Changes in renal physiology
advertisement

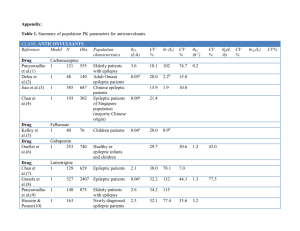
Pharmacokinetics, Pregnancyinduced Physiologic Alterations and Predicaments in Practice Ruston S. Taylor, Pharm.D., BCPS, BCNSP Clinical Pharmacy Specialist Texas Children’s Hospital—The Center Objectives Discuss clinical implications during pregnancy caused by limitations of currently available pharmacokinetic data Identify physiologic changes along the continuum of pregnancy in specific organ systems Relate alterations in various organ systems to influence on pharmacokinetic principles ??Pharmacokinetics?? First, what do we know about pharmacokinetics in the pregnant patient?? Pharmacokinetics: Limitations to current knowledge Specific data for Vd and Cls in pregnancy for individual drugs is limited due to ethical and practical considerations Pharmacokinetic clinical trials exclude pregnant women, due to FDA moratorium Pharmacokinetic data that does exist in pregnancy comes from small sample size studies and incorporates different gestation ages Comparator groups are often composed of non-pregnant women, adult males, and same subject 6-8 weeks postpartum as controls Pharmacokinetics: Limitations to current knowledge Limited pharmacokinetic data available for the following: Anticonvulsants Antihypertensives Antibacterials Analgesics All pharmacologic classes listed have lack of consistency between studies and individuals Pharmacokinetics: Limited data for anticonvulsants Anti-epileptic drugs (AED) are the most studied therapeutic category of agents in pregnancy Plasma concentrations across studied AEDs, especially in the later stages of gestation Decrease in plasma concentrations due to clearance and lower concentrations of binding proteins affect the following: Carbamazepine Phenytoin Phenobarbital Pharmacokinetics: Decreased anticonvulsant plasma concentrations Most anticonvulsants exhibit high albumin binding However, the unbound concentration of “free drug” is pharmacologically active Special attention should be given when interpreting the results of plasma concentrations to guide therapeutic efficacy as most labs report total plasma concentration (bound and unbound) A fall in plasma concentrations does not reflect a fall in free drug Ideally, free drug concentrations should be monitored Pharmacokinetics: Limited data with antihypertensives Beta-blockers (e.g. labetalol): Exhibit a shorter t1/2 in pregnant women, suggesting the need for more frequent doses Calcium channel blockers (e.g. nifedipine): Exhibit faster elimination However, administration frequencies will continue to be ultimately based on patient response Pharmacokinetics: Limited data with antibacterials Plasma concentrations of β-lactam antibiotics are well known to correlate with response of bacterial infections and are unaltered during pregnancy Ampicillin exhibits increased clearance and reduction in plasma concentrations during pregnancy Pharmacokinetics: Extremely limited data with analgesics There is no consistent evidence detailing the pharmacokinetics of analgesics in pregnancy (even studies of the same drug) No management guidance can be formed concerning dosing schedule However, management of pain will continue to be based on pain score trends which may necessitate increases in medication administration Pharmacokinetic DISCLAIMER Vast and complex physiologic changes during pregnancy have significant effects on drug disposition Understanding physiologic changes during the continuum of pregnancy can help guide drug dosing in various stages Wide interpatient and intrapatient variability necessitate monitoring serum drug levels when indicated ??Physiologic changes?? • Identify physiologic changes along the continuum of pregnancy in specific organ systems Why is pregnancy so HARD? Cardiovascular system: Pregnancy-associated changes Changes in maternal hemodynamic variables: Blood volume Blood pressure (BP) Heart rate (HR) Stroke volume (SV) Cardiac output (CO) Systemic vascular resistance (SVR) Cardiovascular system: Complicating variables Factors complicating management may include: Maternal age Multifetal pregnancy Gestational age Body build Labor (length and method of delivery) Regional anesthesia Blood loss Cardiovascular system: Blood volume changes McLennon CE, Thouin LG. Blood volume in pregnancy. Am J Obstet Gynecol 1948; 55:1189. Cardiovascular system: Pharmacokinetic changes due to blood volume Physiologic change Pharmacokinetic impact Volume expansion Decreased Cmax of drugs Enhanced clearance Decreased steady-state concentration Protein binding Decreased drug elimination occurs as drug is inhibited from hepatic and renal elimination Hypoalbuminemia Decreased sites for steroids, hormones, and drugs to bind Decreased binding capacity Larger unbound fraction of drug (free drug) More pharmacologic activity Cardiovascular system: Changes in blood pressure Progesterone effects Blood Pressure (BP) = Cardiac output (CO) x systemic vascular resistance (SVR) BP normally decreases by about 10% by the 7th week of pregnancy Cardiac output (CO) = heart rate (HR) x stroke volume (SV) Increases by 10 weeks’ gestation 30-50% increases seen by latter part of 2nd trimester Blood pressure is a reflection of the cardiovascular system’s ability to maintain perfusion to various organs (i.e. fetoplacental unit) Cardiovascular system: Increased cardiac output causes Renal blood flow Pulmonary blood flow Uterus • Increases by 30% • GFR increases by 30-50% • Increases by 30% • 50 ml/min at 10 weeks • 500 ml/min at term Genitourinary system: Changes in renal tract anatomy As blood volume increases, the kidney increases in length Dilation of collecting system occurs secondary to muscle relaxant effects of progesterone Obstruction to the collecting system can occur due to enlarging uterus Compressing the ureters causes urinary stasis Increased risk of pyelonephritis Genitourinary system: Changes in renal physiology Elevated estrogen levels early in pregnancy result in renin production Conversion of angiotensinogen to angiotensin I and II Causes increase in aldosterone Results in renal tubular sodium retention Genitourinary system: Changes in renal physiology Glomerular filtration rate (GFR) by 50% to a peak around 180 mL/min by end of 1st trimester Results in: blood urea nitrogen (BUN) and serum creatinine (SCr) levels > 0.8 mg/dL are indicators of abnormal function protein excretion considered normal Loss of glucose in the urine (glycosuria) is normal Predisposing factor for UTI Genitourinary system: Pharmacokinetic change in renal drug elimination As GFR by 50%, drugs excreted primarily unchanged in the urine are of concern: Penicillin Digoxin Lithium These drugs exhibit lower steady-state serum concentrations; however, dose alterations are generally not prescribed as data is lacking or conflicting Gastrointestinal (GI) system: Changes in GI physiology Progesterone-mediated smooth muscle relaxant effects during pregnancy may the following: Lower esophageal sphincter tone = GERD and heartburn Gastric and small bowel motility Prolonged gastric emptying and extended intestinal transit times Decreased gastric motility Increased time in large intestine Increased water absorption Gastrointestinal (GI) system: Pharmacokinetic changes in GI The following factors affect the gastrointestinal absorption of drugs: Drug formulation Food composition Chemical composition pH of the intestinal secretions Gastric emptying time Intestinal motility Blood flow Gastrointestinal (GI) system: Changes in metabolic activity Enzyme Pathway Change in Activity Drugs of interest Comments CYP1A2 Decreased Theophylline, clozapine, ondansetron, propranolol, cyclobenzaprine Caffeine half-life also prolonged CYP2A6 Increased Nicotine, cotinine Cotinine is active metabolite of nicotine; may have decreased effect of nicotine gum CYP2C9 Increased Phenytoin, glyburide Monitoring of phenytoin concentration indicated CYP2D6 Increased Many β-blockers, including metoprolol; many TCAs and SSRI, codeine Decreased concentration of SSRI documented and may be associated with recurring symptoms of depression Gastrointestinal (GI) system: Changes in drug metabolism in pregnancy Enzyme Pathway Change in Activity Drugs of interest Comments CYP3A4 Increased Most calcium channel blockers, including nifedipine; most benzodiazepines; most HIV protease inhibitors; most non-sedating antihistamines; methadone May have withdrawal symptoms in patients on methadone maintenance UGT1A1 Increased Acetaminophen Unknown significance UGT1A4 Increased Lamotrigine Significant decrease in serum lamotrigine concentrations; increase in seizure activity unless monitoring and dose adjustment occurs UGT2B7 Increased Lorazepam Unknown significance Gastrointestinal (GI) system: Pharmacokinetic changes in hepatic elimination The cholestatic effects of progesterone on the gall bladder interfere with the clearance of biliary secreted drugs (e.g. rifampin) As illustrated previously, almost all pharmacokinetic elimination mechanisms via the CYP and UGT systems increase during pregnancy However, hepatic elimination cannot be quantified as phenotypic expressions depend on the genetic make-up which varies greatly between individuals Endocrine system: Changes in the pancreas β-cells undergo hyperplasia during pregnancy This results in increased insulin secretion Insulin hypersecretion results in hypoglycemia seen in early pregnancy Peripheral resistance to insulin is a result of production of insulin antagonists, human placental lactogen Placental insulin antagonists result in normal postprandial hyperglycemia Placental-Fetal Compartment Placenta acts as a permeable barrier between the maternal and fetal blood circulations Functions to transport oxygen and nutrients from the mother to fetus, while also providing waste exchange from the fetus to the mother Drugs cross mainly via passive diffusion Factors that determine the ability of a compound to cross the placenta include: pKa, lipid solubility, and molecular size Physiologic conclusions: Physiologic adaptations occur at different times and to different degrees depending on the organ system and individual Maternal ability to adapt may depend on preexisting variables: Maternal age Multiple gestation Ethnicity Genetic factors Physiologic conclusions: Maternal ability to adapt may depend on pregnancy-associated factors: Gestational age Labor Intrapartum blood loss A better understanding of normal physiologic adaptations of pregnancy gives practitioners the ability to manage pregnancy-associated complications References: Belfort Michael, comp. Critical Care Obstetrics. 5th ed. Chichester: Blackwell, 2010. Briggs GG, Nageotte, M. Diseases, Complications, and Drug Therapy in Obstetrics. Bethesda: ASHP, 2009. Dawes M, Chowienczyk P. Pharmacokinetics in Pregnancy. Best Practice & Research Clinical Obstetrics and Gynaecology. 2001; 15(6): 819-826. Koren G. Pharmacokinetics in Pregnancy; Clinical significance. J Popul Ther Clin Pharmacol. 2011; 18(3): e523-e527. Little, B. Pharmacokinetics During Pregnancy: Evidence-Based Maternal Dose Formulation. Obstetrics and Gynecology. 1999 May;90(5): 858-868. Review. Loebstein R, Lalkin A, and Koren G. Pharmacokinetic Changes During Pregnancy and Their Clinical Relevance. Clin Pharmacokinet. 1997; 33(5): 328-343.