103.
advertisement

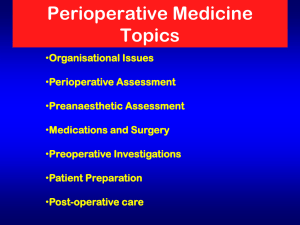
Pre Operative Clearance for Non Cardiac Surgery: ALL CLEAR Dominique Renee Abell, RN, MSN, CCRN, ACNP-BC (ACLS, PALS, TNCC) rbeckum@crossroadsdevelopers.com OBJECTIVES 1. Outline evidence based practice guidelines related to pre operative evaluation for surgery 2. Describe conditions that require pre operative diagnostic evaluations 3. Review the findings that would postpone or cancel surgery “The purpose of preoperative evaluation is not simply to give medical clearance but rather to perform an evaluation of the patient's current medical status, make recommendations concerning the evaluation, management and risk of cardiac problems over the entire perioperative period; and provide a clinical risk profile that the patient, primary physician, anesthesiologist and surgeon can use in making treatment decisions that may influence short term and long term cardiac outcomes” . Goals of Preoperative Evaluation Documentation for which surgery is needed Assessment of patient overall condition/health status Uncovering issues that could cause problems during and after surgery Perioperative risk determination Optimize medical condition to reduce morbidity and mortality Develop perioperative plan of care Goals of Preoperative Evaluation Education of patient and family Surgery Anesthesia Intraoperative care Post operative pain control Reduce anxiety Facilitate recovery Goals of Preoperative Evaluation Reduce cost Decrease length of stay Reduce cancellations day of surgery Increase patient/family satisfaction Nurse Practitioner Responsibilities Perform complete History and Physical Review/Order labs and ancillary studies Assess risk related to patient's co-morbidities Assess need for preoperative specialty consults Communicate with anesthesia provider and surgeon Assist with optimal timing of surgery Medically optimize patient condition preoperatively Situation for Surgery Emergent: life threatening situation, risk of or death of patient if not preformed Urgent: life threatening or debilitating, needs to be done sooner than later Elective: patient may “need” procedure but can be scheduled at any time Cardiac Risk Definition: Combined incidence of cardiac death and nonfatal myocardial infarction Focus on cardiac and pulmonary risk factors that can contribute to complications Determine patient's functional capacity, Metabolic equivalent (MET) Cardiac Risk ACC/AHA guidelines ASA guidelines Lee's Revised Cardiac Risk Index http://www.statcoder.com/cardiac.htm Cardiac Risk Indices Factors associated with life threatening cardiac complications/perioperative cardiac death MI within 6 months S3 gallop or jugular venous distention Age >70 ECG other than Sinus Rhythm, >5 PVC's/min Aortic Stenosis Poor general health/medical status Emergency surgery Intraperitoneal, intrathoracic, aortic surgery Different Levels of Risk High: Unstable Coronary Symptoms- acute or recent MI with evidence of ischemia Unstable or Severe Angina Decompensated Heart Failure Symptomatic/Significant Arrhythmias High Grade Atrioventricular Block Severe Valve Disease Intermediate: Mild Angina Previous MI Compensated or History of Heart Failure Diabetes Mellitus Renal Insufficiency Minor: Advanced Age Abnormal ECG Any other Rhythm besides Sinus Low functional Capacity History of Stroke Uncontrolled Hypertension Primary car provider patient surgeon anesthesiologist History and Physical Medical history-past and current Review of Systemscardiac risk factors, cardiac conditions, associated diseases, changes in symptoms Medication Vital signs Central and Peripheral pulses Lungs/Cardiac Auscultation/Palpation Abdominal palpation Examine Lower Extremities Alcohol, Tobacco, NonFunctional Capacity Prescribed drugs History and Physical Surgical History Allergies Family History of adverse reaction to anesthesia Studies- CBC, INR, aPTT, BMP/CMP,ECG, CXR, Stress Test, PFT, ECHO, Cardiac Cath, Children include birth historypremature,perinatal complications, congenital, chromosomal, anatomic malformations Functional Capacity 1 Metabolic Equivalent (MET) Can you take care of yourself? ADL's- eat, dress,toilet, Walk indoors around the house Walk a block or two on level ground 2-3 mph Do light houseworkdusting, wash dishes Functional Capacity 4 MET Can you climb a flight of stairs or walk up hill Walk on level ground at 4mph Run a short distance Heavy housework-scrub floors, lift or move heavy furniture Moderate recreational activities-golf,throwing a football Functional Capacity >10 MET Swimming, singles tennis, football, basketball, skiing Management of Cardiac Risk Continue current medications Cardio-protective Beta Blockade Coronary angiography/revascularization Pulmonary Complication Definition: revised to clinically significant Pneumonia Respiratory failure with prolonged mechanical ventilation Bronchospasm Atelectasis Exacerbation of underlying lung disease Pulmonary Complications Decreased functional residual capacity/vital capacity Cough Aspiration pneumonia Atelectasis Pneumonia Smoking- even in absence of lung disease Pulmonary complications Procedure specific risk factors Surgical site- most important risk factor Duration Anesthesia Neuromuscular blockade Pulmonary Complications COPD/Asthma Goal is “Personal Best” Poor PFT's do no exclude from surgery or correlate with risk of post operative complications Poor exercise capacity is probably best predictor Along with type and duration of surgery Age and obesity are not independent risk factors Metabolic markers- BUN>30, albumin <3 Pulmonary Complications Reducing Risk Preoperative smoking cessation 8 weeks prior Treat airflow obstruction in patients with COPD/Asthma Administer antibiotics and delay surgery Begin patient education regarding post op lung expansion maneuvers Pulmonary Complications Intraoperative Surgery less than 3 hours Spinal or epidural Regional or local blocks Avoid pancuronium Minimally invasive as possible laparoscopic Pulmonary Complications Post Operative Turn, Cough, and Deep Breath Early mobilization Adequate analgesia Incentive Spirometer/Acapella valve Continuous Positive Airway Pressure (CPAP) Epidural analgesia Intercostal nerve blocks Hematologic Risk Hematocrit < 24% Thrombocytopenia <50,000 History of bleeding diathesis Cirrhosis Hematologic malignancy Antiplatelet medication Anti-coagulation therapy DVT/VTE prophylaxis Chronic Medications Consider every medication/supplement Diabetes- adjust insulin or oral hypoglycemics Chronic steroids- stress dose Hypertensive medications- PO or IV Anti-ischemic medications- transdermal or IV Alcohol use and withdrawal Chronic Medications Monoamine oxidase inhibitors- taper and withdraw 2-3 weeks before surgery Oral contraceptives- stopped 6 weeks before elective surgery secondary to increased VTE risk Herbal supplements discontinued 2 weeks before surgery Aspirin discontinued 7-10 days before Thienopyridines (clopidogrel) 2 weeks before Non-steroidal Anti-inflammatories 7-10 days before Chronic Medications Oral anticoagulants stopped 4-5 days INR 1.2-1.5 before surgery Evaluate for “bridge therapy” Cox 2 inhibitors may be continued up to surgery References: Barnett,MD, S. (2013, December 12). Anesthesia for the older adult. Retrieved from www.uptodate.com Cohn, MD, FACP,S., Aronson, MD, M., Macpherson, D., (2013, June 28). Overview of the principles of medical consultation and perioperative medicine. Retrieved from www.uptodate.com Conde, MD, M., & Moody, Jr, MD, J. M. (2012, Oct 02). Noncardiac surgery in patients with mitral or aortic regurgitation. Retrieved from www.uptodate.com Flood, MD, C., Fleisher, MD, L. (2007). Preparation of the cardiac patient for noncardiac surgery. American Academy of Family Physicians,75(5), 656-665. Retrieved from www.aafp.org Greenland, P., Alpert, J., Beller, G., Benjamin, E., Burdoff, M., Fayad.., Z., Tarkington, L., & Yancy, C. (2010). 2010 accf/aha guideline for assessment of cardiovascular risk in asymptomatic adults. Journal of American College of Cardiology, 56(25), e50-103. Retrieved from http://wwwguideline.gov/content.aspx?id=23510 Hogue, MD, C., & Blakemore Hensley, MD, N. (2014, Jan 13). Anesthesia for patients needing urgent surgery after a recent cardiac event. Retrieved from www.uptodate.com Hughes, CPC, C. (2007). A refresher on coding consultations. Family Practice Management, 14(3), 37-45. Retrieved from http://www.aafp.org Lawerence, MD, V., Cornell, MD, J. E., & Smetana, MD, G. W. (2006). Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: Systematic review for the American College of Physicians. Annals of Internal Medicine, 144, 596-608. Retrieved from http://annals.org Lee, MD, P., Rabkin, MD, M. Medical assessment of the perioperative patient: Preoperative assessment. Retrieved from http://www.medicineclinic.org Olson, E. (2013, April 30). Surgical risk and the preoperative evaluation and management of adults with obstructive sleep apnea. Retrieved from www.uptodate.com Shammash, MD, J., Kimmel, MD, MS, S., Morgan, MD, PhD, Morgan, J. (2013, November 20). Estimation of cardiac risk prior to noncardiac surgery. Retrieved from www.uptodate.com Shammash, MD, J., Kimmel, MD, MS, S., Morgan, MD, PhD, Morgan, J., Devereaux, MD, PhD, P. (2014, February 4). Management of cardiac risk for noncardiac surgery. Retrieved from www.uptodate.com Schumann, MD, R. (2013, November 26). Perianesthesia medical evaluation of the obese patient. Retrieved from www.uptodate.com Smetana, MD, G. (2014, Jan 13). Preoperative medical evaluation of the healthy patient. Retrieved from www.uptodate.com Smetana, M, D, G., Lawrence, MD, V., & Cornell, PhD, J. E. (2006). Preoperative pulmonary risk stratification for noncardiothoracic surgery: Systematic review for the American college of physicians. Annals of Internal Medicine, 144, 581-595. Retrieved from http://annals.org Smetana, MD, Lawrence, MD & Cornell, PhD, 2006) Qaseem, MD, PhD, MHA, A., Snow, MD, V., Fitterman, MD, N., Horbake, MD, E. R., Lawrence, MD, V., Smetana, MD, G. W., & Weiss, MD, K. (2006). Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: A guideline for the American college of physicians. Annals of Internal Medicine, 144, 575-580. Retrieved from http://annals.org Stannard, D., & Krenzischek, D. (2012). Peri anesthesia nursing care: A bedside guide for safe recovery. Sudbury, MA: Jones and Barlett Learnig Qaseem, MD, PhD, MHA, A., Snow, MD, V., Fitterman, MD, N., Horbake, MD, E. R., Lawrence, MD, V., Smetana, MD, G. W., & Weiss, MD, K. (2006). Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: A guideline for the American College of Physicians. Annals of Internal Medicine, 144, 575-580. Retrieved from http://annals.org (Qaseem, MD, PhD, MHA, Snow, MD, Fitterman, MD, Horbake, MD, Lawrence, MD, Smetana, MD & Weiss, MD, 2006) Rothenberg, MD, M. A. (2005). Laboratory tests made easy: A plain English approach. Eau Claire, Wisconsin: Pesi Healthcare.(Qaseem, MD, PhD, MHA, Snow, MD, Fitterman, MD, Horbake, MD, Lawrence, MD, Smetana, MD & Weiss, MD, 2006) Zambouri, A. (2007). Preoperative evaluation for anesthesia and surgery. Hippokratia, 11(1), 13-21.