Continuous Renal Replacement Therapy
advertisement

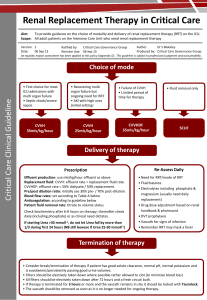
Continuous Renal Replacement Therapy -CRRT Classical ‘renal’ indications for starting renal replacement therapy (RRT) are: Rapidly rising serum urea and creatinine or the development of uraemic complications Hyperkalaemia unresponsive to medical management Severe metabolic acidosis Diuretic resistant pulmonary oedema Oliguria or anuria ‘Non renal’ indications for starting RRT are: Management of fluid balance e.g. in cardiac failure Clearing of ingested toxins Correction of electrolyte abnormalities Removal of inflammatory mediators in sepsis? Rhabdomyolysis Diffusion- movement of solutes across a semi permeable membrane through a concentration gradient Good for smaller sized molecules Convection- movement of fluid across a semi permeable membrane creating a solute drag. Good for smaller and middle sized molecules When to start RRT Conventional starting criteria for RRT should be used Treatment should be started before complications develop- Earlier the better! The rate of change of urea and creatinine is more significant than their absolute levels, however in most cases RRT should be started before urea is 20 – 30 mmol/L. Initiation of RRT on the basis of fluid balance, urine output, potassium level or degree of acidosis will be dependent on the patient’s clinical condition. What type of RRT SCUF CVVH CVVHDF CVVHD SLED(D) Ultrafiltration-UF CVVH CVVHDF a blood pump provides solute removal by diffusion and convection simultaneously. It offers high volume ultrafiltration using replacement fluid which can be administered pre-filter/ post-filter. Simultaneously, dialysate is pumped in counter flow to blood. CVVH v CVVHDF There is no evidence to suggest that CVVH is superior to CVVHDF in terms of patient outcome or renal outcome (or vice versa). With CVVHDF -UF flow rates may be reduced therefore larger molecule removal by convection is decreased If adequate UF rates cannot be achieved using CVVH due to machine limitations, then CVVHDF should be considered. A predominantly convective mode of clearance may be considered in severe sepsis Solute clearance- depends on Blood flow Recirculation Membrane characteristics- type of filter Filter clotting- aim for 85% of prescribed dose Pre/post dilution The removal of potassium, correction of acidosis or the removal of fluid may have just as much of an impact on patient outcome as solute clearance. Pre filter dilution Post filter dilution Ultrafiltration flow rates Moves towards higher UF rates Too low reduces clearance of solutes Too high- affect membrane performance Filtration fraction <25% Ultrafiltration Rates Ronco et al (2000) large prospective study Suggestion that a higher level of solute clearance was beneficial at higher UF rates. (35 mls/kg/hr) American Acute Renal Failure Trials Network (ATN study, 2008), did not find any difference in survival, rate of renal recovery or nonrenal organ failure in ‘intensive’ versus ‘less-intensive’ renal support. The Australian/NZ RENAL study (Randomised Evaluation of Normal vs. Augmented Level of renal replacement therapy in ICU, 2009) compared 40 ml/kg/h to 25 ml/kg/h of ultrafiltrate production in CVVHDF. No difference in terms of outcome. Points for consideration Replacement fluid Membrane Anticoagulation Flow rates- vascular access Temperature management Drug dose adjustment Replacement fluid Composition similar to normal serum electrolytes Bicarbonate/lactate buffer. The individual components of filtration fluid vary but phosphate and potassium supplementation is often needed. Bicarbonate may trigger inflammatory mediators, an undesirable side effect in the critically ill and could theoretically be harmful. Membranes High surface area Used to be cellulose, now synthetic biocompatable Pore size affects solute transfer Phosphates are lost at the same rate as urea Doesn’t clear protein bound molecules eg midazolam Doesn’t secrete toxins like a tubular cell Removes glucose Future ? Bioartificial kidney with human tubular cells lining hollow fibers Anticoagulation Anticoagulation No anticoagulation UFH unfractioned heparin LMWH low molecular weight heparinFragmin Prostacyclin Citrate Others No Anticoagulation Increased risk of clotting Increased consumption of clotting factors and platelets Short circuit life Preventative Measures Pre-dilution High Flow Aim for Filtration fraction of 25% or less Heparin Occurs naturally in human mast cells within the connective tissue of the blood vessels, liver and lungs. Results seen instantly with a half-life of 30 minutes – 2hours reversal with protamine sulphate but Fresh Frozen Plasma remains the definitive treatment. Heparin induced Thrombocytopaenia (HIT) Keeling, D (2006) The management of heparin-induced thrombocytopenia British Society for Haematology 133: p259269 Heparin Used in patients with normal coagulation profile, normal platelet count and not at risk of bleeding The most commonly used anticoagulation for CVVH. Its cheap, effective and well tolerated. APTT and platelet counts routinely measured (no consensus on the frequency of testing -APTT does not always reflect the anticoag effect of heparin) (There is no correlation between increasing APTT and filter life) Fragmin No evidence that it is superior to Unfractioned heparin in terms of efficacy or risk of side effects Extended half life Less risk of HIT lack of reliable predictors of bleeding and antithrombotic activity Epoprostenol (prostacyclin, Flolan®) Considerable use in IHD and CVVH Inhibits platelet aggregation Can use in thrombocytopenia 50% reduction in bleeding therefore beneficial with high risk of patients Short half life of 3 minutes IHD= intermittant haemodialysis Epoprostenol (prostacyclin, Flolan®) Common concerns Expensive and has powerful vasodilator properties Side effects of hypotension, flushing and headache. There is no reliable laboratory test to quantify the anticoagulation effect Its not effective for filter membrane fouling due to fibre clotting Citrate Citrate binds with calcium and makes it unavailable for clotting cascade so need to -monitor serum calcium and give calcium infusion -monitor sodium and acid-base status as citrate to bicarbonate. Suggestion that citrate prolongs CRRT time and reduces need for blood transfusions and/or haemorrhage Others Danaparoids; Fondaparinux- little experience of use in CVVH; monitor anti Xa levels Recombinant hirudin and argatroban are direct thrombin inhibitors. Experience with these drugs is limited, but increasing and they may have pharmacological advantages. Vascular access Usually double D or D/O x section >11FG for blood flows >200-250ml/min Polyurethane- 3 weeks Jugular -Right side less recirculation ? subclavian Femoral catheters shorter than 20cm associated with increase recirculation Hypothermia Do the following have any place in preventing hypothermia ? Wrap circuit Fluid warmer Systemic warming Hypothermia Do the following have any place in preventing hypothermia ? Wrap circuit NO Fluid warmer NO Systemic warming the only available option Blood Requests Due to the high volumes of filtration fluid with the increased pump speed and UF rates we need to monitor phosphate and calcium daily Bloods for U & E, FBC, Clotting- minimum daily TROUBLE SHOOTING Connections top/bottom filter! Air detector Heparin infusion pump Vascular access Alarms Thank You