Patient Information: Setting up a new service
advertisement
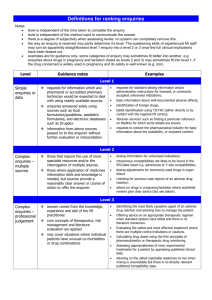
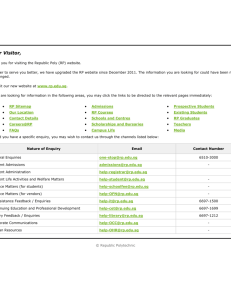
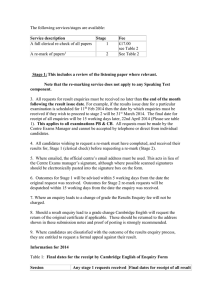
Patient Information: Setting up a new service Pitfalls & Pluses Paul Stevenson Our Service Signposting • We do not produce new material. • Signpost patients to appropriate existing high quality services and information. • Advice staff who are producing specific internal patient information leaflets and products. Quality Assured Information • Certified source : Information Standard • Assess using tool such as DISCERN (www.discern.org.uk) • Discuss with specific healthcare professionals How do we deliver the service • • • • Web Site Telephone Email In Person • Work with wider community • Work with internal staff Web Site We link to a lot of existing material USP - Localisation Access Routes • Web Site is getting approximately 2,000 hits per month. • Difficulty in measuring what that actually means, or the impact . • Far more email enquiries than telephone or in person enquiries. (approx 80% by email) • Direct enquiry levels are still lower than we anticipated: approx 8 per month. Why Offer Face to Face and Telephone Enquiries • We can spend longer with patients. Clinicians and GPs often do not have sufficient time to discuss in depth. • Often not the patient but relative or carer who wants the information. • Often enquiry is prior to contact with a healthcare professional. Book Stock • Fast Facts Series • BMA : Understanding/ Family Doctor series • Medical Dictionary/Encyclopaedia • Good basic visual physiology and anatomy text Setting Up The Service – Reflections • Objectives and Aims “We need a patient information Service” – Difficult to get exact measurable objectives from Executives. – Cost savings through reducing re-admissions. – Supporting long-term condition pathway. Limitations we knew about in advance • Budget A few thousand pounds. Limited scope for what service can do. • Location Within current healthcare library Limited patient footfall or ‘drop in’ opportunities • Staffing One full time member of staff Limited outreach and community involvement work • Patient Information Strategy I wrote one Lacked clear specific objectives or outcomes • IT NHS block on social media and advanced web functions. Enquiries – What we Expected • General enquiries about specific conditions & treatments • The kind of thing that’s on NHS Choices: Enquiries – What we Actually Get • More orientated to local service provision: “I’m claustrophobic, is your MRI scanner enclosed or open?” Layers of Enquiry • Patient has bladder weakness • Asked for information on “exercise at home” as unable to go far or do vigorous exercise without incontinence issues. • Actually wanted information about dealing with incontinence Active Listening • Sometimes people just want to be listened too… Set Boundaries Explicitly document what is expected of the service. Will you give information that differs from local practice? – i.e. Give details of a drug that is prohibitively expensive. – i.e. Give details of a surgical technique that is not used in the local hospital – i.e. Give details of off-label drug use such as Avastin for AMD www.rcpsych.ac.uk/pdf/General%20-201.45%20Staff%20%20Patient%20Boundaries%20%20Relationships_Ashen%20Hill%20East%20Sussex.pdf – Code of Conduct / Professional Standards – Is it OK to accept gifts of thanks ; or start friendships with patients ? – What support should staff expect to be in place for them? Setting Boundaries • Enquiry – woman wanted details of local private options for abortion. • Was her 20th abortion , used as method of birth control. How do you best answer this enquiry? • • • Do you supply the details requested Give information on alternative methods of birth control Is this a safeguarding adults issue – is there possibly an abusive scenario here? Do your staff know there responsibility for safeguarding adults/children? Setting Boundaries • Enquiry –man wants details of European countries that offer euthanasia. How do you best answer this enquiry? • Do you give the information requested ? • Do you give information on palliative care and end of life planning ? • Do you refuse to answer the enquiry stating referral to more expert healthcare professionals is needed ? – Counselling – End of life /Palliative care team Set Boundaries Explicitly document what is expected of the service. – Information –vs- advice – What depth – Will you clarify the meaning in statistical data? – Will you supply journal article/research level information? – At what point do you ‘refer’ to other services , what is the referral process? Good Governance • Record patient enquiries – Useful for service evaluation – Evidence in any legal proceedings – NHSLA • Standard operational Procedures (SOP) & Guidelines – Protects & supports staff delivering the service – Indicates the level of service expected – Gives patients consistency of service What worked • Email enquiries • Specific Focus on local information and support • Patient Information prescriptions & Integration with care-pathways • Starting small and gradually growing What we would do differently 1. Establish clear objectives & outcomes 2. Identify physical location that is prominent and easily accessible to patients. 3. Have SOP and guidelines in place prior to service starting. 4. Ensure staff delivering service are confident and have opportunities for training . Further Information • Contact me if you have any questions or want to visit • Paul.Stevenson@anhst.nhs.uk