Transfusion _10-18-13_revised PMG
advertisement

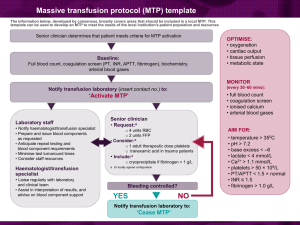
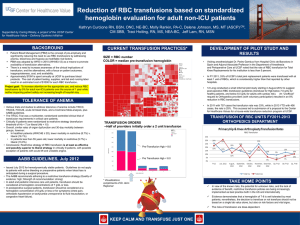
BLUE CROSS BLUE SHIELD OF MICHIGAN CARDIOVASCULAR CONSORTIUM VASCULAR INTERVENTIONS COLLABORATIVE- (BMC2 VIC) P. Michael Grossman, MD Director, BMC2 PVI Associate Professor University of Michigan Hospitals and Health Center October 2013 Focus for Today Update on our recent expansion and addition of new sites Brief overview of data from the PVI part of our Collaborative History of transfusion in BMC2 Future direction What is the “Blue Cross Blue Shield of Michigan Cardiovascular Consortium Vascular Intervention Collaborative?” I only have a few minutes, so from now on….. BMC2 VIC What is BMC2 VIC? Regional, physician-run, multidisciplinary collaboration Partnership with Blue Cross Blue Shield of Michigan Assess and improve quality of care and outcomes of PVI patients Overcome barriers of traditional market and academic competition Collect, organize, audit, and analyze data Report procedural variables and outcomes Individual physician operators Institutions Support quality improvement initiatives 4 Which Physicians Participate? Consecutive cases from all vascular interventions in participating hospitals Truly multidisciplinary Vascular surgery Interventional radiology Interventional cardiology 2014 PVI – 47 Participating Hospitals/Outpatient Centers New PVI Outpatient Center Participants Michigan Vascular Center Michigan Outpatient Vascular Institute BMC2 PVI/VIC DATA OVERVIEW PVI Patient Characteristics PVI Patients Have Multiple Co-Morbidities 2012 (%) n=8927 Female Gender Average Age (years) Current Smoker Hyperlipidemia Hypertension Diabetes Mellitus CHF COPD CVD/TIA CAD Renal Failure on Dialysis Body Mass Index Anemia 43.8 68.5 40.5 86.8 91.3 47.7 20.8 28.7 29.2 59.7 5.7 30.1 43.5 Percent of PVI Procedures by Arterial Bed BMC2 PVI Outcome Trends: 2007 – YTD Q2 2013 23% Percent 38% 14% 44% 6-Month Medication Compliance* 2009 – 2012 Percent RX compliance at 6 months with discharge medications *Medication Compliance – Patient continues to take the medications as prescribed at discharge after the PVI procedure 12 6-Month Medication Compliance* Not Discharged with RX: 2009 – 2012 RX use at 6 months for patients not discharged on RX (and no documented contra-indication) *Medication Compliance – Patient continues to take the medications as prescribed at discharge after the PVI procedure 37 Transfusion HISTORY IN BMC2 BMC2 “Historical” Quality Improvement Approach Collect data Audit data Report data to participants Benchmarked to collaborative Good performers congratulated Underperformers scrambled to meet the mark or ignore the reports Communication with physician champions and site data coordinators “Trickle Down” Quality Improvement Early PVI Transfusion Data Early Transfusion Data Quality Improvement Initiative: 2008 Initiative focused on decreasing peri- procedural bleeding complications and post-procedural transfusion Weight-based heparin anticoagulation dosing Initial procedural heparin dose should be ≤ 60 U/kg Check intra-procedural ACT Heparin to achieve an ACT of 200 to 250 seconds Follow guidelines for blood transfusion 18 From “Trickle Down” to “Aim for a Target” “…Setting a target resulted in better performance and significant cost savings (in janitorial services).” Quality Improvement Goals: 2009-2010 Physician Advisory Committee approved creation of numeric PVI goals based on Collaborative data and goal to smooth practice variation across sites and reduce outliers: ASA at Discharge > 90% Statin at Discharge >75% Vascular Complications < 4% Post PVI Transfusion < 7% Contrast Induced Nephropathy < 7% A Quality Improvement Team was Created QI team performed 24 site visits over a 2 year time period Visited sites where outcomes were low Discussed a detailed questionnaire regarding site processes for peripheral vascular procedures Obtained site protocols and order sets Identified and starred the very best practices from these visits Worked with the QI Team to merge the best practices together into a BMC2 compendium of “Best Practices” QI Site Visit Questionnaire - Transfusion April 2010 BMC2 Meeting All BMC2 meeting to obtain a comprehensive review of the outcome literature, ways to prevent complications and patient management Transfusion was one of the areas of focus “Best Practice” protocols distributed to all sites – transfusion protocols included Added focus on patients transfused with Hgb >8.0 Additional quarterly hospital QI Reports were also created with detailed outcome specific information Transfusion as an Adverse Outcome Independent risk factor for mortality in several cardiovascular studies Transfusion associated with bleeding Increased hospital stay Increased cost Other risks of transfusion: RBCs in stored blood act as NO “sinks” Increase vasoconstriction, platelet aggregation Stored RBCs are low in 2,3-diphosphoglyceric acid and have high oxygen affinity Increased inflammatory mediators Exacerbation of myocardial ischemia 24 Transfusion Literature ACS Patients who received a blood transfusion had markedly worse 30-day mortality compared with those who did not receive a transfusion. Rao SV, et. al., JAMA 2004; 292:1555–1562 Patients undergoing lower extremity revascularization; found a higher risk of postoperative mortality, pulmonary, and infectious complications after receiving intraoperative blood transfusion. O’Keeffe SD, et. al. J Vasc Surg 2010; 51:616-21 25 Transfusion Literature (cont.) Independent association between RBC transfusion and increased risk of 1-year mortality. PCI Patients receiving blood > 35 days old had significantly worse 1-year survival rates compared with patients receiving blood < 35 days old and patients not transfused. Kim, P., et. al. Clinical Cardiology 2007; 30:II-35-43 In patients undergoing cardiac surgery, transfusion of red cells that had been stored for more than 2 weeks was associated with a significantly increased risk of postoperative complications as well as reduced short-term and long-term survival. Koch CG et al. N Engl J Med 2008; 358:1229-1239 26 2010 BMC2 Best Practice Protocols 2010 BMC2 Best Practice Protocols 2010 BMC2 Best Practice Protocols 2008 - 2010 Transfusion Rate – 6% to 7% RESULTS FROM OUR POST-PROCEDURE TRANSFUSION QI INITIATIVE? 2011 Survey: Value of BMC2 Best Practices 49 Responses: 75% had obtained the protocols 66% thought the protocols added value to quality improvement in the BMC2 Collaborative 46% stated the protocols were used at their site to support quality improvement Several others mentioned that quality improvements were “in process” BMC2 PVI Outcome Trends for Transfusion: 2007 – YTD Q2 2013 Transfusion Rate (%) 52% Transfusion RECENT PVI SURVEY RESULTS SEPTEMBER/OCTOBER 2013 15 RESPONDENTS Recent PVI Survey Results Do you transfuse at a threshold of: Recent PVI Survey Results Do you use clinical parameters to decide when to transfuse in addition to Hgb? If so: Recent PVI Survey Results Does your hospital employ techs, nurses, PAs or other professionals who obtain femoral artery access in the cath lab?: Recent PVI Survey Results In a patient with a post operative NSTEMI and Hgb = 9.5 would you transfuse? Recent PVI Survey Results In a post procedure patient with CAD and without symptoms of ischemia and a Hgb = 7.5 would you transfuse this patient? Transfusion FUTURE DIRECTION Predictors of PVI Post-Procedure Transfusion All Variables - Excludes hybrid procedures Significant Variables (P-value < 0.05) Variable Odds Ratio Lower Limit CI Upper Limit CI Female 1.981 1.759 2.230 BMI 0.984 0.975 0.994 Hx CHF 1.322 1.156 1.512 Hx COPD 1.370 1.213 1.548 Hx CVD/TIA 1.284 1.140 1.446 Hx CAD 1.223 1.049 1.425 Hx Prior PCI 0.865 0.752 0.994 Hx Prior CABG 0.790 0.683 0.913 Current/Recent GI Bleed 2.128 1.618 2.799 Hx Afib 1.246 1.081 1.437 Hx Renal Failure/Current Dialysis 1.417 1.156 1.738 Hx Renal Transplant 0.549 0.315 0.955 Predictors of PVI Post-Procedure Transfusion (cont.) All Variables - Excludes hybrid procedures Significant Variables (P-value < 0.05) Variable Odds Ratio Lower Limit CI Upper Limit CI IV Heparin Post-Procedure 5.763 5.010 6.630 Indication = Claudication 0.803 0.709 0.909 Indication = Limb Ischemia 2.118 1.853 2.421 Pre-Procedure Anemia (WHO def.) 4.645 3.996 5.399 Pre-Procedure Creatinine >1.5 1.249 1.072 1.454 Mesenteric Procedure 2.078 1.483 2.913 Heparin Dose (>=60 units/kg) 1.214 1.069 1.378 C stat 294.7, P-value 0.6381, AUC 84.05% Variables: Preliminary Risk Model Family History of premature CAD Hyperlipidemia Hypertension Diabetes CHF Significant Valve Disease COPD CVD/TIA CAD Prior PCI Prior MI Prior CABG Current/Recent GI Bleed Afib Other Atherosclerotic Disease Renal Failure Renal Transplant Gender Age BMI Pre Procedure Aspirin Pre Procedure Clopidogrel Pre Procedure Prasugrel Pre Procedure Statin Pre Procedure Cilostazol Pre Procedure Coumadin Procedure Type: Upper Extremity Procedure Type: Lower Extremity Procedure Type: Mesenteric Procedure Type: Renal Indication = Claudication Indication = Limb Ischemia Pre Procedure Anemia (WHO definition) Pre Procedure Creatinine >1.5 43 Preliminary Risk Model Includes patient history and pre-procedure variables only – Excludes hybrid procedures Significant Variables (P-value < 0.05), AUC 81.12% Variable Hx CHF Hx COPD Hx CVD/TIA Hx CAD Hx Prior PCI Hx Prior CABG Current/Recent GI Bleed Hx Afib Hx Renal Failure/Current Dialysis Hx Renal Transplant Female BMI Pre-Procedure Warfarin Mesenteric Procedure Upper Extremity Procedure Indication = Claudication Indication = Limb Ischemia Pre-Procedure Anemia (WHO definition) Pre-procedure Creatinine >1.5 Odds Ratio 1.328 1.316 1.281 1.179 0.861 0.798 2.186 1.181 1.370 0.559 2.002 0.980 1.365 2.694 2.064 0.738 2.589 4.927 1.196 Lower Limit CI 1.165 1.168 1.141 1.010 0.748 0.692 1.678 1.017 1.121 0.326 1.782 0.971 1.151 1.565 1.188 0.648 2.245 4.247 1.031 Upper Limit CI 1.514 1.483 1.438 1.377 0.990 0.919 2.847 1.372 1.674 0.958 2.248 0.989 1.617 4.638 3.585 0.840 2.985 5.715 1.388 Post-Procedure Transfusion: OE Plot (Blinded) Collaborative Post-Procedure Transfusion OE Plot Future Direction Implementation of risk model for transfusion into quarterly reports Issuance of “final” 2013 BMC2 Best Practice Protocols this winter – will contain Post op MI, SSI, and transfusion in a surgical setting. Draft 2013 Best Practices are in your folders today. 47 BMC2 Welcomes Dr. Carson We are looking forward to hearing his presentation later this morning and are grateful to him for joining us today. Jeffrey L Carson, MD Vice Chair, Research Richard C Reynolds Professor of Medicine Chief, Division of General Internal Medicine Rutgers Robert Wood Johnson Medical School New Brunswick, New Jersey 08901