Ventricular Septal Defect - Universitätsklinikum Hamburg
advertisement

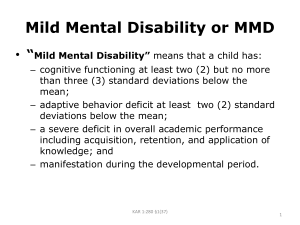
Klinik für Kinderherzchirurgie Cyanosis or Congestive Heart Failure in Children: Murmurs of Shunts, Stenosis, and Insufficiency A. Dodge-Khatami, MD, PhD Chief of Pediatric Cardiac Surgery Head of Program for Congenital Heart Disease University Heart Center – UHZ University of Hamburg-Eppendorf School of Medicine Hamburg, Germany Klinik für Kinderherzchirurgie even rare congenital heart defects will be seen once in your careers (0.8% of all births); how should you react? most important objective: distinguish between a blue and pink patient with a murmur and understand why! Klinik für Kinderherzchirurgie Shunts: Location + Direction • • • Intra or extra-cardiac? Which heart chambers are affected? Qp/Qs = pulmonary / systemic flow ratio Qp = VO2 / pulm Vv O2 – PA O2 Qs = VO2 / Vv O2 – Ao O2 • In the absence of a shunt, Qp/Qs = 1 Klinik für Kinderherzchirurgie Normal circulation Q = P/R Qp/Qs = 1 Klinik für Kinderherzchirurgie Shunts: Direction • Left >>> right or Right >>> left? Which is more probable? Why? • Left > right : PDA, ASD, VSD, AVSD, AP window, Truncus, PAPVD, TAPVD • Right > left : right inflow or outflow obstruction + intra-cardiac shunt: Tricuspid atresia (TA)/Tricuspid Stenosis (TS), Pulmonary Atresia/Pulmonary stenosis, TOFallot Klinik für Kinderherzchirurgie Shunts: Direction • Left >>> right : VSD Left >> right shunt Qp/Qs > 2 - 3 Pressure + Volume Overload Klinik für Kinderherzchirurgie Shunts: Physiology Left >>> right: • • • • LV volume overload Increased pulmonary flow, pulmonary infections Pulmonary Hypertension (PHN), severity and degree according to shunt size Bacterial endocarditis Right >>> left: • • • RV pressure overload + strain Cyanosis Polyglobulia Klinik für Kinderherzchirurgie Shunts: Treatment Left >>> right: volume restriction, diuretics, inotropes, permissive hypercapnea ventilation (hypoventilation), shunt closure Right >>> left: hydration, (transfusion), hyperventilation, increase pulmonary blood flow +/- shunt closure Klinik für Kinderherzchirurgie Shunts: Operative Indications L >> R: • Symptoms: tachycardia, tachypnea, hepatomegaly, sweating during feeds, failure to thrive • Qp:Qs > 1.5 • Aortic valve prolapse +/- insufficiency R >> L: • cyanosis, RVH + strain Klinik für Kinderherzchirurgie 5 most common congenital heart defects? Klinik für Kinderherzchirurgie 5 most common congenital heart defects? Ventricular Septal Defect (VSD) 30% Patent Ductus Arteriosus (PDA) 10% Coarctation (coA) 5-8% Atrial Septal Defect (ASD) ~ 8% Tetralogy of Fallot (TOF) 5-10% Klinik für Kinderherzchirurgie • case: blue child (10 years old) with a murmur (where?) auscultation: holosystolic murmur at precordium saturations: ? Cyanosis: central or peripheral? „Hippocratic fingers“- Clubbing Central: intracardiac shunt + obstruction to pulmonary blood flow Peripheral: Chronic Pneumonia, Chronic Interstitial Lung Disease, Pulmonary Neoplasia, Circulatory Collapse (+Peripheral Vasoconstriction) next step ? Klinik für Kinderherzchirurgie x-ray: differential diagnosis? Klinik für Kinderherzchirurgie x-ray: • • next step ? prominent central pulmonary markings black peripheral lung fields Klinik für Kinderherzchirurgie echocardiography: Cardiomegaly, biventricular dilatation + hypertrophy Diagnosis ? Klinik für Kinderherzchirurgie echocardiography: Cardiomegaly, biventricular dilatation + hypertrophy VSD: why is the child blue? Klinik für Kinderherzchirurgie Right >> Left shunting = Cyanosis > increased cellularity (muscular and interstitial) >> fixed pulmonary vascular resistance = Eisenmenger syndrome Klinik für Kinderherzchirurgie Patent Ductus Arteriosus (PDA) Klinik für Kinderherzchirurgie Patent Ductus Arteriosus (PDA) • continuous „machinery“ murmur • LV hypertrophy + LA dilatation Increased pulmonary vascular markings, interstitial pulmonary edema • failure to thrive • recurrent upper respiratory infections • fatigue with exertion • tachypnea, tachycardia, heart failure Klinik für Kinderherzchirurgie Portsmann, 1967 Patent Ductus Arteriosus (PDA) R. Gross, Boston, 1938 Klinik für Kinderherzchirurgie Coarctation (coA) Klinik für Kinderherzchirurgie Coarctation (coA) • bi-modal presentation: newborns in cardiovascular shock: ductal-dependent (PGE1) vs. „asymptomatic“ hypertensive children: headaches, epistaxis Klinik für Kinderherzchirurgie Coarctation (coA) • mid-systolic murmur in the back, systolic or continuous murmurs on the lateral chest walls (collaterals), diminished femoral pulses • Left Ventricular hypertrophy, myocardial infarction • circle of Willis aneurysms, aortic aneurysms, aortic dissection, aortic rupture • average age at death ~ 35 years if untreated : congestive heart failure (1/4), bacterial endocarditis (1/4), spontaneous rupture of the aorta (20%), intracranial hemorrhage (13%) Klinik für Kinderherzchirurgie Coarctation (coA) C. Crafoord, Stockholm, 1944 End-to-end anastomosis Klinik für Kinderherzchirurgie Voßschulte, 1957 Patch plasty Coarctation (coA) Gross, 1951 Interposition graft Waldhausen, 1966 Subclavian flap Klinik für Kinderherzchirurgie Coarctation (coA) : results Mortality: 4-14%, age-dependent Complications: • hypertension, chylothorax, recurrent nerve paresis (stridor) • recurrent coA ~ 10-15% if surgery in the newborn period, >> balloon dilatation • paraplegia • aneurysm Klinik für Kinderherzchirurgie Atrial Septal Defect (ASD) • systolic murmur, fixed split second heart sound (prolonged flow time on the right – delayed closure of the pulmonary valve) • Dilated right atrium + ventricle • Pulmonary hypertension recurrent upper respiratory infections • atrial arrhythmia (flutter, fibrillation) • congestive heart failure • no risk of bacterial endocarditis Klinik für Kinderherzchirurgie Atrial Septal Defect (ASD) F.J. Lewis, Minneapolis, 1952, inflow occlusion King, 1976, device closure Klinik für Kinderherzchirurgie Atrial Septal Defect (ASD) J. Gibbon Jr., Rochester, father of cardio-pulmonary bypass, 1934-53 Klinik für Kinderherzchirurgie Atrial Septal Defect (ASD) J. Gibbon Jr., Rochester, 1953 Klinik für Kinderherzchirurgie Atrial Septal Defect (ASD) : results • Gibbon (1953): first success, followed by 5 deaths, abandonned surgery and requested a 1 year moratorium on his bypass machine… • current: mortality ~ 0% Klinik für Kinderherzchirurgie Ventricular Septal Defect (VSD) most frequent CHD ~ 30% Klinik für Kinderherzchirurgie Ventricular Septal Defect (VSD) • Holosystolic murmur, increased pulmonary vascularity on x-ray, • Cardiomegaly, biventricular dilatation + hypertrophy. • Dyspnea, sweating during feeding, failure to thrive. • Recurrent upper respiratory tract infections. Klinik für Kinderherzchirurgie Ventricular Septal Defect (VSD) Untreated: • 25-40% spontaneous closure > 2-3 years • endocarditis (0.3% per year) • pulmonary hypertension > pulmonary arteriolar wall thickening • increased PVR, reversal of shunt = Eisenmenger syndrome • cyanosis (by 1-2 years of age) • death Klinik für Kinderherzchirurgie Ventricular Septal Defect (VSD) Klinik für Kinderherzchirurgie Ventricular Septal Defect (VSD >>> VSD) • increased cellularity (muscular and interstitial) • increased reactivity • fixed contraction • vascular wall sclerosis >> fixed pulmonary vascular resistance = Eisenmenger syndrome Klinik für Kinderherzchirurgie Ventricular Septal Defect (VSD) C.W. Lillehei, Minneapolis 1954: VSD „King of Hearts: the True Story of the Maverick Who Pioneered Open Heart Surgery “, G.W. Miller Cross-circulation: father as oxygenator, but potentially 200% mortality… Klinik für Kinderherzchirurgie Ventricular Septal Defect (VSD) C.W. Lillehei, Minneapolis 1954: VSD 28/47 patients survived:~ 40% mortality Klinik für Kinderherzchirurgie Ventricular Septal Defect (VSD) Klinik für Kinderherzchirurgie Ventricular Septal Defect (VSD): Results mortality ~ 1-2% heart block > pacemaker 1-2% long-term prognosis excellent! Klinik für Kinderherzchirurgie Ventricular Septal Defect (VSD): palliation PA banding • multiple VSDs • small baby, failure to thrive Muller / Damman, 1952 Klinik für Kinderherzchirurgie Tetralogy of Fallot (TOF) most frequent cyanotic CHD ~ 10% 1. Overriding Aorta 2. Ventricular Septal Defect 3. Right ventricular hypertrophy 4. Right Ventricular Outflow Tract Obstruction (RVOTO) Klinik für Kinderherzchirurgie Tetralogy of Fallot • systolic murmur • right aortic arch (25%), „boot shape“ heart • right ventricular hypertrophy • cyanosis, tet „spells“: dynamic RVOT contraction • clubbing (after 6 months), dyspnea, exercise intolerance • brain abscess • polycythemia > pulmonary + cerebral thrombosis Klinik für Kinderherzchirurgie Tetralogy of Fallot (TOF) Palliation H. Taussig A. Blalock Baltimore, 1944, classic Blalock-Taussig Shunt = „blue baby operation“ Modified BT shunt, 1976 Klinik für Kinderherzchirurgie Tetralogy of Fallot (TOF) Right Ventricular Outflow Tract Obstruction (RVOTO): - Suprapulmonary (Pulmonary Arteries) - Pulmonary Valve - Subpulmonary (Right Ventricle) Central Importance of the Pulmonary Valve distally: Pulmonary Artery growth proximally: protect the Right Ventricle Klinik für Kinderherzchirurgie Tetralogy of Fallot (TOF): complete repair C.W. Lillehei, Minneapolis 1955: Fallot correction Klinik für Kinderherzchirurgie Tetralogy of Fallot (TOF) Klinik für Kinderherzchirurgie Tetralogy of Fallot (TOF): results Mortality 3-5 % Heart Block < 3%, seldom requires a pacemaker Post-operative arrhythmia frequent Reoperations required for: • residual VSD (seldom) • residual pulmonary valve insufficiency • residual right outflow obstruction Klinik für Kinderherzchirurgie Tetralogy of Fallot (TOF): reoperations • residual pulmonary valve INSUFFICIENCY right ventricular volume overload + dilatation + failure arrhythmia better growth of pulmonary arteries? late REOPERATION • residual right outflow STENOSIS right ventricular pressure overload pulmonary artery stenosis/hypoplasia late REOPERATION