N Engl J Med
advertisement
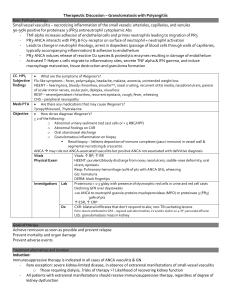
BSR Course, Oxford, 2011 Treatment of Vasculitis: immunesuppressives and biologics David Jayne Vasculitis and Lupus Clinic Addenbrooke’s Hospital Cambridge UK Principles • Identify drives – Infection, drugs, malignancy • Induce and maintain remission • Minimise drug toxicity ‘Standard’ therapy: ‘add-on’ therapy IV methyl prednisolone Plasma exchange Intravenous immunoglobulin TNF blockade ? improve effective + reduce toxicity Prednisolone CYC 0 AZA/MTX 3 6 9 12 15 18 24 months CYC; cyclophosphamide, AZA; azathioprine, MTX; methotrexate Reduce cyclophosphamide exposure Switch to alternative on remission IV pulse instead of daily oral Alternative induction for non-severe disease 4 Generalised (CYCAZAREM) Remission Relapse 1.0 .9 .8 Group Cyclophosphamide Survival .7 Azathioprine .6 0 2 4 6 8 10 12 14 16 Time from remission to relapse (months) Oral CYC + prednisolone Continued CYC vs. AZA Jayne, N Engl J Med 2003 CYCLOPS de Groot et al, Ann Int Med 2009 Early systemic (NORAM): methotrexate (MTX) vs. cyclophosphamide (CYC) Remission Relapse 91.5 95.5 Survival to first relapse % Survival to 1st relapse 1.0 .9 .8 .7 .6 .5 .4 LIMB .3 MTX Cyclophospham .2 .1 Methotrexate CYC 0.0 0 2 4 6 8 10 12 14 16 18 20 P = 0.02 Months from entry EUVAS de Groot et al, Arthritis Rheum 2005 Generalised vasculitis – cyclophosphamide (3-6 months) Time toTime remission, BVAS =0 to remission Recovery of renal function 1.0 80 .8 Glomerular filtration rate (ml/min) 70 .6 .4 .2 0.0 0 2 4 6 8 60 LIMB Daily oral 50 Pulse 40 10 12 14 16 0 18 3-6 18 Time (months) Months from entry De Groot, ASN 2006 Jayne, New Eng J Med 2003 Evidence based recommendations • EULAR recommendations for conducting clinical studies and/or clinical trials in systemic vasculitis: focus on ANCA-associated vasculitis. Ann Rheum Dis. 2007;66:605-617. • EULAR Recommendations for the management of primary small and medium vessel vasculitis. Ann Rheum Dis. 2008;68:310-317. • EULAR Recommendations for the management of large vessel vasculitis. Ann Rheum Dis. 2008;68:318-323. • www.vasculitis.org EUVAS EUVAS Remission maintenance Azathioprine ≅ methotrexate How long ? 10 Less cyclophosphamide increases relapse risk 0.00 0.25 0.50 0.75 1.00 IMPROVE: Cumulative Incidence of Relapse 0 1 2 3 4 5 Time (years) AZA th MMF Hiemstra, Am Soc Nephrol 2009 Newer therapies, Biologic or nonBiologic ? • • • • • • IVIg Anti-TNF Rituximab ATG Alemtuzumab Abatacept • Mycophenolic acid – Mycophenolate mofetil (Cellcept) – Enteric coated MPA (Myfortic) • Leflunomide • Deoxyspergualin Rituximab Rituximab for refractory vasculitis n = 63 Jones, Arthritis Rheum 2009 Rituximab in ENT/eye disease (n=32) Pre-RTX Post-RTX Martinez del Pero et al, Clin Otolaryngol 2009 Rituximab - Randomised Trials in AAV • RITUXVAS (EUVAS) – New, with renal involvement – N=44 – 12 month data reported 2008 • RAVE (US) – New/relapsing renal/non-renal – N=197 – 6 month data reported 2009 RITUVAS - Baseline Characteristics Patients Age PR3/MPO-ANCA GFR (ml/min/1.73m2) RTX 33 68 20/13 25 CYC 11 67 5/6 15 Both 44 68 25/19 21 Dialysis 24% 9% 20% Jones, New Engl J Med 2010 RITUXVAS – remission (BVAS = 0 for 6 months) Time to Remission CYC Sustained remission 25/33 (76%) 9/11 (82%) No sustained remission 2 incomplete response 1 incomplete response 6 deaths 1 death 0.00 0.25 0.50 0.75 1.00 RTX 0 100 200 Time (days) Cyclophosphamide 300 400 Rituximab Jones, New Engl J Med 2010 RITUXVAS – safety 21 (39%) 7 (21%) 0.66/pat yr 0.60/pat yr 6 (18%) 2 (18%) 1.00 0.75 Infections Death 12 (36%) 1.1 /pat yr 0.50 31 (42%) 1.0 /pat yr 0.25 SAEs 0.00 CYC Proportion Free of SAE RTX Time to first SAE 0 50 100 150 200 Time (days) CYC 250 300 350 RTX Jones, New Engl J Med 2010 Relapse RTX N=33 CYC N=11 7 (21%) 2 (18%) Major 1 (3%) 2 (18%) Minor 6 (18%) 0 (0%) Relapse Jones, ACR/ASN 2010 RAVE = US trial RAVE design • 197 new (49%) or relapsing WG/MPA creatinine < 4.0mg/dl, no lung haemorrhage • Randomised, double-blind rituximab 375mg/m2/wk x4 vs. oral CYC • Primary end-point remission and steroid withdrawal at 6 months Stone J et al, N Engl J Med 2010 % patients RAVE – remission rates p=ns p=ns * p=0.01 Stone J et al, N Engl J Med 2010 RAVE results • Efficacy – Nephritis and alveolar haemorrhage similar response • Safety – Similar AE rates • 18 month data end 2010 Stone J et al, N Engl J Med 2010 • Dosing • Concomitant medication • Biomarkers Cambridge retrospective survey • Non-protocol (n=34) – 82% full remission – 15% partial remission – 3% treatment failure • Protocol (n=72) – 93% full remission – 4% partial remission – 3% treatment failure Jones, ACR/ASN 2010 Relapse • 24 months – Non-protocol 71% – Protocol 22% End of follow-up – – Non-protocol 76% Protocol 29% Jones, ACR/ASN 2010 Take home messages Cyclophosphamide induction has been optimised Remission maintenance with AZA or MTX, MMF less effective Rituximab alternative to CYC and preferred for relapsing/refractory disease. ? Maintenance of remission after RTX Thank you