hypovolemia. Pulmonary problems due to abd. Distention. ,
strangulation (from volvulus impairing blood supply), gangrene, perforation, fluid and
electrolytes.
DIAGNOSTICS – X-RAY Abdominal (show presence of gas & fluid in intestines), Bun
( may be elevated due to dehydration ) , CT SCAN, , Serum Amylase, Electrolyte
(potassium & chloride lost in vomitus), Arterial bloods ( predicts alkalosis or acidosis),
an elevated WBC may indicate strangulation or perforation, elevated HCT may
indicate hemoconcentration. Decreased HCT &HGB indicates bleeding.
Barium enemas help locate large intestinal obs. however if perforation is suspected
this won’t be done. A Sigmoidoscopy or colonoscopy provides direct visualization of
the obs. In colon.
Management
Decompression of intestines, by removing gas, fluid, and correction of fluid and
electrolyte balance. NG tubes are used to decompress, and prior to surgery to empty
the stomach and relieve distention. .
A sigmoidoscopy may reduce a sigmoid vovulus of the. Colon decompression
catheters may be passed through a partially obs. Area, via colonscope to
decompress the bowel prior to surgery.
A. Adhesions B. Incaarcerated hernia C. Tumor
D. Intussusception E. Volvulus
5
DISEASES OF LOWER GI
•
•
•
•
•
6
Management Cont’d
IV fluids with Na & K, to correct fluid & electrolyte balance from vomiting (NS,
RL). TPN for nutritional deficiencies, to improve patient’s nutritional status prior
to surgery and to promote post- op healing. Blood volume expanders if
strangulation has occurred. Broad spectrum antibiotic. Most mechanical obs. Are
treated surgically, they may involve resecting the obstructed portion and
anastomosing the remaining healthy bowel. A partial colectomy, colostomy or
ileostomy may be done for extensive involvement or necrosis is present. A
laparotomy for inspection and removal of gangrenous tissue and adhesions can
be removed. During the assessment determine location, duration, intensity,
frequency of pain, is there abdominal rigidity. Onset, frequency, color, odor and
amt. of vomitus. Bowel , whether they pass flatus, can you hear bowel sounds,
is there a palpable mass.
Nursing –
Health history previous history of obs., hernias, abdominal surgery, bowel
diseases, medications.
Strict . I&O, observe for S/S of dehydration., Monitor character of N/G drainage,
glucose monitoring. Skin care, check stoma,
DISEASES OF LOWER GI
•
•
•
•
7
Upper obs. There may be metabolic alkalosis, Lower obs, they may have metabolic
acidosis. Analgesics are held until obs. is located because they may mask other
signs &symptoms, and decrease intestinal motility. CVP monitoring, Measure Output
indicates renal function.Measure abd. Girth. Monitor cardiac status, VS.
Care for NG tube, mouth care, nasal care, use water soluble lubricant for lips and
nares. Check patency, when NG is to be D/C, it is clamped 1 hour out of every 3 hrs,
or 3 hrs. out of every 4.
Elevate HOB helps with breathing, splint abdomen when coughing, use inspirometer.
Potassium levels play an important role, it is responsible for smooth muscle
contraction in GI causing low potassium causes decreased peristalsis.
DISEASES OF LOWER GI
•
•
•
8
Diverticular Disease
A diverticulum is a saccular dilation or outpouching of the mucosa through circular
smooth muscle of intestinal wall. Diverticular disease occurs in 2 forms, diverticulosis,
( a multiple non inflamed diverticula ). In non inflamed the person is most often free of
symptoms, but may have some abd. discomfort. Diverticulitis is an inflammation of
the diverticula ( caused by retention of stool and bacteria in diverticulum forming a
hard mass ), inflammation of diverticulum will spread to surrounding areas in the
intestine . Diverticula may occur any place in the GI tract except the rectum. Most
often it is present in the large intestine in the sigmoid area. There is a high incidence
in the Western population, that consumes diets low in fiber high in refined CHO. It
affects both sexes equally. The incidence for developing it increases with age.
Contributing factors are, diets highly refined (purified) and fiber deficient, decreased
activity levels, postponement of defecation. Decreased blood supply and nutrition.
Lack of dietary fiber slows transit time and more water is absorbed from stool, making
it difficult to pass through the lumen. This decreased bulk combined with a narrowed
lumen causes high intraluminal pressures, leading to formation of diverticula. Muscle
in the area of the diverticula will hypertrophy, this causes a narrowing of bowel lumen,
increasing pressure in lumen.
DISEASES OF LOWER GI
•
•
•
•
9
Deficient fiber and lack of fecal bulk contributes to muscle hypertrophy and
narrowing of bowel. Contraction of muscle in response to stimuli such as meals may
occlude lumen causing more increased lumen pressure. This high pressure causes
mucosa to herniated through muscle wall forming diverticulum. The areas where
nutrient blood vessels penetrate muscle layer are most common sites for diverticula
to develop
Manifestations
Diverticulosis- most people are asymptomatic, those with symptoms have crampy
abdominal pain in the LLQ, usually relieved by passing flatus or BM. They alternate
with constipation and diarrhea. Usually they progress to diverticulitis. As it progresses
they develop narrow stools (decrease in caliber), occult bleeding, weakness and
fatigue. A complication may be hemorrhage and diverticulitis.
Diverticulitis- undigested food and bacteria collect in the diverticula, forming a hard
mass which will impair the mucosal blood supply causing perforation, abdominal pain
localized over area involved, tender LLQ mass, fever, chills, nausea, anorexia,
elevated WBC, abdominal tenderness.They may experience constipation or
frequency of defecation. Complication, peritonitis,bowel obs., hemorrhage
manifested by ( hematochezia-maroon stools) , scarring and fibrosis of bowel wall
narrowing bowel lumen. Fistulas form ( colovesical) causing urinary tract infections.
Perforation of fistula into intestines, ureters, vagina, abdominal wall,leads to bleeding.
10
11
DISEASES OF LOWER GI
12
•
Diagnostics
•
History & physical, WBC, CBC, Guaic stools, blood cultures, barium enema,
Abdominal X-Ray, CT scan with or without contrast, sigmoid or colonoscopy( not
done in acute diverticulitis, can cause perforation).
Management
High fiber diet low cost fiber supplement (bran), bulk laxatives psyllium hydrophilic
mucilloid (metamucil), anticholinergic dicyclomine (bentyl ) and donnatal, relieve
spasms. Broad spectrum antibiotics metronidazole (flagyl), ciprofloxacin (cipro),
trimethoprim-sulfamethoxazole (septra-bactrim), severe attacks may necessitate the
need for hospitalization, then they receive IV antibiotics cephalosporins such as
mefoxin (cefoxitin), piperacillin-taxobactam(Zosyn). Talwin (pentazocine) for pain
causes less increase in colonic pressure than morphine and demerol. Stool softeners
colace,
Increase fluids, avoid increased intrabdominal pressure (lifting, bending, vomiting,
tight restrictive clothing) NPO, rest bowel, Diet- avoid foods with seeds (popcorn,
berries, caraway seeeds, nuts), control hemorrhage, colostomy care and skin care.
I&O
Surgery
Bowel resection, temporary colostomy until inflammation subsides. After 2-3 months
then they close and reconnect bowels.
•
•
•
•
•
DISEASES OF LOWER GI
•
•
•
•
13
Hemorrhoids
The anus and anal canal contains superficial venous plexuses, when pressure on the
veins increase or venous return is impeded, they develop varicies, which become
weak and distended. They occur when venous return from the anal canal is impaired.
Precipitating factors, straining to defecate in sitting or squatting position increases
venous pressure, Pregnancy increases intraabdominal pressure, raising venous
pressure, prolong sitting, obesity, chronic constipation, low fiber diets, they think it can
occur from shearing force during defecation, this force damages supporting
structures leading to dilatation of veins. Blood flow through veins are impaired. Clots
form in the vein causing bleeding with defecation.
They may be internal above internal sphincter, Internal rarely cause pain, usually they
present with bleeding. Bleeding is bright red and varies in quantity. Recurring
bleeding can lead to anemia, they also pass mucous, have feeling of incomplete
evacuation of stool
External occurs outside the external sphincter, bleeding is rare, anal irritation, feeling
of pressure and difficulty cleaning anal area are manifestations. Hemorrhoids are
reddish blue, if blood clots in external hemorrhoid it becomes inflamed and
painful.itching , burning
DISEASES OF LOWER GI
•
•
•
•
•
•
•
•
14
As hemorrhoids enlarge they can prolaspe or protrude through anus. Initially they
prolapse with defecation then they regress back into canal, as time goes on they may
have to manually replace them.Normal hemorrhoids are not painful, pain is
associated with ulcerations and thrombosis. Prolapse hemorrhoids can strangulate as
a result of edema, this leads to thrombosis. Then they have pain. Thrombosis is a
hematoma beneath the skin which usually resolve spontaneously.
Diagnostic
Ext. ones Seen on examination, they are asked to do valsalva to detect prolapse.
Anoscopic exam. used to detect internal hemorrhoids, stool for guaic, sigmoidoscopy
Management
High fiber diet, increase fluids, increase stool bulk, reduce straining, Metamucil,
colace, preparation H suppository, local anesthetic and astringent effect (Nupercaine)
reduces discomfort and irritation of surrounding tissue. Witch hazel shrinks mucous
membrane. Sitz bath, bed rest, no straining
Sclerotheraphy inject chemical irritant into tissue surrounding hemorrhoid,this
reduces inflammation, fibrosis and scarring, also used for bleeding. Another is rubber
band ligation, tie band around await for tissue necrossing and sloughing away 7-10
days.
Hemorrhoidectomy-surgically excised with use of laser , Post op they have packing
for 24 hours. Post op they have pain, spasms, given sitz bath, rubber donut, dischg
after 1st BM
15
.
Internal Hemorrhoid
16
DISEASES OF LOWER GI
•
•
•
17
Crohn’s Disease called regional enteritis chronic inflammatory disease, with
unknown origin, It can affect any part of GI tract from mouth to anus. It occurs most
during ages 15-30 yrs. If it occurs in older persons there is a high mortality. There is a
higher incidence in women. It occurs most in Jewish upper class. It occurs as shallow
ulcer, then it can regress or progress to involve other layers of the intestines. There is
an inflammation of segments of the GI tract. It is most commonly seen in the terminal
end of the ileum, and ascending colon. It involves all layers of the bowel wall. It skips
segments so you have normal bowel separating abnormal. The ulcerations are deep,
and penetrates inflamed edematous mucosa. Thickening of bowel wall occurs with
narrowing of the lumen.It resembles cobblestone. And the development of strictures,
and fistulas, that communicate with other loops of bowel, skin, rectum, bladder and
vagina.The inflammation edema, and fibrosis leads to obstruction, abscess.
Malabsorption and malnutrition developes the ulcers prevent absorption of nutrients.
When the ileum and jejunum are involved absorption of many nutrients are impaired.
In the terminal ileum there is Vit B12 malabsorption, and bile salts resorption.
Eventually there is protein loss , slow blood loss and anemia develops.
Crohns’
18
19
Prolaspe Rectum
20
Rectal Irritation and Small Fissure
21
DISEASES OF LOWER GI
•
•
•
•
•
•
22
Manifestation
Continuous episodic diarrhea, stools are liquid or semiformed.Abdominal
pain and tenderness.Pain is in RLQ and is relieved with defecating. Mass
can be felt RLQ. Fever, fatigue, malaise, weight loss, anemia, anorectal
fissures, ulcers, fistulas, and abscesses N/V epigastric pain If fistula cause
abscess they have chills ,fever, tender abd. Mass, and leukocytosis.
Perforation of bowel, massive hemorrhage is rare. It puts at risk for Cancer
of small bowel.
Complications
Narrowing of lumen, fistulas, perforation, intrabdominal abscesses,
peritonitis, impaired absorption, causing deficiency in fat soluble vits.
Arthritis, liver disease, cholelithiasis, uveitis (inflammation of Eye) caused by
local or systemic bacterial infections, kidney stones, intestinal obstruction,
N/V, if bowel fistula UTI,
Diagnostics
Colonoscopy, can perforate bowel with procedure. Barium, UGI series, stool
culture, stool for occult blood CBC, serum albumin, folic acid
DISEASES OF LOWER GI
•
•
•
•
•
•
•
•
•
23
Management
Sulfasalazine (azulfidine) a sulfonamide antibiotic, assess for allergies causes skin
rashes, assess Bun,Creat, UA, CBC,
Corticosteroids ( monitor glucose), Mercaptopurine (purinethol) azathioprine (6-mp)
immunosuppressive agent (helps withdraw from steroids) , flaggy or cipro
Antidiarrheal (loperamide) not given in acute attack causes toxic dilatation of colon.
Diet,
TPN, no milk products, increase fiber, NPO to rest bowel., elemental diet low
residue, roughage and fat
Surgery
Total colectomy- removing entire disease portion.of colon and rectum, with ileal
pouch and anal anastamosis. In anal canal, with a temporary ileostomy to allow for
healing, when closed have 6-8 weeks obesity and advanced age this is not done do
permanent ileostomy.
Kock ileostomy intraabdominal reservoir with nipple valve stoma formed, stool
collects in pouch, catheter inserted into valve to drain pouch.
Proctocolectomy with ileostomy
24
Kock ileostomy (continent ileostomy)
25
Ileoanal Reservoir
26
Ileoanal Anastomosis
27
DISEASES OF LOWER GI
•
•
•
•
28
ULCERATIVE COLITIS
It is an inflammation and ulceration of the colon and rectum. The most common type
is chronic intermittent colitis or recurrent colitis. It can occur at any age but peaks
between age 15-25 yrs. Both sexes are equally affected, and it is seen more often in
the Jewish population. The colon wall is made of three layers; mucosa, submucosal,
muscularis externa, and pouches (haustra) which allow the c colon to contract. The
inflammation is widespread and it involves the mucosa and submucosa. The onset is
slow, with attacks that last approx. 1-3 months.
Etiology
The condition usually begins in the rectum and sigmoid, it moves up the colon in a
continuous pattern, stopping at the ileocecal junction. There are periods of remission
and exacerbation. In the area of the colon that is affected, there is an increase blood
supply and edema. After a period of time abscesses will develop in the intestinal
glands (crypts of Lieberkuhn), as time goes on the abscesses will break through the
crypts into the submucosa leaving ulcerations. These ulcerations destroy the mucosal
epithelium, causing bleeding and diarrhea and necrosis. With a decrease in the
mucosal surface are there will be a decrease in absorption thereby causing a loss of
fluids and electrolytes.
Ulcerative Colitis
29
DISEASES OF LOWER GI
•
•
•
•
•
•
30
As cells breakdown protein is lost through stool. The areas in the inflamed mucosa
form pseudopolyps, which look like tonguelike projections into bowel lumen.
Granulation of tissue occurs and the mucosal musculature thickens and causes
shortening of the colon.
MANIFESTATIONS
Diarrhea 6-10 daily, blood and mucus in stools, nocturnal diarrhea, anemia,
hypovolemia, malnutrition, fecal urgency with tenesmus (spasms and anal
contraction, with involuntary straining to void or defecate). LLQ cramping which is
relieved with defecation the pain may be mild or severe associated with perforation ,
fatigue, anorexia and weakness, dehydration. Other manifestations include systemic
effects arthritis, skin lesions, mucous membrane lesions, inflammation of vascular
layer of eye which may involve the sclera and cornea, thromboemboli.
COMPLICATIONS
Intestinal- hemorrhage, strictures, perforation, toxic megacolon (acute dilatation and
paralysis of the colon that might progress to rupture)manifestation of megacolon
fever, tachycardia, hypotension,dehydration, abd. Tenderness, colonic dilation.
Extraintestinal- complication directly related to colitis malabsorption, or complications
related to disturbance in immune system, joint pain, skin, mouth, and eyes, anemia,
leukocytosis.
DISEASES OF LOWER GI
•
•
•
•
•
•
•
31
DIAGNOSTICS
CBC, electrolytes, serum protein, elevated WBC (indicates perforation),
hypoalbuminema ( due to loss of protein in stool ), stool for guiac, stool cultures to
R/O infectious causes.
Sigmoidoscopy and Colonoscopy (visualize entire colon) helps identify extent of
inflammation, biopsy (help with a more definitive diagnosis).
MANAGEMENT
Drug Therapy1. Sulfasalazine (Azulfidine) a sulfonamide antibiotic it is poorly absorbed by the GI
tract but it has a topical affect on the intestinal mucosa, assess for allergies causes
skin rashes. It is effective in maintaining remission, once in remission the dose will be
reduce however they may remain on a maintenance dose of the drug for up till 1 year.
The active anti inflammatory ingredient in sulfasalazine is (5 aminosalicylic acid) it
inhibits prostaglandin production in the bowel, thereby reducing inflammation, it is
available in a preparation that does not contain sulfa (Olsalazine or
Mesalamine).causes N/D and flatulence. Assess renal function test (Creat, Bun, UA),
liver function test and CBC.
The drug increases sensitivity to sun need (sun block), monitor urinary output. If
taking oral contraceptives it may interfere with it’s effectiveness, will need and
alternative while on drug. Medications can be given Orally, or by retention enema,
DISEASES OF LOWER GI
•
•
•
32
2. Corticosteroids- ( Prednisone or Prednisolone), good choice for
management when there is no systemic manifestations. If remission not
achieved then the patient is hospitalized and treated with IV steroids (Solu
Medrol), bed rest with IV replacement of electrolytes. Monitor for signs of
Cushing syndrome, hypertension hirsutism and mood swings. If the rectum
is the area of involvement steroid enemas can be given.
3. Immunosuppressive drugs- (6 mercaptopurine/ 6 MP) (Imuran) Used
when the patient fails to respond to all other meds. And before surgery is
considered, these meds help withdraw from steroids. SE are bone marrow
depression, and increased risk for infection. Patient’s taking this drug are
encouraged to drink 1800-2400 cc of fluid to reduce the risk for
nephrotoxicity.Taken with food or milk to reduce gastric irritation.
4. Anti diarrheal – Lomotil (diphenoxylate), Imodium (loperamide), these
drugs slow gastric motility causing a decrease in diarrhea, they are held in
acute attacks cause toxic dilatation of colon.
Colostomies
33
DISEASES OF LOWER GI
•
•
•
•
•
•
•
•
34
Surgery- This is done when the patient fails to respond to all other form of treatment,
and when the are in a debilitating state
1. Total Proctocolectomy with permanent IleostomyRemoval of colon, rectum and anus with closure at anus, then a stoma is created with
terminal end of ileum. Few problems with this procedure.
2. Total Proctocolectomy with continent Ileostomy (kock pouch). Patient does not
need external pouch. The stoma may be coved if there is mucus drainage. They take
distal end of ileum slit it and fold into a one way valve, the distal end of ileum is made
into a internal pouch, the pouch is a reservoir and has to be drained at regular
intervals by inserting a catheter. A one way valve is created at the internal end of
ileum. The valve closes when the pouch fills with feces. There are complications,
inflammation of pouch, fistulas may develop.
3. Total Colectomy and Ileal Anal Reservoir
Removal of entire colon with ileoanal anastomosis and formation of an ileal anal
reservoir. This procedure is done in two parts, over 2 months apart, first they do
colectomy, with temporary ileostomy and reconstruction of ileal reservoir with ileoanal
anastomosis , the second surgery is closure of ileostomy with the functioning
reservoir. Once adaptation occurs the person can control and have less number of
BM’s in 24 hrs
Post –Op same care as for crohns- Stoma care, skin care, Respiratory assess, IV’S,
I&O
,
DISEASES OF LOWER GI
•
35
Dietary- Diets vary from eliminating all milk products, increased fiber, high protein,
high caloric, food may be withheld to rest bowel. TPN, or nasal gastric feeding,
supplemental feeding(ensure), Vitamin & iron supplements. Foods that increase GI
motility are held (cold food, whole wheat bread, nuts, raw fish), Zinc deficiency occurs
with diarrhea so they need supplements.
DISEASES OF LOWER GI
•
•
•
•
36
Cancer of the Colon
Colon cancer is the third most common cancer in the USA, over 50,000 have died as
a result. It occurs most often at age 50 yrs, and men and women both develop the
disease equally. Most cases are diagnosed late, decreasing the chance of survival.
The etiology is unknown,but there are risk factors that have been identified. Genetic,
IBD (inflammatory bowel), diet, people from lower socioeconomic , eat foods high in
calories, meat protein, and fats.
Most all colorectal malignancies are adenocarcinomas that begin as a adenomatous
polyp, they are most often found in the rectum and sigmoid colon. They usually go
undetected and without symptoms , by the time the become symptomatic it has
metastasized to other adjacent structures, spreading through the intestine wall into
the lymphatic system, 5 – 15 yrs of growth may occur before it is diagnosed.The
largest number of cases occurs on the right side of the intestines. .
Manifestations- left side colon Ca. rectal bleeding, alternating diarrhea with
constipation, change in stool caliber (narrow, rlbbonlike), and feeling of incomplete
evacuation. Right sided, vague abdominal discomfort or crampy, colicky abd. Pain ,
iron deficiency anemia and occult bleeding, weakness and fatigue.
DISEASES OF LOWER GI
•
•
•
•
•
•
•
37
Complications Bowel obstruction due to narrowing of bowel lumen, Perforation of
bowel wall, Metastasis
Diagnostics CBC (detect anemia), Stool for occult blood ( avoid red meat, & NSAID)
give false pos., CEA, LFT’s, Sigmoidoscopy / Colonoscopy, CXR (detect METS), CT,
MRI, biopsy, Barium enema, US,
Surgery
Resection of tumor, adjacent colon, lymph nodes
Abdominalperineal resection with colostomy, different colostomy procedures are used
depending on location/. Laser photocoagulation
Chemo / Radiation
Chemo ordered when lymph nodes are involved use of combination drugs