Immunodeficiencies
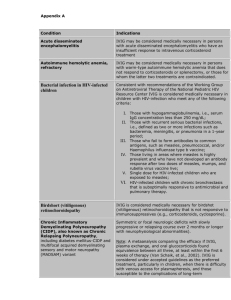
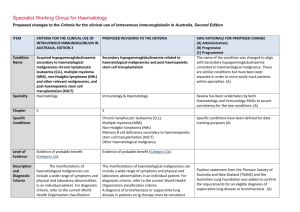
advertisement

Primary Immunodeficiencies Dr. Katia Sitnitskaya Host defense Innate immunity AG-specific immunity • Complement: alternative pathway • Complement: classical pathway AG + AB • Phagocytes: - neutrophils - macrophages • T cell response • B cell: AB production • Natural killers US: how many we are talking about ? Most common ? Complement cascade you DON’T HAVE TO remember Complement: - opsonization: C3b, C5b - chemotaxis: C3a, C5a - membrane attack: C5-9 Opsonization Chemotaxis Complement deficiencies: very rare (-) opsonins + chemotaxis Pyogenic infections Complement deficiency • C5-9 “terminal pathway” deficiency: 40% relapse of Meningoccal infection • 3 – 5% of cases of Meningococcal infection = complement deficiency • AB-sensitized sheep RBC: measurement of total hemolytic c. by classical pathway (CH50) • Unsensitized rabbit RBC; measurement of total hemolytic c. by alternative pathway (AH50) Deficiency Mechanism Infections CH50 C2 = most common opsonins Pyogenic in 1/5 (SLE) < 10% Properdin (Xp11) opsonins Pyogenic Normal (AH50 low) C5 - 8 chemotaxis membrane attack Recurrent N.men < 10% C9 membrane attack Recurrent N.men 50% Phagocytic disorders Phagocytic disorders LAD “Indigestion” = CGD, Chediak-Higashi Phagocytic Disorders: 1. “commuting” LAD: - the defect is a lack of a neutrophil adhesion molecule = no emigration into tissues. - presents with delayed separation of the umbilical cord, recurrent SBIs, leukemoid reactions Leukocyte adhesion deficiency (LAD) A. Normal neutrophils aggregate B. Neutrophils from a patient with LAD type 1 fail to aggregate in vitro C. Patients with LAD type 1 have periodontitis & recurrent GI, GU, and respiratory infections Congenital agranulocytosis Kostmann Disease • AR, 1: 1 000 000 • An abnormal G-CSF–induced intracellular signal transduction ? • ANC < 500/mm3 + normal WBC count because of the monocytosis. • Abnormal CD64+ (FCgRI receptor) on neutrophils • Mild anemia may be present from chronic inflammation. • + Hyper-g-globulinemia. • Mortality rate without Tx: 70% within the 1-st year of life • Tx: failure of G-CSF BMT, or stem cell transplantation. Phagocytic disorders 1. NADPH oxidase catalyzesreduction of O2 to superoxide anion (O–•2 ) 2. Superoxide dismutase convert it to H2O2 3. Neutrophil-derived myeloperoxidase (MPO) converts H2O2 into a HOCl–bleach Cl2 Clinical Features of CGD A. Inflammation of the nares. B. Large granuloma in the neck C. Severe gingivitis D. An esophageal stricture caused by a granuloma. Resolution after treatment with CSs Chediak-Higashi syndrome • AR, the long arm of chromosome 1 • The lysosomes fail to fuse with the phagosome. • Neutropenia + diminished chemotaxis + giant lysosomes • Dx: chemotaxis assay • Decreased NK functions. • The platelets are abnormal (easy bruising). • Oculocutaneous albinism, photophobia, enterocolitis and peripheral neuropathy. • BMT has been used with excellent results in several cases. • 85% of children with CHS, develop lymphoma-like condition which generally conduces to death. • Prenatal Dx: giant neutrophil granules in the fetal blood. Myeloperoxidase deficiency • Common 1 : 2000, AR • Dercreased intracellular killing (no bleach) • Absence of myeloperoxidase enzyme in neutrophil and monocyte granules. • MPO deficiency + diabetes mellitus = Candidal sepsis + osteo • Most patients are asymptomatic • Dx: chemoluminescence test • Vacuolized neutrophils Phagocytic disoders A. Normal peripheral blood smear B. Peripheral blood smear from a patient with the Chédiak–Higashi syndrome: large perinuclear granules. C. Peripheral-blood smear from a patient with agranulocytosis: the cytoplasm is pale, no granules are present, and nuclei are notched and hyposegmented. D. Nitroblue tetrazolium test (NBT) in normal neutrophils: phagocytosis results in dark-blue staining of the cytoplasm E. NBT in neutrophils from a patient with CGD: there is no phagocytosis = no dark-blue cytoplasmic staining. F. A hair from a patient with the Chédiak–Higashi syndrome in which giant granules are present, ( normal hair on thr right). Phgocytic disorders summary Common infections with GN and catalase (+), like Staph. aureus, Pseudomonas a. + Aspergillus. “Central” immunodeficiencies: bone marrow / thymic events RBC Platelets Granulocytes Monocytes Ag CR CR 3 Pre-B Common Lymphocyte Precursor CR = complement receptor; , = membrane IgM and IgD Ab-forming cells THY Pre-T IgM... B 1 Hematopoeitic stem cell TH,C,S 2 TH,TC,TS/R... T-effector T - cells LYMPHOCYTE DIFFERENTIATION 1. Bruton’s A-g-globulinemia: XR, chrom. Xq22 2. DiGeorge Syndrome = Thy. aplasia: microdelition, chrom. 22q 3. Severe Combined ImmunoDeficiency (SCID): multi-modal T cell disorders Severe combined ImmunoDeficiency (SCID) SCID Loss of the MHC molecule = “Bare lymphocyte syndrome”: no recognition of other cells SCID The only host defenses are: - Complement - Phagocytosis Maintenance: - Bactrim Px, Azithro Px - IVIG Salvage: - Recombinant ADA injections - BMT DiGeorge Syndrome: • Sporadic microdeletion of 22q “CATCH-22” Cardiac malf. Abnormal face • Hypertelorism, down-slanted eyes, + cleft palate (“midline defects”) Thymic hypopl. Cleft palate Hypo-Ca-emia Developmental defect of the 3-d & 4-th pharyngeal pouches • No thymus = low T cell counts • No parathyroid glands = hypo-Ca-emic seizures • CV: interrupted aortic arch & truncus arteriosus • Treatment: thymus transplant Ataxia-Telangiectasia • • AR, chromosome 11 1 case in 100,000 births • Single gene mutation results in impaired repair of DNA damage = cancer in1/4 ( lymphoma) • Usually presents in the 2-d year of life as a lack of balance and slurred speech. • Ocular telactasia before age of 6. Mild MR in 1/3 • Progressive cerebellar degeneration (CT: atrophy) + immunodeficiency in 2/3 + radiosensitivity (x-ray) • AFP, may be small thymus, dys-g-globulinemia ( Ig G2,4 & A) Wiscott-Aldrich disease • WASP gene on Xp11 chromosome = X-linked recessive • Defective cytoskeleton of T cells and platelets • TCP + Eczema + recurrent sino-pulmonary infections, HSV / CMV, PCP • Labs: small Plt, • Tx: IVIG T cells, B cells, BMT • Pre-natal Dx: EM of fetal lymphocyte Ig A & E, specific ABs IL-12 receptor deficiency Monocytes and macrophages bind IFN- g activation: 1. production of hydrogen peroxide (H2O2) 2. synthesis & release of IL-12 & tumor necrosis factor (TNF) A. Resolving mycobacterial infection with normal granuloma formation B. An AR mutation of the IFN-g receptor : mycobacteria survive in macrophages C. Same patient: no granuloma IL-12 produced by macrophages and dendritic cells in the presence of a pathogen, binds to its receptors on T cells and NK cells inducing the release of IFN-g T cell deficiencies: summary B cell disorders Bruton’s X-linked A-g-globulinemia • Absence or deficiency of a Bruton’s tyrosine kinase: maturation arrest of pre-B cells • Levels of all Ig levels are less than 10% of normal. • Infections start after 5 months of age: capsulated ( H. influenzae, Strep. pneumoniae, Giardia lamblia, ECHO viruses) . Tiny tonsils, • Molecular confirmation of the Dx: fluocytometry • Treatment: IVIG Selective Ig A deficiency • Most common immunodeficiency: 1: 700 in US • Some cases are AR. • 1 : 300 in atopic population • Majority of patients are clinically normal • Ig A < 5: recurrent / chronic sinopulmonary, GI, GU infections • Allergy, GI (celiac disease, UC), JRA, SLE • IgG is c/indicated unless IgG deficiency also present Hyper-E syndrome • Pruritic dermatitis (eczema) • Recurrent staphylococcal abscesses of skin, lung, joints, etc. • Eosinophilia of blood and sputum • Ig G, M, A usually normal • Extremely high Ig E > 1000 , high Ig D • Diminished response to immunization • Poor cellular and humoral response to neoantigens • Tx: IVIG BMT T helper Hyper-M X-linked disorder Patients have abnormal CD4 ligand on T cells, and can not properly signal B cells Thus, this is really a T cell problem; the B cells work fine Block in switching from Ig M to IgG, IgA, IgE B cell Hyper-M X-linked disorder • X-linked recessive: Xq26 + sporadic cases • Recurrent pyogenic, mostly sinopulmonary, infections • Sclerosing cholangitis • Increased incidence of autoimmune and lymphoproliferative disorders • Low Ig G & Ig • Neutropenia, TCP, anemia • Tx: IVIG Common Variable Immune Deficiency (CVID) • AD / X-linked • Onset after 10 y., recurrent sinopulmonary infections & other pyogenic Lymphadenopathy and splenomegaly may be present • IL-2, IFN-g, CD40L (defective CD4 function ) • IgG < 50% (< 250), Ig A & M • No specific Ab production / no response to vaccines • Anti - B cell autoantibodies • Patients may have a higher occurrence of atopic / rheumatalogic diseases, lymphoid hyperplasia • Treatment: IVIG to keep IgG > 400 Transient hypo-g infantorum • Delayed onset of IgG synthesis, but always > 200 • Physiological nadir of IgG level 430 – 660 @ 4 – 12 mo. Of age • Onset of symptoms coincides with decline in matrnal IgG level • Normal levels of Ig A & M • Normal IgG response to immunization • Mature B cells & plasma cells are present • Resolves by 24 – 36 months of age B cell disorders summary Examples of Infectious Agents in Different Types of Immune Deficiencies Pathogen Type Bacteria T-Cell Defect Bacterial Sepsis B-Cell Defect Streptococci, Staphylococci, Haemophilus Viruses CMV, EBV, varicella, chronic respiratory & GI infections Enteroviral encephalitis Fungi & Parasites Candida, PCP Giardiasis Special Features OIs failure to clear infections Recurrent sinopulmonary infections, sepsis, chronic meningitis Granulocyte Defect Staphylococci, Pseudomonas Candida, Nocardia, Aspergillus Complement Defect Neisseria, pyogenic bacteria Warning Signs of Primary Immunodeficiency Disorders Medical history • • • • > 8 ear infections / year > 2 serious sinusitis / year > 2 pneumonias / year > 2 deep-seated infections, or infections in unusual areas Physical signs • Poor growth, FTT • Absent lymph nodes or tonsils • Skin lesions: telangiectasias, petechiae, lupus-like rash • Recurrent deep skin/organ abscesses • Ataxia (ataxia-telangiectasia) • Need for IV ABx to clear infection • Infections with unusual /opportunistic organisms • Family Hx of primary immunodeficiency • Oral thrush after1 year of age • Oral ulcers Table 1. Indications for immune evaluation Infection frequency Infection type Single episode Osteomyelitis Septic arthritis Meningitis Two episodes Sepsis Pneumonia Multiple episodes Sinusitis Bronchitis Pneumonia D. Dube et al, POSTGRAD MED, 2002 Table 4. Tests of immunologic functions Initial Advanced Cellular immunity CBC: ANC & ALC Lymphocyte subsets Candida skin test LPA, CTL activity, Cytokine production ADA level Humoral immunity Serum Ig G, A, M, E Diphth / Tetanus and Pneumoc. titers IgG 1 - 4 subclasses B-cell quantitation In-vitro AB production Phagocytic function CBC, NBT test FACS = H202 (for CGD) Chemoluminescence assay (for M-p-o) Chemotaxis assay (for C-H) CD 11 / 18 (LAD) Complement Total Hemolytic Complement assay: Quantitation of individual complement components and regulatory molecules Classical = CH50 Alternative = AH50 Serum opsonic and chemotactic assays Workup for suspected P.I.D. IVIG is indicated for: - Bruton’s a-g-globulinemia - Hyper-M & Hyper-E - CVID & Ig subcl. = if NO SPECIFIC Abs ! - SCID & Wiscott-Aldrich Indications for BMT: • Hyper-E syndrome • SCID • Wiscott-Aldrich • Chediak-Higashi • Kostmann Disease Selected causes of secondary immunodeficiency diseases Causes Examples Malnutrition Protein / energy malnutrition, malabsorption syndrome Infection HIV, congenital CMV / EBV / Toxoplasma Drugs Corticosteroids, Phenytoin, Sulfasalazine, Cytotoxins Chronic medical conditions Sickle cell disease, cystic fibrosis Malignancy ALL, AML, lymphomas Protein (Ig) loss Protein-losing enteropathy, nephrotic syndrome Chromosomal syndromes Down syndrome