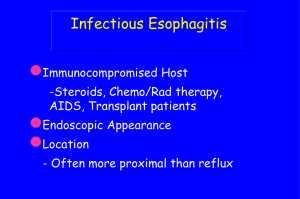
ESOPHAGITIS: CAUSES Organisms (fungal)
advertisement

THERAPEUTIC FAILURE The reason we are here today Therapeutic failure Wrong diagnosis Right diagnosis Wrong treatment Right diagnosis Right treatment Wrong client Therapeutic failure Wrong diagnosis Right diagnosis Wrong treatment Right diagnosis Right treatment Wrong client Therapeutic failure Wrong diagnosis Right diagnosis Wrong treatment Right diagnosis Right treatment Wrong client Therapeutic failure Wrong diagnosis Right diagnosis Wrong treatment Right diagnosis Right treatment Wrong client Patient is "spitting up" Regurgitation Vomiting Expectoration DEFINING THE PROBLEM VOMIT REGURG Prodromal signs usually no Retching usually no Bile sometimes no Digested blood sometimes no If it looks like vomiting, it is probably vomiting If it looks like regurgitation, then you don’t know for sure If it looks like vomiting, it is probably vomiting If it looks like regurgitation, then you don’t know for sure But it is still more efficient to look for causes of regurgitation first TAMU #79877 TAMU #151587 TAMU #151587 TAMU #117587-9/09 TAMU #117587-12/09 TAMU #156420 TAMU #156420 TAMU #159116 Sig: 4 month F German shepherd CC: Febrile HPI: 1 month ago: dog febrile with soft cough – cured with antibiotics 3 days ago had same signs PE: T = 39.5 C No other abnormalities MSU #167884 Sig: 10 yr M(c) Mixed breed dog CC: Coughing HPI: Coughing began 2 years ago and is not controlled with any medications Dog now vomiting for 2 months Causes of Congenital Esophageal Weakness • Idiopathic Causes of Acquired Esophageal Weakness • Idiopathic • Myasthenia gravis (localized) • Hypoadrenocorticism (usually atypical) • Various Myopathies/Neuropathies • Spirocerca lupi • Tetanus/Botulism • Distemper • Hypothyroidism (?) • Trypanosomiasis (??) Acquired Weakness Congenital Weakness Look for cause Idiopathic Cause found Treat cause Idiopathic Supportive therapy Acquired Weakness Congenital Weakness Look for cause Idiopathic Cause found Treat cause Idiopathic Supportive therapy THERAPY FOR CONGENITAL MEGAESOPHAGUS • Dietary modification – Gruel from an elevated platform THERAPY FOR CONGENITAL MEGAESOPHAGUS • Dietary modification – Gruel – Meatballs (esp with partial motility) – Canned food – Dry food TAMU #124375 Sig: 2 yr M(c) Dalmatian CC: Vomiting HPI: Present since obtained dog 1 month ago. Dog “inhales” food & immediately vomits food without bile or blood Dog drools constantly Recently has trouble swallowing PE: Not remarkable TAMU #118002 Sig: 5 month F German shorthaired pointer CC: Vomiting HPI: 8 days ago: vomiting clear liquid Next day vomited blood and sticks Laparotomy: inflamed duodenum & blood in stomach Still vomits fluid & blood PE: No significant findings TAMU #118002 CBC: PCV = 20% (35-55) Profile: Albumin = 1.9 gm/dl (2.5-4.4) TAMU #99514 2/3 Sig: 10 yr F(s) Bichon CC: Vomiting HPI: Started vomiting bile on 1/12 Removed linear foreign object Vomiting continues: surgical pyloromyotomy 3 days later PE: Depressed, tight abdomen ESOPHAGITIS: CAUSES Organisms (especially fungal) ESOPHAGITIS: CAUSES Organisms (fungal) Foreign objects ESOPHAGITIS: CAUSES Organisms (fungal) Foreign objects Caustic agents ESOPHAGITIS: CAUSES Organisms (fungal) Foreign objects Caustic agents doxycycline clindamycin ciprofloxacin NSAIDs ESOPHAGITIS: CAUSES Organisms (fungal) Foreign objects Caustic agents Gastric acid Excessive gastric acidity ESOPHAGITIS: CAUSES Organisms (fungal) Foreign objects Caustic agents Gastric acid Excessive gastric acidity Excessive vomiting ESOPHAGITIS: CAUSES Organisms (fungal) Foreign objects Caustic agents Gastric acid Excessive gastric acidity Excessive vomiting Iatrogenic (post anesthesia) ESOPHAGITIS: CAUSES Organisms (fungal) Foreign objects Caustic agents Gastric acid Excessive gastric acidity Excessive vomiting Iatrogenic (post anesthesia) Spontaneous gastric reflux ESOPHAGITIS: CLINICAL SIGNS Mild disease: “spit up” white phlegm ESOPHAGITIS: CLINICAL SIGNS Mild disease: “spit up” white phlegm Moderate disease: poor appetite, regurgitate food ESOPHAGITIS: CLINICAL SIGNS Mild disease: “spit up” white phlegm Moderate disease: poor appetite, regurgitate food Severe disease: anorexia, drooling, severe pain, regurgitation, vomiting ESOPHAGITIS: DIAGNOSIS History (e.g., repeated vomiting, recent anesthesia) ESOPHAGITIS: DIAGNOSIS History (e.g., repeated vomiting, recent anesthesia) Physical examination (oral lesions) ESOPHAGITIS: DIAGNOSIS History (e.g., repeated vomiting, recent anesthesia) Physical examination (oral lesions) Radiographs (lesions may be subtle) ESOPHAGITIS: DIAGNOSIS History (e.g., repeated vomiting, recent anesthesia) Physical examination (oral lesions) Radiographs (lesions may be subtle) Endoscopy (most sensitive/specific) CHEMICAL CLEARANCE • The ulcerated/eroded esophagus is ultra-sensitive to even minute amounts of acid • You must “clear” the stomach of acid – the more severe the esophagitis, the more you must eliminate gastric acid secretion ESOPHAGITIS: TREATMENT • Antacids – – Proton pump inhibitors H-2 receptor antagonists ANTI-ACID DRUGS: PPI’s • Proton pump inhibitors – Irreversibly inhibit H+-K+ ATPase • Omeprazole (1-2 mg/kg PO q12-24h) • Lansoprazole (1 mg/kg IV q24h) • Pantoprazole (1 mg/kg IV q24h) • Esomeprazole (1 mg/kg IV q24h) – start working immediately, but require 2-5 days to achieve maximal effect – Can cause diarrhea ESOPHAGITIS: TREATMENT • Antacids • Prokinetics Volume clearance • Cisapride (0.1-0.5 mg/kg PO q1224h) better than metoclopramide • Mosapride available soon? (IV) • Erythromycin (1-5 mg/kg PO, IV,q8-12h) • Metoclopramide (0.25 mg/kg IV, PO, q8-12 h) more effective on liquids • Ranitidine (2.2-4.4 mg/kg PO, IV q8-12h) ESOPHAGITIS: TREATMENT • Antacids • Prokinetics • Analgesics (primarily topicals) ESOPHAGITIS: TREATMENT • Antacids • Prokinetics • Analgesics • Gastrostomy tube (rarely needed) ESOPHAGITIS: TREATMENT • Antacids • Prokinetics • Analgesics • Gastrostomy tube • Carafate ? ESOPHAGITIS: TREATMENT • Antacids • Prokinetics • Analgesics • Gastrostomy tube • Carafate ? • Antibiotics? • Steroids? TAMU #178379 TAMU #174578 TAMU #174578 – with abd pressure TAMU #107138 Sig: 8 yr F(s) Mix 20 kg CC: Vomiting HPI: Started 5 weeks ago Vomits every other day or more often Vomitus often has yellow component Has lost 3.18 kg over the last month Referring vet has dx’ed hiatal hernia and reflux PE: No significant abnormalities TAMU #107138 Sig: 8 yr F(s) Mix 20 kg CC: Vomiting HPI: Started 5 weeks ago Vomits every other day or more often Vomitus often has yellow component Has lost 3.18 kg over the last month Referring vet has dx’ed hiatal hernia and reflux PE: No significant abnormalities HIATAL HERNIA Symptomatic Asymptomatic Young Old Symptoms may be due to hiatal hernia Symptoms possibly due to other disease Surgery may be appropriate Medical therapy might be best HIATAL HERNIA Symptomatic Asymptomatic Young Old Symptoms may be due to hiatal hernia Symptoms possibly due to other disease Surgery may be appropriate Medical therapy might be best HIATAL HERNIA Symptomatic Asymptomatic Young Old Symptoms may be due to hiatal hernia Symptoms possibly due to other disease Surgery may be appropriate Medical therapy might be best