Wegener`s Granulomatosis
advertisement

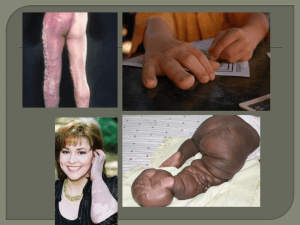
Clinical Pathological Conference 三軍總醫院 小兒科部 R2 田炯璽 / 洪志興 醫師 Present Illness A 15-year-old boy with history of allergic rhinitis had fever and epistaxis developed this March. (Two months before present) Bilateral markedly enlarged exudative tonsillitis was also present, which was improved after treatment with Amoxicillin-clavulanic acid (Augmentin). However, one week later, arthralgias developed in the ankles and subsequently in the knees and hands. Night sweating was noted, however, no joint swelling or erythema. Present Illness Soon, cough developed, and it was occasionally associated with thick, whitish, blood-streaked sputum and postnasal drip with bloody nasal discharge. The patient coughed frequently but appeared well. Past, Personal History A case of allergic rhinosiusitis. Suffered from paranasal sinusitis since 10 years old. Sinus surgery was performed at another hospital in this January. Pathological result revealed acute and chronic rhinosinusitis with stromal eosinophils. Laboratory Data CBC: WBC: 9000/ul Neutrophils: 63% Lymphocytes: 17% Monocytes: 8% Eosinophils: 11% (990/ul) Basophils: 1% HCT: 44% PLT: 391000/ul Biochemistry: No abnormalities including serum BUN, creatinine, AST, ALT, uric acid, LDH, and glucose levels. Laboratory Data ESR: 22 mm/hr (child: 4 ~ 20 mm/hr) ANA: negative Rheumatoid factor: negative Urine routine: Protein: (+) RBC: 2~4/ Hpf (30mg/dl) Radiological Findings Chest film: Bilateral ill-defined, rounded, patchy opacities, none of them larger than 2cm in diameters. No lymphadenopathy, no pleural effusion. CT of chest: Multiple ground-glass opacities throughout both lungs, some had a rounded shape, and some had a central radiolucency, a feature consistent with cavitation. Bronchoscopic Examination Normal airway with no abnormal secretion. Broncho-alveolar lavage: A few acid-fast bacilli. Cytology: negative for malignant cells. Microbiological Examinations Ordinary culture for lavage : negative Fungus culture for lavage : negative Legionelle culture for lavage : negative PPD test for the patient: negative. Hospital course After the examinations performed which was described previously, a regimen of isonizid, rifampin, and pyrazinamide was begun. Two weeks later, another CT scan of chest showed no change in the bilateral opacities and no new lesions. The examination of a stained sputum revealed no acid-fast bacilli. Then the anti-TB regimen was discontinued. Problems Major Problems Productive cough with blood-streaked sputum. (Hemoptysis?) Positive findings on chest film and chest CT scan. Bloody nasal discharge (Epistaxis) Eosinophilia Minor Problems Previous exudative tonsillitis Night sweating Arthralgias Elevated ESR Mild proteinuria, and RBC in urine. Acid-fast bacilli found in bronchoalveolar lavage History of allergic rhinosinusitis. Questions to be asked: Any specific contact history? Living on a farm or near a coal mine? Drug history? History of asthma? Any other positive findings of physical examinations? Skin rash or purpura? Hepatosplenomegaly? Other palpable lymphadenopathy? Any other examinations of immunology? Serum immunoglobulin level (especially IgE) ? Did ANCA test performed? Which form is predominant? cANCA or pANCA? Serum angiotensin-converting enzyme level? Hemoptysis The expectoration of blood or blood tinged sputum. Bleeding can occur from disruption of the pulmonary or bronchial vessels. First it must be determined if a child is truly experiencing hemoptysis, because blood from the nose or GI tract may appear similar to bleeding from the pulmonary system. The blood in hemoptysis is generally bright red and frothy, has an alkaline pH, may contain sputum, and may be accompanied by a cough. Differential Diagnosis of Hemoptysis Infection Tracheobronchitis Pneumonia Bacterial TB Fungal (e.g., aspergillosis) Parasitic Tracheostomy-related Bronchiectasis Cystic fibrosis Ciliary dyskinesia Immunodeficiency Foreign body Congenital heart disease (mainly with pulmonary vascular obstructive disease) Pulmonary arteriovenous malformation Trauma Alveolar hemorrhage syndromes Connective tissue disease/vasculitis (e.g., Goodpasture syndrome, Wegener granuloma) Primary pulmonary hemosiderosis (e.g., idiopathic, Heiner syndrome) Pulmonary thromboembolism Tumor Bronchial adenoma Metastasis DDx Flowchart of Hemoptysis DDx Flowchart of Hemoptysis Differential Diagnosis of Rhinorrhea/Nasal Congestion Seasonal allergic rhinitis Perennial allergic rhinitis Non-allergic rhinitis with eosinophilia Rhinitis medicamentosa Drugs/medication (prazosin, guanethidine, reserpine, cocaine) Mechanical/anatomic obstruction Cerebrospinal fluid rhinorrhea Pregnancy Hypothyroidism Wegener’s granulomatosis Sinusitis (viral, bacterial, fungal) Conditions that may mimic symptoms of rhinitis A. Structural/mechanical factors 1. Deviated septum/septal wall anomalies 2. Hypertrophic turbinates 3. Adenoidal hypertrophy 4. Foreign bodies 5. Nasal tumors a. Benign b. Malignant 6. Choanal atresia B. Inflammatory/immunologic 1. Wegener’s granulomatosis 2. Sarcoidosis 3. Midline granuloma 4. Systemic lupus erythematosus 5. Sjogren’s syndrome 6. Nasal polyposis C. Cerebrospinal fluid rhinorrhea Eosinophilia Eosinophils regulate and moderate mast-celldependent immediate hypersensitivity reactions Major function is as a cytotoxic cell, especially against helminthic infection. Absolute eosinophil count > 0.7 X 109/uL(700/ul) Eosinophilia Differential Diagnosis of Eosinophilia Allergic disorder Gastrointestinal disorder Infectious diseases Immunodificiency disease Allergic rhinitis Asthma Acute urticaria Hypersensitivity drug reaction Tissue-invasive helminth infection Pneumocystic carinii Toxoplasmosis Amebiasis Malaria Bronchopneumonia aspergillosis Coccidiodomycosis Scabies Malignant disorder Brain tumors Hodgkins disease T cell lymphoma AML Myeloproliferative disorder Inflammatory bowel disease Peritoneal dialysis Eosinophilic gastroenteritis Milk precipitin disease Hyper IgE syndrome Wiskott-Aldrich syndrome GVHD Pulmonary disease Löffler syndrome Eosinophilic leukemia Hypersensitivity pneumonitis Miscellaneous Thrombocytopenia with absent radii Vasculitis Histiocytosis with cutaneous involvement Hypereosinophilic syndrome Differential Diagnosis of Eosinophilia Differential Diagnosis of Night Sweats Pulmonary Tuberculosis The most specific confirmation of pulmonary tuberculosis is isolation of M. tuberculosis. Unfortunately, three consecutive morning gastric aspirates yield the organism in less than 50%. The culture yield from bronchoscopy is even lower. For most children, the presence of a positive tuberculin test, and abnormal chest radiograph consistent with tuberculosis, and a history of exposure is adequate proof that tuberculosis is present. Acid-fast Stain The Ziehl-Neelsen technique employed for identification of acid-fast bacteria. Acid-fast bacteria includes those cause tuberculosis, nontuberculosis mycobacteria infection, and Norcardia. Miliary Tuberculosis Erosion of a parenchymal focus of primary tuberculosis into blood or lymphatic vessels may result in dissemination of the bacilli and a miliary pattern. Usually complicates the primary infection, occurring within 2-6 months of the initial infection. Lesions are often larger and more numerous in the lungs, spleen, liver, and bone marrow. More often, the onset is insidious with early systemic signs, including anorexia, weight loss, and low-grade fever. Within several more weeks, the lungs may be filled with tubercles, and dyspnea, cough, rales, or wheezing occurs. The resolution of miliary TB is slow, even with proper treatment. The chest radiographic abnormalities may not resolve for many months. Miliary Tuberculosis Diagnosis of disseminated tuberculosis can be difficult. Early sputum or gastric aspirate cultures have a low sensitivity. The tuberculin skin test is non-reactive in up to 40% of patients. Biopsy of the liver or bone marrow with appropriate bacteriologic and histologic exams more often yields an early diagnosis. The most important clue is usually history of recent exposure to an adult with infectious tuberculosis. Treatment: the AAP and CDC have endorsed a regimen of 6 months of INH + RIF supplemented during the first two months by PZA as standard therapy of intrathoracic tuberculosis. Lymphoma (Non-Hodgkin) Lymphoblastic (T cell) lymphoma often presents as an intrathoracic tumor, usually a mediastinal mass, and is associated with dyspnea, chest pain, dysphagia, pleural effusion and superior vena cava syndrome. Cervical or axillary lymphadenopathy is present in up to 80% of patient at diagnosis. Hodgkin Disease Painless, firm, cervical or supraclavicular lymphadenopathy is the most common presenting sign. B symptoms: unexplained fever, weight loss, or night sweats. Pulmonary Metastasis Metastatic lesions are the most common forms of pulmonary malignancy in children. Primary process including Wilm’s tumor, osteogenic sarcoma, soft tissue sarcoma, and hepatoblastoma. Pulmonary tumors may present as fever, hemoptysis, wheezing, cough, pleural effusion, chest pain, dyspnea, recurrent pneumonia, or atelectasis. The prognosis varies and depends on the type of tumor involved. Histiocytosis Mainly referred as Langerhan’s cell histiocytosis. Bone lesions are the commonest manifestation(78%), second commonest: skin and mucous membrane (40%). Pulmonary involvement (25~30%): diffused cystic changes, nodular infiltrates, or extensive fibrosis can occur. The radiographic apearance may resemble miliary tuberculosis. Multi-system disease is frequent with patient’s presentation(40%), with single bone involvement mostly(53%). Pulmonary involvement is less frequently (6%). Painful bone lesion affecting hematopoeitically active bones are common. Löffler Syndrome (Eosinophilic Lung Diseases) Synonym: Simple pulmonary eosinophilia. Characterized by migrating pulmonary infiltrates accompanies by peripheral eosinophilia but minimal respiratory symptoms. The name “Löffler syndrome” is rarely used today. Chronic cough, intermittent fever, dyspnea, wheezing , and occasionally abdominal pain and weight loss. Patients present with nonspecific interstitial, alveolar or mixed pulmonary infiltrates, which tend to be bilateral and diffused. Often patients would have allergic reaction to parasites (c.g. heminthiasis), or drugs(c.g. ampicillin, ibuprofen). Extrinsic Allergic Alveolitis (Hypersensitivity Pneumonitis) Typically an adult disease, but have been reported in children. Caused by inhalation of a variety of organic antigens. The chronic form shows further progression of the granulomatous alveolitis resulting in interstitial fibrosis and honeycombing. Chest radiographs show coarse reticulonodular infiltrates and bronchiectasis. Patients with chronic disease may present as dyspnea, severe cough, weight loss, weakness, hypoxemia Lab findings: leukocytosis with neutrophilia; modest ESR elevation; serum immunoglobulins(IgM, IgA, IgG) are often elevated. Bronchoalveolar lavage fluid typically shows marked lymphocytosis and may also contains higher levels of immunoglobulins. Sarcoidosis Chronic, multi-system granulomatous disease of unknown cause. Manifestations: peripheral lymphadenopathy, arthritis, uveitis, skin rash, hepatosplenomegaly Acute fever, erythema nodosum, iritis, polyarthritis. Insidious including weight loss, cough, fatique, bone and joint pain, and anemia. Pulmonary involvement is variable: parenchymal infiltrates, miliary nodules, and hilar and paratracheal lymphadenopathy occurs. Typical symptoms with pulmonary involvement are dyspnea with exercise, and a dry cough. Hemoptysis is rare, as is production of sputum. Sarcoidosis Lab findings: elevated ESR; eosinophilia; hyperproteinemia, hypercalcemia, hypercalciuria. Serum angiotensin-converting enzyme level is elevated in about 2/3 of patients. Definite diagnosis: tissue biopsy (mostly lung ) – mononuclear cell granulomatous inflammatory process. Collegen Vascular Disease Primarily suggesting systemic lupus erythematosus, which consists a variety of clinical manifestation. Characterized by fever, weight loss, rash, hematologic abnormalities, arthritis, and involvement of heart, lung, CNS, and kidney. Restrictive interstitial lung disease is the commonest form of parenchymal involvement. The chest radiograph is usually normal but may present “platelike” atelectasis or interstitial fibrosis with “ honeycombing”. May also present the radiographic manifestation of vasculitis. It may be asymptomatic. Wegener’s Granulomatosis A necrotizing granulomatous angiitis affecting small and medium-size arteries and veins. The three major areas of involvement are the upper respiratory tract, the lung parenchyma, and the kidney. Upper airway: Acute and chronic sinusitis, often with secondary infection, occurs in over 80% of patients. Nasal ulcers, mucosal inflammation with nasal obstruction, septal perforation, and necrosis of nasal cartilage with “saddle nose”. Lower airway: Pulmonary infiltrates, pulmonary nodules (which may cavitate), and pulmonary hemorrhage. Renal: glomerulonephritis—80%, and half develop renal insufficiency. Wegener’s Granulomatosis Musculoskeletal: myalgias and arthralgias in 70% of patients, which a third develop a true nondeforming, nonerosive arthritis. Cutaneous: palpable purpura, cutaneous ulcers, pyoderma gangrenosum, and Raynaud’s phenomenon. Neurologic: Mononeuritis multiplex, peripheral symmetric polyneuropathy, cranial neuropathy, infarction, subdural or subarachinoid hemorhage, seizures, or cerebritis. GI tract: abdominal pain, diarrhea, and intestinal ulcers with or without bleeding. Cardiac: 10% of patients. Including pericarditis, coronary arteritis, cardiomyopathy, and conduction defects. Wegener’s Granulomatosis Lab findings: Elevated ESR; Normocytic anemia, leukocytosis, thrombocytosis. Rheumatoid factor (+): 50% ANCA(+), cytoplasmic pattern: 90% in active stage and 40% in remission. RBC and RBC casts in urinalysis. Rising creatinine indicates renal failure. Diagnosis: Biopsy evidence of vasculitis. The most tru reliable disgnostic tissue is obtained by open lung biopsy. Treatment: Cyclophosphamide for the mainstay of treatment. Corticosteroid for initial therapy. Churg-Strauss Syndrome (Allergic Granulomatosis and Angiitis) A necrotizing, granulomatous, small-vessel vasculitis associated with asthma, sinusitis, and eosinophilia. Pulmonay involvement is the cardinal feature of it. Patients generally have a long history of upper respiratory allergies, asthma, and eosinophilia before the onset of syndrome. Increased levels of IgE and peripheral eosinophilia are common in untreated patients, and asthma, sinusitis, and allergic rhinitis are major manifestation of the disease. Pulmonary: Adult-onset asthma is most common, affecting nearly all patients; Patchy infiltrates seen in half of the patients, are generally evanescent, and may sometimes associated with pleural effusion. Churg-Strauss Syndrome (Allergic Granulomatosis and Angiitis) Constitutional symptoms - Malaise, fatigue, flulike symptoms, weight loss (70%), fever (57%), myalgias (52%) ,arthralgias (40%) Skin manifestations (49%): Purpura, skin nodules, urticarial rash, necrotic bullae, digital ischemia Cardiac manifestations – congestive heart failure, restrictive cardiomyopathy, and pericarditis. Gastrointestinal symptoms (31%) - Symptoms related to GI vasculitis and GI bleeding Peripheral neuropathy - Mononeuritis multiplex (most frequent form, occurring in as many as 77% of patients) Renal: FSGN 50% Churg-Strauss Syndrome (Allergic Granulomatosis and Angiitis) Lab findings: Elevated ESR; Anemia, eosinophilia; Elevated IgE level. ANCA(+): 70%, perinuclear pattern. Rheumatoid factor (+): 50% RBC, RBC casts and proteinuria in urinalysis. Churg-Strauss Syndrome (Allergic Granulomatosis and Angiitis) Diagnosis: 6 criteria proposed by the American College of Rheumatology in 1990: (1) asthma (2) peripheral eosinophilia of 10% or higher on differential leukocyte count (3) mononeuropathy (including multiplex) or polyneuropathy (4) paranasal sinus abnormality (5) nonfixed pulmonary infiltrates (6) biopsy-proven extravascular eosinophila The presence of 4 or more of these criteria distinguished CSS from other vasculitides, with a sensitivity of 85% and a specificity of 99.7% Biopsy confirmation of vasculitis is mandatory, however, the most fruitful biopsy sites are nerve, skin, lung and kidney. Anti-neutrophil Cytoplasmic Antibody (ANCA) Antibodies directed against certain proteins in the cytoplasm of neutrophils. Two major categories of ANCA based on different targets for the antibodies: cytoplasmic (cANCA) and perinuclear (pANCA). cANCA are found primarily in patients with Wegener’s granulomatosis (90%), microscopic polyarteritis, and active glomerulonephrtis. pANCA occurs in various vasculitis disorder, such as polyarteritis nodosa(PAN), Churg-Struss syndrome, polyangiitis overlaping syndrome, Goodpasture’s syndrome, and inflammatory bowel disorder(ulcerative colitis). 80% of patients in whom pANCA are found has evidences of vasculitis or disorders mentioned above. Impression Wegener’s Granulomatosis or Churg-Strauss Syndrome Or Miliary tuberculosis Diagnostic Procedure Thoracoscopic or open-lung biopsy & ANCA test Thanks for Your Attention