Thrombocytopenia - Jacobi Medical Center
advertisement
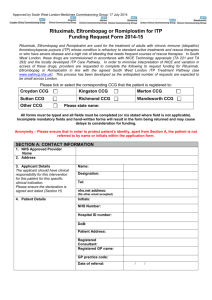
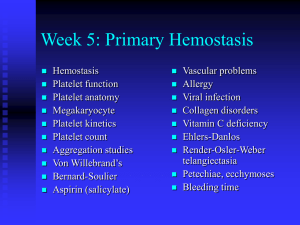
ADVANCES IN THE DIAGNOSIS AND TREATMENT OF THROMBOCYTOPENIA Petechiae Remove Antigen: Rx Inciting Agent = Fix “ITP” HIV Hepatitis C Helicobacter pylori WHEN TO DO A BONE MARROW IN THE THROMBOCYTOPENIC PATIENT? ITP: A SIMPLE DISEASE • Patients make auto-antibodies directed against their own platelets • These platelets are rapidly destroyed • If the platelet count becomes low enough, bleeding symptoms may ensue • Bleeding is rarely serious, ie an intracranial hemorrhage, even at very low counts ITP: A COMPLICATED DISEASE • Anti-platelet antibodies have not been able to be measured discriminatively: the diagnosis and prognosis (outcome, risk of bleeding) remain insecure • Patients may not make platelets well • Treatment is uncertain: who needs it, what to treat with and in which order Pathophysiology of ITP Implications for Diagnosis and Treatment Effect on the Platelet Count of Plasma : ITP into Normal Disease incidence (thousands) 1000 800 600 400 200 1 2 3 Hours 1 2 Harrington WJ, et al. J. Lab Clin Med. 1951;38:1-10. 3 4 5 Days 6 7 8 9 ITP: what tests are helpful • • • • • • Complete CBC---not just the platelets Bone marrow---not in all/most cases Blood type & DAT-prognostic re hemolysis PT-PTT, Thyroid, Ig’s, lupus, SMA Anti-phospholipid antibodies Platelet turnover (estimates): platelet retics, thrombopoietin, large platelets Who Needs Treatment with ITP? At What Platelet Count ? Needs to be individualized: job physical trauma ie sports access to care anxiety effect on fatigue Acute Platelet Increase • gold standard: IVIG at 1 gm/kg • IV anti-D: as fast as IVIG at 75 mcg/kg • Steroids: IV solumedrol 30/kg, high dose dexamethasone or Prednisone 2-4/kg • Platelet transfusions • Combinations including Steroids, IVIG, IV anti-D and/or vincristine Advantages and Disadvantages of Treatment for Children with ITP Advantages Disadvantages • Steroids: oral, continuous so much toxicity often works with any usage • IVIG: rapid substantial blood product, platelet increase headache, 4-6hrs • IV anti-D: 5-15 minute, at fever-chill, hemo75 mcg/kg=IVIG lysis, IVH, blood STUDY TREATMENTS ARM - A D D D D days 1 2 3 4 7 14 21 28 ARM - B RTX D D D D RTX RTX RTX days 1 2 3 4 7 D: 14 21 28 Dexamethasone 40 mg po daily x 4 RTX: Rituximab 375 mg/m2 IV x 4 ML18542 study Clinica Ematologica-Udine SPLENECTOMY CONCLUSION: ITP IN CHILDHOOD • Treatment is indicated for those at risk of (serious) bleeding • Choice of treatment needs to be appropriate for the goal: acute vs cure • New treatments will revolutionize care • Understanding of pt pathophysiology may allow individualization of care GUIDELINES FOR PLATELET TRANSFUSIONS “SAVE ‘EM TIL YOU REALLY NEED ‘EM” NEVER TRANSFUSE A NUMBER. ALWAYS TRANSFUSE A PATIENT! Platelet Production Is Suboptimal in ITP Patients Autoantibodies inhibit Mk growth and promote apoptosis (Chang, McMillan) Autologous 111In-platelet studies show platelet production < normal in 2/3 pts---same results with absolute platelet retics TPO levels normal in 75% of ITP patients (relative TPO deficiency) Damaged or Dysfunctional Mk in marrow (Houwerijl) Pathophysiology of ITP Macrophage P Thrombopoietin P Peripheral blood P Bone marrow P Platelet Megakaryocyte TPO Agonists in Thrombocytopenic States: Focus on ITP Newer agents that will probably revolutionize our approach to thrombocytopenia in many conditions, not only ITP rhTPO and PEG-rHUMGDF rhTPO PEG-rHuMGDF • Glycosylated • Full length • Not glycosylated • Truncated • Additional polyethylene glycol moiety COOH terminal domain Polyethylene glycol NH2 Mpl-binding domain COOH NH2 Mpl-binding domain Kuter DJ, Begley CG, Blood 2002;100:3457. Why Are We Not Using the 1st Generation Thrombopoietins? Initial use of MGDF (and also rhuTPO) resulted in the development of antibodies to exogenous (administered) 1st generation TPO’s that cross-reacted with endogenous TPO (native eTPO): a number of multiply-dosed recipients developed a lasting thrombocytopenia. AMG 531 Fc Carrier Domain • • • • Unique platform “peptibody” Made in E. coli Molecular weight = 60,000 D 4 Mpl binding sites TPO Agonist Peptides • No sequence homology with TPO • Cleared endothelial FcRn Recycled • Cleared RES Bussel JB et al. N Engl J Med. 2006;355:1672. Romiplostim: 38% Durable Response, 79% Overall Response Placebo Romiplostim 60 38.1 40 20 0 0.0 (P = 0.0013) Overall Response 78.6 80 60 40 20 0 0.0 (P < 0.0001) 20 Mean (SE) Number of Weeks With Platelet Response 80 100 Overall Platelet Response (%) Durable Platelet Response (%) 100 Durable Response Number of Weeks Platelet Response 15 12.3 (1.2) 10 5 0.2 (0.1) 0 (P < 0.0001) Platelet response: platelet count ≥ 50 x 109/L Durable platelet response: platelet response for ≥ 6 weeks of final 8 weeks, in the absence of rescue medications during 24 week trial Overall response: either durable or transient platelet response (≥ 4 weekly platelet responses) Error bars represent standard deviation of the mean Romiplostim (AMG 531): Summary In splenectomized patients: • 38% durable response, 79% overall response • Increased and maintained platelet counts over 24 weeks • Significantly decreased the use of rescue medications • All romiplostim patients discontinued or reduced concurrent ITP therapy (corticosteroids, azathioprine, danazol) • Romiplostim appeared to be well tolerated Romiplostim: Summary of Long-term Dosing Efficacy Data Summary • The majority of patients achieved long-term platelet counts > 50 x 109/L and double the baseline value – Mean platelet count maintained between 50 and 250 x 109/L over 2 years • Use of concomitant and rescue medications was substantially reduced over time • No trend in this study for adverse events to increase in frequency with longer drug exposure • One patient had neutralizing antibodies to AMG 531; negative on retesting Eltrombopag: Oral Platelet Growth Factor Small molecule, non-peptide thrombopoietin receptor (TPO-R) agonist Does not compete with TPO for binding to TPO-R Low immunogenic potential Active only in humans, chimps Stimulates megakaryocyte proliferation and differentiation Orally bioavailable Increases platelet counts in normal volunteers Thrombopoietin MW 64,000 Eltrombopag MW 442 Primary Endpoint: Percentage of Patients With Platelets ≥50,000/µL at Day 43 Visit† 100 Responders (%) 80 P <0.001‡ OR = 9.61 (3.31, 27.86) 60 40 20 0 Placebo§ †Last Eltrombopag observation carried forward. significance at 5% (2-sided) level of significance. §1 patient received IVIg on Day 1. Logistic regression analysis adjusted for randomization stratification variables. ‡Indicates Median Platelet Counts (25th and 75th Percentiles) Baseline to Week 20 350 300 Platelet count (Gi/L) 250 200 150 100 50 0 Baseline 1 2 3 4 5 6 7 8 9 11 12 13 14 15 16 17 18 19 20 65 60 51 55 48 39 43 42 39 33 Week Number of subjects: 107 106 106 99 10 97 92 90 83 76 67 62 Splenectomized pts respond as well as non-splenectomized pts Conclusions • The EXTEND data suggest that oral eltrombopag was well tolerated and safe • Eltrombopag up to 75 mg/day increased and sustained platelet counts >50,000/μL in the majority of patients • Eltrombopag reduced the incidence and severity of bleeding HCV Phase II Study Median Platelet Count 250 Placebo 30 mg 50 mg 75 mg 200 150 100 50 INITIATION MAINTENANCE 0 0 14 McHutchison, NEJM 2007 28 42 56 70 Study Day 84 98 112