Corneal Abrasions
advertisement
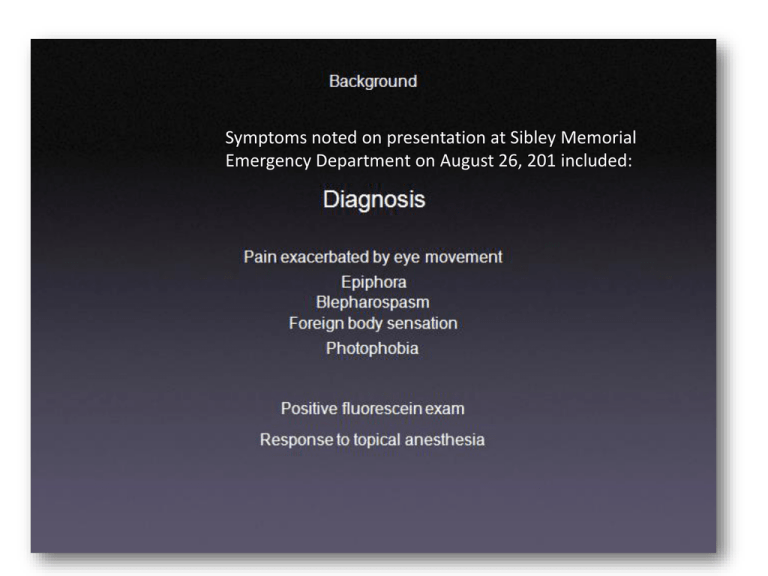
Symptoms noted on presentation at Sibley Memorial Emergency Department on August 26, 201 included: This is the cover of a brochure published in the summer of 2011 by Sibley Hospital. Featured on the cover is Dr. Cope’s photograph along with an introductory heading to a new fast track initiative to move patients in and out of the ER at an accelerated pace. I was at the ER for a total of 35 minutes and one wonders how much of that had to do with this financially motivated “imitative”. This presentation includes salient points about the injury, infection and subsequent Pain and suffering that I sustained as a result of misdiagnosis and mistreatment that Exacerbated or caused a melting corneal ulcer. The mismanagement of my Heathcare on August 25th occurred at Sibley Memorial Hospital by attending physian Gregory Cope, MD. Corneal abrasions`(From HCP LIVE published in 2007) The management of corneal abrasions involves pain relief and prevention of secondary infection. The decision to patch an eye after a corneal abrasion is very controversial.13 Patching the eye closed will alleviate some pain, but it does not accelerate corneal healing.14 Eye patching should be avoided if the corneal abrasion was caused by organic trauma or contact lenses because the patching can allow microbial contaminants to proliferate overnight Soft contact lens use It is also important to ask about the use of soft contact lenses. A soft contact lens wearer with a red eye should be presumed to have an infectious corneal ulcer (bacterial keratitis) until proven otherwise. There is a high incidence of gram-negative corneal ulcers (ie, Pseudomonas aeruginosa infection) in patients who sleep while wearing their contact lenses.6 Any corneal epithelial defect with an underlying "white" corneal opacity noted on examination should be assumed to be a corneal ulcer (Figure 3). Such a patient should urgently be referred to an ophthalmologist. If not properly diagnosed and treated, the risk of developing a visually debilitating scar or a corneal perforation is high because the microbial enzymes can rapidly melt the cornea.7 Treatment consists of topical fortified broad-spectrum antibiotics applied to the eye at hourly intervals. Topical corticosteroids are contraindicated in the presence of infectious corneal ulcers because they may accelerate further melting of the cornea. Where does information for the emergency physician come from? Challenge unique to the emergency physician: Relevant information can come from literature in any specialty • Original studies, review articles, editorials • Literature interpretation clearinghouses/systematic reviews: Cochrane, BestBETs, I nfo POEMs, Clinical Evidence • Opinion clearinghouses: EMA, ACP Journal Club, EM Reports • Paper textbooks (Rosen's Emergency Medicine, Yanoff's Ophthalmology) • Online textbooks (UpToDate, eMedicine, Jeff Mann's EM Guidemaps, review Of Optometry.com) • Guidelines - local, national • Local practice • Personal experience Management Note when This was published Schein, O.D., et al, Am J Emerg Med 11(6):606, November 1993. Contact Lens Abrasions and the Nonophthalmologist About 25 million persons in the U.S. wear contact lenses. Users of contact lenses who sustain corneal abrasions often initially present to primary care physicians. The authors, from the Johns Hopkins University in Baltimore, discuss the management of corneal abrasions in these individuals. Contact lens-associated ulcerative keratitis, a break in the corneal epithelium with underlying suppuration of the corneal stroma, is usually due to bacterial infection and is most commonly caused by Pseudomonas species. The risk of contact lens-associated ulcerative keratitis is increased 10- to 15-fold with overnight use of extended-wear soft lenses as compared with daily wear soft lenses. Appropriate management differs from that of the patient presenting with a corneal abrasion not associated with contact lens use. Erythromycin and sulfas that are frequently employed in patients with other types of mechanical corneal abrasion are inadequate in these cases. Aminoglycoside ointments (e.g., tobramycin or gentamicin) or combination products such as Polymyxin B and Bacitracin, which are effective against Pseudomonas, should be utilized. Routine patching is discouraged, as this intervention limits tearing and increases the temperature and humidity of the ocular surface, favoring bacterial replication. Topical steroids also promote bacterial replication. Since the patient will not experience the pain relief produced by patching, adequate oral analgesics should be employed. Early follow-up should be scheduled (typically within 24 hours), when reexamination with a slit- lamp biomicroscope should be performed. Three cases are discussed in which initial mismanagement resulted in significant sequelae (and litigation in two cases). If no infiltrate, Rx antipseudomonal abx (flouroquinalone or aminoglycoside) drops Analgesia Ophthalmology followup 24 hours Management Undebated Approaches Do not prescribe topical anesthetics for any reason Do not patch high risk corneal abrasions, meaning: The person presenting is a contact lens wearer organic matter such as a tree limb is a possible cause Emergency protocol should be implemented if there is no Improvement in symptoms four hours after removal of the contact lens. The assumption of microbial keratitis is standard and an Emergency consult with an ophthalmologist is necessary for Immediate evaluation and treatment. Management Schein, O.D., et al, Am J Emerg Med 11(6):606, November 1993. Contact Lens Abrasions and the Nonophthalmologist About 25 million persons in the U.S. wear contact lenses. Users of contact lenses who sustain corneal abrasions often initially present to primary care physicians. The authors, from the Johns Hopkins University in Baltimore, discuss the management of corneal abrasions in these individuals. Contact lens-associated ulcerative keratitis, a break in the corneal epithelium with underlying suppuration of the corneal stroma, is usually due to bacterial infection and is most commonly caused by Pseudomonas species. The risk of contact lens-associated ulcerative keratitis is increased 10to 15-fold with overnight use of extended-wear soft lenses as compared with daily wear soft lenses. Appropriate management differs from that of the patient presenting with a corneal abrasion not associated with contact lens use. Erythromycin and sulfas that are frequently employed in patients with other types of mechanical corneal abrasion are inadequate in these cases. Aminoglycoside ointments (e.g., tobramycin or gentamicin) or combination products such as Polymyxin B and Bacitracin, which are effective against Pseudomonas, should be utilized. Routine patching is discouraged, as this intervention limits tearing and increases the temperature and humidity of the ocular surface, favoring bacterial replication. Topical steroids also promote bacterial replication. Since the patient will not experience the pain relief produced by patching, adequate oral analgesics should be employed. Early follow-up should be scheduled (typically within 24 hours), when reexamination with a slit- lamp biomicroscope should be performed. Three cases are discussed in which initial mismanagement resulted in significant sequelae (and litigation in two cases). If no infiltrate, Rx antipseudomonal abx (flouroquinalone or aminoglycoside) drops Analgesia Ophthalmology followup 24 hours Management Schein, O.D., et al, Am J Emerg Med 11(6):606, November 1993. Contact Lens Abrasions and the Nonophthalmologist About 25 million persons in the U.S. wear contact lenses. Users of contact lenses who sustain corneal abrasions often initially present to primary care physicians. The authors, from the Johns Hopkins University in Baltimore, discuss the management of corneal abrasions in these individuals. Contact lens-associated ulcerative keratitis, a break in the corneal epithelium with underlying suppuration of the corneal stroma, is usually due to bacterial infection and is most commonly caused by Pseudomonas species. The risk of contact lens-associated ulcerative keratitis is increased 10to 15-fold with overnight use of extended-wear soft lenses as compared with daily wear soft lenses. Appropriate management differs from that of the patient presenting with a corneal abrasion not associated with contact lens use. Erythromycin and sulfas that are frequently employed in patients with other types of mechanical corneal abrasion are inadequate in these cases. Aminoglycoside ointments (e.g., tobramycin or gentamicin) or combination products such as Polymyxin B and Bacitracin, which are effective against Pseudomonas, should be utilized. Routine patching is discouraged, as this intervention limits tearing and increases the temperature and humidity of the ocular surface, favoring bacterial replication. Topical steroids also promote bacterial replication. Since the patient will not experience the pain relief produced by patching, adequate oral analgesics should be employed. Early follow-up should be scheduled (typically within 24 hours), when reexamination with a slit- lamp biomicroscope should be performed. Three cases are discussed in which initial mismanagement resulted in significant sequelae (and litigation in two cases). If no infiltrate, Rx antipseudomonal abx (flouroquinalone or aminoglycoside) drops Analgesia Ophthalmology followup 24 hours The Search • Cochrane • BestBets • EMA Database • infoPOEMs - [several articles I already knew about] • ACP Journal Club, Clinical Evidence [no relevant info] • National Guideline Clearinghouse, Ontario Guidelines Advisory Committee, ACEP Clinical Policies & Policy Statements, CAEP Policies & Guidelines, GuideEM, Primary Care CPG's. [no relevant info] • EM Reports - Eye emergencies and Eye trauma reviews • Journal Watch EM - [two articles I already knew about] • PubMed Applying the Patch Had I not been a contact lens wearer and not removed my lens the night before (and seen improvement in the hours since removal) and if the abrasion was considered large 10 mm in diameter then a minority of physicians may have patched the eye. The key is that they would have patched the eye, not given me the materials and written and verbal instructions to do so myself when I got home. This was presumably because I was driving however, I should have been advised not to drive. Note, the time spent in the ER was 35 minutes exactly and discharge was at 7:00 pm. In the interim it had grown to dusk outdoors. My visual acuity without correction in the left eye was legally blind. All facts known and noted by Dr. Cope. Below is a description of how patching was formerly done in non contact lens wearers: Two gauze eye pads and three strips of tape are required for patching. Antibiotic ointment is applied to the eye by instilling a small amount (1/2" to 1" ribbon) in the inferior cul-de-sac. One pad is folded in half. The patient is asked to close both eyes gently. There should be no squeezing of the orbicularis muscles. The folded patch is used to occupy the space over the globe in the orbit and apply pressure to the globe. The second pad is then placed over the folded pad. The patient or an assistant is asked to apply firm pressure to the second pad, while it is being taped firmly with the three strips of tape. These strips are most effective if place obliquely from the midline over the nose toward the cheekbone. The patient is then asked to open the eyes and report if the lid under the patch can be raised. If it can then the patch has not been applied successfully and must be redone. The patch is left in place overnight, and no more than 24 hours. A patch that is worn too long may interfere with the diagnosis of infection because the patient cannot monitor vision and discharge. Pseudomonas Ulcers Following Patching of Corneal Abrasions Associated with Contact • • • Lens Wear Clemons, Carol S. MD; Cohen, Elisabeth J. MD; Arentsen, Juan J. MD; Donnenfeld, Eric D. MD; Laibson, Peter R. MD : We report our experience with six patients-each with a history of contact lens use-who were diagnosed as having Pseudomonas corneal ulcers after having been pressure patched in treatment for apparent corneal abrasions. Four of these six patients (67%) required penetrating keratoplasty due to marked central corneal scarring following healing of their corneal ulcers. By comparison, among the 44 patients with a history of contact lens use hospitalized at Wills Eye Hospital between January 1978 and June 1986 with Pseudomonas corneal ulcers, only 11 (25%) required corneal transplantation. It is important to be aware that serious ulcers associated with the use of contact lenses can present initially as sterile-appearing erosions. Pressure patching should be avoided in patients with corneal abrasions and a history of contact lens use. Note: Even unweighted, this represents an increase by 42 percent in the percentage of patients who developed P. Aeruginosa infections soley because they were pressure patched, with no other variations in treatment, presentation or etiology. In reality the percentage is much greater because of the number of cases involved in the unpatched group. (C) 1987 The Contact Lens Association of Ophthalmologists, Inc. Vance Wilson was planning to leave on a vacation to the Black Hills of South Dakota on Friday, August 26 th, 2011 (labor day weekend. He had just purchased a Canon p95 camera and was testing it on the evening of August 24th, 2011. This photo was taken with the self timer function at about 10 pm. A few hours earlier, Mr. Wilson had removed his left contact lens due to a scratching or irritated feeling; as this photo shows, his left eye appears fairly clear at that time. Twenty hours later, he presented at the Sibley Memorial Hospital Emergency department because of increased redness, photophobia, tearing, pain, and spasm. He had not put the contact lens in since its removal before this photo was taken. Mr. Wilson followed The instructions and Used the materials given to him by Dr. Gregory Cope; patching his left eye after applying a ribbon of the erythromycin ointment from the sample tube obtained from the physician at bed time which that evening was at 12:30 am. Nine or ten hours later he awoke to blindness, copious blue-green discharge, eyes crusted shut and in debilitating pain. Shocked, he called Washington Eye Physicians and Surgeons and scheduled an Exam for that afternoon. This photo was taken by Dr. Neil Martin at Washington Eye on September 1, 2011 at approximately 3:00 PM, following a week of harrowing treatment At Johns Hopkins University in Baltimore, MD. Prior to this the eye was completely obscured By a white mucous substance. Mr. Wilson’s vision at this stage was hand movement at 4 feet. Wilson, Vance left eye on September 1, 2011 (photographed by Dr. Neil Martin – Washington Eye Physcians and Surgeons. Vance Wilson on May 25th, 2012 following corneal transplant surgery; note this surgery was needed to correct the scarring that resulted from Sibley’s mistreatment and performed almost exactly nine months after the injury and infection inflicted at Sibley Memorial Hospital. The following are issues resulting from the August, 26 th, 2011 incident noted in Mr. Wilson’s left eye as of October 15, 2012: Posterior Synechiae (scarring of the posterior chamber Unevenly shaped Iris due to melding of pupil and iris tissue during infection. +2 Cataract formed during infection Neovascularization formed during infection. Exaggerated astigmatism uneven topography. Each of these conditions has a cumulative negative impact in increasing the risk for future rejection of the transplant and additional complications, some eye threatening. (evisceration of the eye.) The surgeon who perfomred the transplant has stated that the prognosis is unknown due to the deeply scarred eye tissue; current vision in left eye is 20’70 to 20’100 (fluctuating). Mr. Wilson is still using steriod drops every four hours in his left eye. There are eleven stitches' still in the eye (originally there were 18.) Comparison photo showing scar taken on April 30th, 2012 –left eye Is at right in photograph. The Corneal transplant was performed on May 23rd, 2012. Pseudomonas Ulcers Following Patching of Corneal Abrasions Associated with Contact • • • Lens Wear Clemons, Carol S. MD; Cohen, Elisabeth J. MD; Arentsen, Juan J. MD; Donnenfeld, Eric D. MD; Laibson, Peter R. MD : We report our experience with six patients-each with a history of contact lens use-who were diagnosed as having Pseudomonas corneal ulcers after having been pressure patched in treatment for apparent corneal abrasions. Four of these six patients (67%) required penetrating keratoplasty due to marked central corneal scarring following healing of their corneal ulcers. By comparison, among the 44 patients with a history of contact lens use hospitalized at Wills Eye Hospital between January 1978 and June 1986 with Pseudomonas corneal ulcers, only 11 (25%) required corneal transplantation. It is important to be aware that serious ulcers associated with the use of contact lenses can present initially as sterile-appearing erosions. Pressure patching should be avoided in patients with corneal abrasions and a history of contact lens use. Note: This represents an increase by 42 percent in the percentage of patients who developed P. Aeruginosa infections soley because they were pressure patched, with no other variations in treatment, presentation or etiology. (C) 1987 The Contact Lens Association of Ophthalmologists, Inc. Dr. Cope noted a centrally located “defect” on my left cornea. He also noted that I had removed my left contact lens the evening before and seen in the hours since then (about sixteen hours) worsening or progressing symptoms, warranting an emergency ophthalmological consult (standard of practice, nationally) Symptoms noted: photophobia, pain FBS, clear discharge, loss of vision Was not noted but that is inexplicable becaus a) I was not wearing glasses and my vision was very poor and b) an epithelial defect was Centrally on my left cornea. I do not recall And there is not mention of a visual Acuity exam. *** ***I think this alone says it all. algorithm Abrasion was not large; the ulcer Was measured at 4.5 cm D the next Day at Washington Eye. I verbally rated Pain as a “7” on a 1-10 scale noted in chart. Corneal Abrasions Corneal abrasions are defects of the normal corneal epithelium caused by trauma from small objects (often a fingernail, twig, hairbrush, or comb). They also occur after removal of a foreign body. Corneal abrasions from contact lenses represent a separate category with a unique set of clinical problems. In a one-year survey of admissions to a British emergency eye clinic, corneal abrasions accounted for 10% of the visits.54 Corneal abrasions are quite painful, and most people do not return to full functioning until the abrasion is healed. Patients describe immediate, sharp pain followed rapidly by tearing, photophobia, a decrease in visual acuity, and a persistent foreign body sensation. The eye will appear injected. Topical anesthetic drops will often significantly improve the pain, reduce blepharospasm, and allow a full examination. Fluorescein staining reveals the corneal defect. The magnification provided by a slit lamp allows a detailed quantification of the size as well as the depth of the lesion. The natural history of most abrasions is full healing in 2-3 days. Except in the cases of abrasions associated with contact lens use, infection occurs in fewer than 1% of cases. Until the mid-1990s, accepted therapy involved occlusive eye patches, antibiotic ointments (felt to be more soothing than drops), oral analgesics, and optional cycloplegics. The theory behind the occlusive patches was to provide a stable corneal environment to promote rapid reepithelialization. Patches were also thought to reduce pain. A meta-analysis by Flynn et al in 1998 that combined five randomized clinical trials showed no statistical difference in healing between patched and un-patched eyes, and no reduction in pain in patients whose eyes were patched.55 These trials, however, enrolled only patients with small- to moderatesized abrasions (< 10 mm2). Large abrasions seem to enjoy improved healing if patched.56 Unlike eye patching, topical NSAID drops may improve patient comfort. In one randomized, doubleblind, placebo-controlled trial of 100 patients with corneal abrasions, topical ketorolac 0.5% (Acular) was shown to reduce pain and photophobia significantly at the one-day mark. The ketorolac group was also able to return to function one day sooner, on average, than the placebo group. There was no difference in rates of healing or complications.56 A smaller study using diclofenac 0.3% (Voltaren) showed a small but statistically significant improvement in pain scale at two hours.57 The exact mechanism of action of these topical NSAIDs has not yet been delineated. It is probably some combination of reduction in pain sensation and antiinflammatory effect.56 For traumatic, non-contact lens abrasions with significant pain, Kaiser et al recommendketorolac 0.3% QID for three days or until the patient is comfortable, a broad-spectrum antibiotic ointment TID for three days or until the abrasion is healed, an optional shortacting cycloplegic such as cyclopentolate, and no patch (unless the abrasion is > 10 mm2).56 Many emergency physicians prescribe narcotic pain medicines for patients with corneal abrasions; these drugs are especially appreciated when the patient tries to go to sleep. Corneal abrasions in contact lens users represent a distinct problem. There are approximately 25 million contact lens wearers in the U.S. They are all at increased risk of developing infected abrasions—referred to as ulcerative keratitis. Overnight, extended-wear soft lenses carry a 10- to 15fold risk of infection. The causative organism is most often Pseudomonas species. The course can be fulminant, leading to permanent vision loss from corneal scarring. Do not patch corneal abrasions secondary to contact lens use. In 1987, Clemons et al reported six cases of Pseudomonas keratitis following pressure patching for contact-lensassociated corneal abrasions.58 The occlusive patch favors bacterial replication by raising corneal temperature and interfering in the normal protective effects of routine eye blinking, tear exchange, and tear movement. The treatment of contact-lens-associated abrasions should begin with an antibiotic ointment that covers Pseudomonas (such as gentamicin [Genoptic] or combination polymixin/bacitracin). Steroid combinations should be avoided, as they may favor bacterial replication. Follow-up within 24 hours should be arranged, because suppuration of the abrasions can occur rapidly. Contact lens use should not resume until the abrasion is fully healed.59 The offending lenses should be replaced or inspected carefully for evidence of damage. Note the pressure patching accelerated suppuration sot that it had occurred within 15 hours and probably much sooner.