Syncope and Hypotension in the Elderly Patient
advertisement

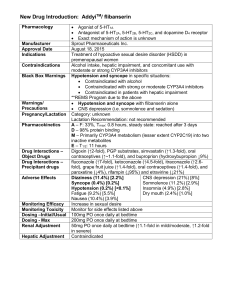
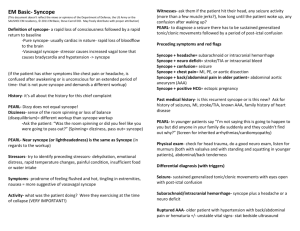
Syncope and Hypotension in the Elderly Patient Lewis A. Lipsitz, MD Hebrew SeniorLife, Beth Israel Deaconess Medical Center, Harvard Medical School Disclosures: None Syncope Definition Transient loss of consciousness, characterized by unresponsiveness and loss of postural tone, with spontaneous recovery. Epidemiology of Syncope • • • • • Prevalence up to 47% in healthy young 23% 10-year pevalence in the NH pop. 6-33% 1-year mortality in pts. over 60. $2 Billion annual costs. Up to 40% of cases remain unexplained, despite extensive inpatient evaluations. Syncope Case 1 • An 88 year old nursing home resident with hypertension, CAD, and mild dementia was found unresponsive and slumped in her chair, 1 hour after breakfast. She had taken isosorbide dinitrate, metoprolol, lisinopril, and HCTZ before breakfast. Her BP was 105/72, pulse was 64. Syncope Case 2 • An active 75 y.o. man with no active medical problems suddenly became dizzy and fainted while cleaning his apartment. A friend found him and rushed him to the hospital where he was admitted and ruled out for an MI. A head CT and exercise stress test were normal. BP and P were: 158/92, 72 supine and 90/62, 72 standing. Syncope Etiology Only if one knows the causes of syncope will he be able to recognize its onset and combat the cause. Miamonides 1135-1204 CE Etiology of Syncope in the NH Diseases Myocardial Infarction Aortic Stenosis Dehydration Seizure Disorder Cerebrovascular Event Cardiac Ischemia Tachy-Brady Syndrome Lipsitz, LA, J Chronic Ds, 1986; 39:619 No. of Patients 6 5 4 3 3 3 3 Etiology of Syncope - 2 Diseases No. of Patients Acute respiratory failure 2 Cervical Spondylosis 1 Sinus arrest 1 Paroxysmal atrial tachycardia 1 Carotid sinus syndrome 1 Heart block 1 Etiology of Syncope - 3 Situational Stresses No. of Patients Drug-induced hypotension 11 Postprandial hypotension 8 Defecation/colostomy irrigation 7 Orthostatic hypotension 6 Fecal impaction 3 Vomiting 1 Micturition 1 Bending over 1 Etiology of Syncope - 4 Unknown No identifiable precipitants Unexplained hypotension No. of Patients 17 8 Elderly patients are at risk of hypotension during common daily activities. Age-related Changes in BP Regulation • • • • Decreased cerebral blood flow Baroreflex impairment Reduced renal salt and water conservation Impaired early diastolic ventricular filling 190 SUP STD BREAK STD/AMB NTG STD AMB MED LUNCH STD SBP (mm Hg) 170 150 old 130 young 110 90 7 8 9 10 Time (hours) 11 12 1 The Higher You Are, The Farther You Fall Honolulu Heart Study Prevalence of OH* 12.0% 10.0% 8.0% 6.0% 4.0% 2.0% 0.0% 71-74 75-79 Masaki, Circulation 1998;98:2290 80-84 Age 85+ * 3 min stdg Prevalence of OH by Age Age N 55-59 621 % with >20 mmHg drop 11.6 60-64 1,617 10.6 65-69 1,288 12.2 70-74 982 15.9 Prevalence of OH by Level of Supine SBP Supine SBP N <120 567 % with >20 mmHg drop 2.8 120-139 1,549 5.2 140-159 1,362 13.6 >160 1,030 26.6 Prevalence of OH by Age if Supine SBP > 160 mmHg Age N 55-59 99 % with > 20 mmHg drop 28.3 60-64 309 24.6 65-69 312 26.3 70-74 310 28.4 Effect of Hypotension on the Brain Role of Medications in Hypotension and Syncope? The effect of HCTZ and mild volume contraction on BP response to tilt in healthy young and elderly subjects. Shannon RP, et al, Hypertension 8:438, 1986 Orthostatic Hypotension is Reduced By Chronic Antihypertensive Therapy Baseline mo t No r 22 20 22 18 18 10* 4 4 0 0 0 e.. Ni fed . ipi M eto ne pr olo En l ala pr il Pr az os in Th iaz ide 25 Prevalence 20 15 (%) of Orthostatic 10 Hypotension 5 0 2 Years Masuo et al. AJH 1996; 9: 6* Does Antihypertensive Therapy Threaten Cerebral Blood Flow? Sit-to-stand Procedure • Avoids hydrostatic changes in perfusion pressure (vs. tilt). • Simulates a common activity of daily living. • Causes rapid and reproducable declines in arterial pressure. Effect of 6 Months of BP Control on Cerebral Blood Flow Lipsitz, et. al., Hypertension, 2005 What’s Different About Syncope in Elderly People? • Multiple Pathologic Conditions • Situational Hypotension – Postprandial – Drug-induced – Orthostatic • Cardiovascular causes > vasovagal • Vasovagal prodrome is less common. • Reflex Syncope - e.g. Carotid Sinus Synd. Syncope Evaluation • Hx of diseases, drugs, and precipitants • PE for CV ds., neuro signs, GI bleeding • BP during activities preceding syncope: posture change, meals & medications. • Carotid sinus massage (if no CVD or cardiac conduction disease) • Focused laboratory studies Syncope Evaluation - Labs • • • • • • • For most patients: EKG, Chem screen, CBC. If cardiac sx, or abnormal EKG - r/o MI If Hx of CVD - ambulatory cardiac monitor If situational - ambulatory BP monitoring If suspicious murmur - cardiac echo/Doppler If focal neuro findings or Seizures - EEG/CT If unexplained - Tilt and EPS Whom to Admit? Boston Syncope Rule (97% Sens., 62% Spec. for adverse outcome or critical intervention (Grossman, JEM 2007)) 1) Signs and sx of an acute coronary syndrome; 2) Signs of conduction disease; 3) Worrisome cardiac history; 4) Valvular heart disease by history or physical; 5) Family history of sudden death; 6) Persistent abnormal vital signs in the ED; 7) Volume depletion such as persistent dehydration, GI bleeding, or hematocrit < 30; and 8) Primary CNS event. Definition of Orthostatic Hypotension • 20 mmHg or greater decline in systolic BP and/or 10 mmHg or greater decline in diastolic BP when changing from a supine to upright position (sitting or standing). • 1 and/or 3 minute value. • HR is not a reliable indicator in geriatric patients because of baroreflex impairment. Causes of OH • Systemic – Hypertension – Dehydration – Deconditioning – Adrenocortical insufficiency • Drugs – Antipsychotics – MAOs & tricyclics – antihypertensives (acute doses) – vasodilators (NTG) – L-Dopa – BBs, CCB’s, etc. Causes of OH • Autonomic Neuropathy • CNS Disorders – Diabetes Mellitus – Multiple Systems Atrophy – Amyloidosis – Parkinson’s Disease – Tabes Dorsalis – Multiple Strokes – Paraneoplastic – Myelopathy – Alcohol – Brain stem lesions – Nutritional Evaluation of OH • Sx: Postural dizziness, falls, or syncope; po intake; abnl. sweating, incontinence, HA,GI dysmotility, impotence, poor night vision. • Hx: HTN, DM, CA, Stroke, Parkinsons, Arrhythmias, Meds & alcohol. • PE: BP & P supine, 1 & 3 min stdg; pupils, skin, CV and neuro exams. • Labs: Hct, Lytes, Glu, SPEP, B12, RPR +/cortisol, brain imaging, tilt with NE levels, HRV during deep breathing & Valsalva, sweat tests. Nonpharmacologic RX of OH • • • • • • • Drug withdrawal, substitution or reduction Avoid warm environment Avoid straining activity Squatting, leg crossing Increase salt intake Waist-high compression stockings Sleeping in the head-up position Definition of PPH 20 mm Hg or greater decline in systolic BP within 2 hours of the start of a meal. PPH - Clinical Associations • Patients with HTN, autonomic insufficiency, Parkinson’s Disease, Diabetes, Renal failure • 24-36% of nursing home residents. • 23% of elderly patients admitted to a geriatric hospital with syncope or falls. • 50% of elderly pts. with unexplained syncope • Angina, TIA’s, lacunar infarcts, leukoaraiosis Evaluation of PPH • BP pre & post meal: 400 kcal, 7080% CHO. • Hx: Meds, EtOH, autonomic Sx, HTN, DM, CVD, Parkinson’s, autonomic neuropathy. • post-meal EKG to r/o angina. • consider dumping syndrome. Nonpharmacologic Rx of PPH • Stop hypotensive meds or give between meals. • Avoid preload reduction (diuretics or prolonged sitting), maintain adequate intravascular vol. • Avoid EtOH. • Multiple small meals of protein and fat. • Walking exercise after meals (frail elderly). • ? cold rather than warm meals. Mean Arterial Pressure (mmHg) 110 100 90 80 Walk -5 0 5 10 15 20 25 30 35 40 45 50 55 60 65 70 75 80 Time after meal (min) Nach dem essen sollst du ruhen oder tausand schritte tuen. -German folk wisdom Pharmacologic Rx of OH and PPH • Caffeine: 250 mg (2 cups brewed) in AM • Fludrocortisone: 0.1 to 1.0 mg QD (watch for CHF, supine HTN, and hypokalemia. • Midodrine: 2.5-10 mg po TID (supine HTN) • Octreotide: 50 mg subQ, 30 min. pre-meals Challenges and Unmet Needs 1. Causes of Unexplained Syncope? – Neurally-mediated (vasovagal): fewer premonitory sx in elderly patients. – Dysautonomia – Paroxysmal brady- or tachy-arrhythmias – Carotid Sinus Hypersensitivity 2. Better Diagnostic tools – Tilt tests, EPS, BP monitoring? Validate Syncope Rule in Elderly 3. Methods to improve cerebral perfusion. Principles of Treatment • Treat the primary etiology if one is found. • Age is NOT a contraindication to treatment, but increases the risk of drugs and surgery. • Identify and minimize the impact of multiple contributors, particularly drugs. • Behavioral interventions to avoid situational hypotension.